INTRODUCTION
Brachioradial pruritus (BRP) is a localized neuropathic dysesthesia of the upper extremities.1 The typical presentation is a middle-aged white female with signs of erythema on the dorsolateral upper extremity(ies) that has intense pruritus.2 The most accepted causative factor of BRP is cervical radiculopathy with excessive ultraviolet radiation (UVR) exposure.3–5 The typical treatment consists of UVR avoidance, topical medications such as capsaicin or mild steroids, and oral medication such as gabapentin.6,7 Research on treating the underlying cervical lesion leading to the symptoms of BRP is lacking. Only 1 case study is available on the effective treatment of BRP through chiropractic intervention.8 This paper describes the successful resolution of medication-resistant BRP in a 42-year-old woman treated with Orthospinology Upper cervical chiropractic adjusting of the craniocervical junction (CCJ) and Pierce Technique spinal adjusting of the C5 vertebra.
The Orthospinology upper cervical method aims to improve the structural alignment of the craniocervical junction (CCJ), thus restoring the neurological integrity of the surrounding anatomy.9 The CCJ comprises the base of the occiput to the C2 vertebra. This includes the occipitoatlantal and atlantoaxial joints. The spinal unit is highly mobile, but at the cost of stability. An injury to the CCJ can displace the alignment of the joint surfaces. Grostic’s Dentate Ligament Theory suggests that a displaced CCJ may cause inappropriate indirect mechanical tension on the transition between the brain stem and the spinal cord, leading to nerve distress.10
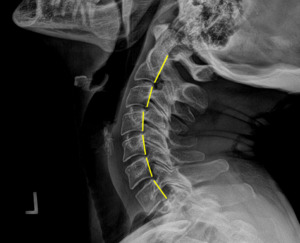
To correct the alignment of the CCJ using the Orthospinology upper cervical method, a handheld instrument applies a force <3lbs to the transverse process of C1 at a vectored angle based on x-ray measurements to reduce the malpositioning. (Figure 1) We discuss this intervention further, along with the Pierce Technique high-velocity, low-amplitude (HVLA) procedure below.
CASE REPORT
A 42-year-old athletic female sought care for a 3-year history of intense itching and erythema of the right upper arm and neck stiffness. She stated that the symptoms began when she was on vacation in the American desert southwest. She remembers having her right arm resting on the car window attaining sun exposure when the pruritus initiated. Her neck stiffness started this vacation as well. Upon returning home, her primary-care physician prescribed her a short trial of prednisone and ordered a cervical MRI, which showed mild degenerative changes in her mid-cervical spine. The prednisone improved the pruritus and the neck stiffness for a few weeks. However, her condition again flared, causing her to seek a dermatologist evaluation. She was seen by 2 dermatologists, receiving simultaneous agreement of a BRP diagnosis. She was given two different ointments, gabapentin, and eventually an antihistamine, all of which failed help. She was then treated with physical therapy and acupuncture, both failing to achieve permanent results. (Informed consent to publish the patient’s case findings was discussed verbally and written with her signed form on file. )
Physical And Chiropractic Exam Findings
During the initial chiropractic evaluation, noticeable erythema and scabbing were observed on the patient’s right dorsolateral arm. (Figure 2) She had static postural imperfections such as head tilt, a short right leg in the supine position, forward head posture, and a tilted pelvis when standing. Her musculature surrounding the 1st and 5th cervical vertebrae was taut and painful to palpation. During motion palpation, the C5 vertebra was noted to be restricted in flexion and bilateral rotation. Active and passive global cervical ranges of motion were both restricted and painful. Deep tendon reflexes of the entire right upper chain were absent; the left reflexes were all intact.
X-Ray Findings
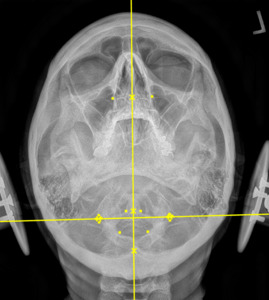
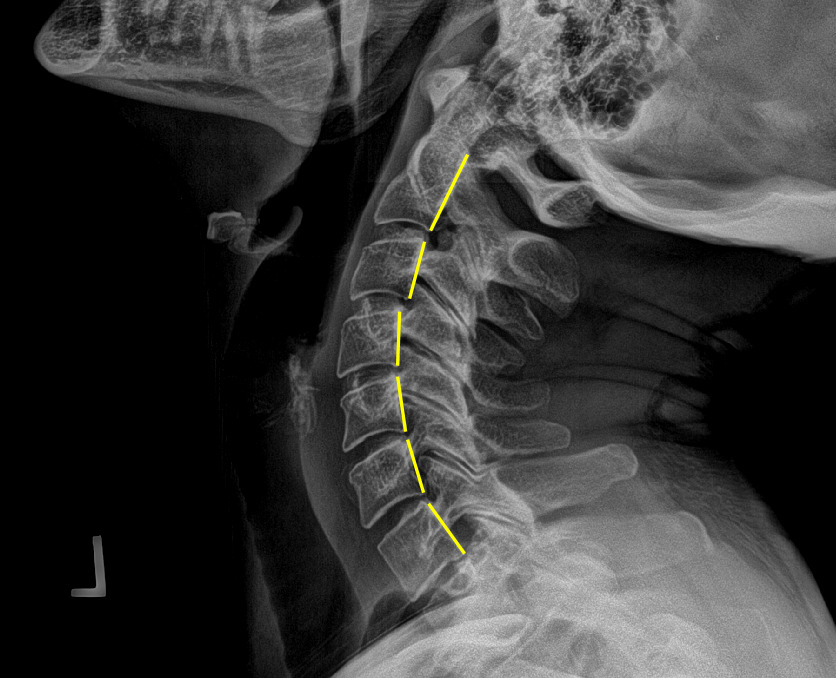
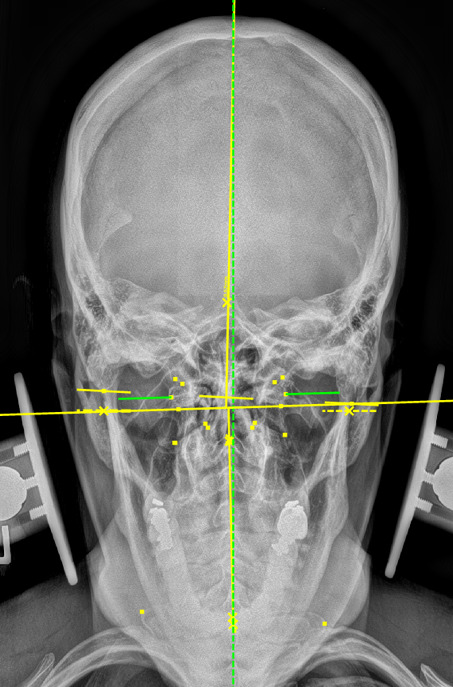
Plain film radiography of the cervical spine showed a grade 1 spondylolisthesis of C4 (Figure 3), mild disc and facet degeneration of C5 (Figure 3), a motion fixation of the C4-C5 vertebrae unit in forward flexion (Figure 4), a retrolisthesis of C3 on extension (Figure 5), and a structural malposition of the craniocervical junction as per Orthospinology measurements. (Figures 6 and 7). Though these are static films and active motion cannot be observed in real-time, motion restriction of the C4-C5 vertebrae unit from neutral to forward flexion position was determined by a lack of spinous separation, a lack of intervertebral foramen expansion, and an absent intersegmental kyphosis of George’s Line.
Treatment Plan
The patient had 12 visits over 3 months. We started twice per week for the first 2 weeks, then reduced to once per week for the following 6 weeks, finishing with once every 2 weeks for the remaining 4 weeks. The planned treatment consisted of Orthospinology upper cervical intervention to the craniocervical junction when indicated, high-velocity low-amplitude manual spinal adjustment to the C5 vertebra on the first visit, and instrument-assisted vibration to the C5 vertebra on all subsequent visits.
We chose to apply spinal adjusting to the C5 vertebra using the Pierce Technique method. To describe the process, I used my hypothenar eminence to contact the spinous process of C5 while the patient was in the prone position. Then, I applied a high-velocity low-amplitude vectored force in the direction of posteroinferior to anterosuperior along the apophyseal joint angles. On the subsequent visits, I used a computerized instrument-assisted tool to apply light force and vibration to the C5 joint surfaces in the same posteroinferior to anterosuperior direction.
Patient Outcome
After the initial treatment, the patient’s pruritus and erythema increased (Figure 8); however, her neck stiffness improved substantially as noted subjectively and by active and passive range of motion. By the 3rd visit, she noted that the pruritus and erythema were beginning to move proximally up her arm, from the mid-forearm to just proximal to the elbow. After 1 week since her initial treatment, her erythema had resolved and the pruritis had substantially improved. (Figure 9) After 30 days, the pruritus had resolved, and the scabbing had begun to heal. (Figure 10) After 60 days, besides faint permanent scarring, she returned to pre-condition status. (Figure 11) She remains in pre-condition status nearly 2 years after her initial treatment. She did not receive any other forms of treatment for her BRP from other providers during the chiropractic care.
DISCUSSION
This case study documents the resolution of BRP in a 42-year-old female who previously failed many treatments. The clinician treated the underlying cervical lesions, in an attempt to achieve long-term healing of the symptoms.
RATIONALE FOR ADJUSTING PROCEDURES
Orthospinology Upper Cervical
As stated above, Orthospinology upper cervical adjusting was used “when indicated,” during the plan of care. This upper cervical chiropractic method is based on the idea that the CCJ is either structurally aligned and allowing for neurological harmony, or misaligned and causing neurological dysfunction. Though direct neurological function was not measured in this case, the Orthospinology procedure uses indirect measures to evaluate neurological function as it relates to the craniocervical junction. Grostic researched the anatomical bridge of the dentate ligaments from the C1 vertebra to the dura mater of the spinal cord. A misalignment of C1 thus can affect nerve function through mechanical tension and irritation of the spinal cord. The dorsal spinocerebellar tract (DSCT) is theorized to be the first affected by a C1 misalignment due to its lateral location within the spinal cord. Inappropriate nerve signals from the DSCT may lead to a reflexive change in peripheral muscle tone, affecting posture. Therefore, postural evaluations are conducted to assess for these changes in the Orthospinology Upper cervical procedure.10–12
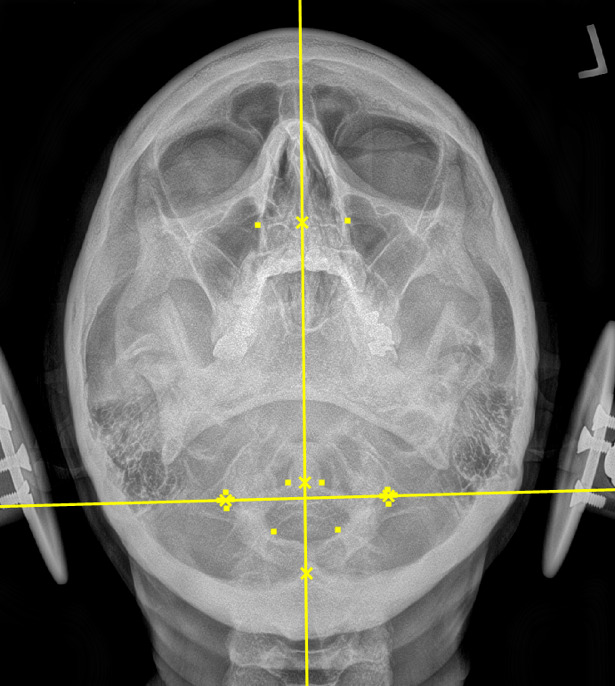
During the initial examination, the chiropractor evaluates the patient’s postural findings, including standing head tilt, head rotation, shoulder height comparison, hip height comparison, lower neck deviation, and supine leg-length inequality. The chiropractor will then take 3 radiographic images of the CCJ minimum to view the alignment in a projected 3-dimension. These images are the cervical neutral lateral (sagittal plane), the nasium (frontal plane), and the vertex (transverse plane). A series of measurements are graphed on the radiographs to assess for alignment. Then, the Orthospinology upper cervical procedure provides a calculation and vectored angle based on these measurements to reduce the misalignment. The chiropractor will use this angle to administer the adjustment to the CCJ. Immediately after the adjustment, the chiropractor evaluates the postural findings for correction. If it has improved, the chiropractor repeats the nasium and vertex views to observe for structural correction. If the postural findings do not improve, the chiropractor may administer a subsequent adjustment before the post-imaging is taken.12
Since the philosophy of the Orthospinology upper cervical procedure is that the CCJ is either structurally aligned and allowing for neurological harmony, or misaligned causing neurological dysfunction, the concept of holding the alignment must be discussed. After the adjustment, the patient is in alignment until a stressor causes a subsequent misalignment. It has been observed that when patients present with a subsequent misalignment, it is typically measured identically to their initial presenting misalignment. This is believed to occur due to individual anatomical variations and weaker ligaments in the direction of the misalignment from the injury that caused the initial misalignment. This also allows for the chiropractor to repeat the adjustment at the same measured angles as the initial adjustment without having to repeat imaging every time the patient presents with the physical findings of a misalignment. The patient in this case study presented with the need for a craniocervical junction adjustment on visits 1, 3, 4, and 10.13
Pierce Results HVLA and Instrument Adjusting
As stated in the case study section, the patient was only treated on the initial visit with the Pierce HVLA adjustment to the C5 vertebra, and on all subsequent visits, C5 was treated with an instrument. After the initial HVLA, the motion, palpatory, and pain findings resolved and ceased to return during the entire plan of care; thus, a subsequent HVLA was not indicated. The practitioner continued to treat the C5 spinal segment with light-force instrument adjusting on subsequent visits for proprioceptive input without taking the joint into its paraphysiological space. When a joint is injured and fixated, proprioceptive afferentation becomes dysfunctional. Applying light force and vibration to the joint will stimulate the Pacinian receptors, putting neurological input through pathways that were previously underworked and receiving faulty information from the fixated joint.13–15 Applying neurological input to an underworked or injured pathway may provide healing through neuroplasticity.16
Other Case Reports
Though research on treating the cervical spine in BRP patients is lacking, 1 retrospective case series of 3 examined the outcomes using CT-guided cervical nerve root block. All 3 patients had positive cervical spine lesions and failed oral and topical medications. The nerve root block substantially reduced the patients’ BRP symptoms.17 This nerve root block study did not use manual means as its intervention, as we did here; however, it still showed positive results with BRP after doing some form of intervention to the cervical spine.
CONCLUSION
Though this case study is limited to a single patient, it suggests that conservative chiropractic management of the cervical spine may provide benefit to the BRP patient. By treating the underlying cervical lesions, the patient was able to receive a successful, long-term result. Further research should examine the management of the cervical spine in BRP outcomes and evaluate for direct causative links between cervical lesions and BRP. This case study may serve as a reminder to always consider the anatomical generators of every patient’s condition.