INTRODUCTION
Background
Lumbar spinal disc injury is a prevalent, disabling, and costly condition plaguing millions of people of many different backgrounds and occupations.1 The lumbar spinal disc can be injured by autoimmune, infection, and metastatic processes; however, degeneration and physical trauma account for the majority of pathophysiological mechanisms.1 The spinal disc contains two anatomically relevant structures as related to injury. The annulus fibrosis (AF) as the outer surface, and the nucleus pulposis (NP) as the inner layer. The spinal disc can be described as a “jelly doughnut” where the outer bread resembles the AF, and the internal jelly resembles the NP. The degenerated and traumatically injured disc presents as two categories and four total possibilities.2 Table 1 discusses these presentations.
The most common way a lumbar spinal disc can endure a herniation is when a degenerated predisposed segment undergoes flexion with rotation while under a load; for example, when a patient bends forward at the waist and reaches to the side while picking up a heavy package.
Epidemiology
Epidemiology studies on lumbar disc herniations (LDH) very considerably and have conflicting results due to many cases achieving pre-injury pain and disability status spontaneously.3 A patient can have radiographic evidence of LDH and be asymptomatic, creating a diagnostic challenge and complicating research. Saying this, the most common symptom of LDH is low back pain (LBP). Non-differentiated LBP has been studied and documented well. Therefore, we will discuss LBP epidemiology. Most sources list that roughly 65%-80% of the population will experience at least one episode LBP in their lifetime.4 LBP is the second most common cause of disability in the United States.5 LBP costs the United States up to $200 Billion annually, directly and indirectly.6 A staggering 149 million work days are missed due to LBP per year.7 Comparatively, LBP accounted for 13-17% of all sickness-absence in the Norwegian health system. 16% of those persons missed work for more than seven weeks.8
Treatment Options
Treatment for disc herniations very considerably and depend heavily on the provider type from whom the patient seeks care.1 Treatments range from watch-and-wait all the way up to aggressive surgery. As with any health malady, benefits, risk, cost, and patient values should be considered with disc herniation treatment. Additional factors such as patient demographics, presence of neurological deficit, and disruption of daily activities should be used to guide treatment recommendations. This paper documents and describes the successful functional outcomes and reduction in disc extrusion size visible on pre-post MRI following a comprehensive plan of chiropractic care.
CASE REPORT
History
A 60-year-old male sought care for left lumbar and left anterior knee pain that began 2 months prior. The pain was insidious, gradual, worsening, constant, and rated 9/10 at its worst. The patient is a mechanic and had a similar pain pattern 15 years prior.
Examination
The patient had a noticeable antalgic lean to the right. The lumbar paraspinals and gluteal muscles had global tenderness and spasm. Intersegmental tenderness and motion restrictions were noted at L4, L5, and bilateral sacroiliac joints. Kemp’s test elicited pain bilaterally around the base of the spine. Bechterew’s test elicited radiating pain while testing the left leg. The patient underwent functional testing such as single-leg squat and heel-toe walking. He was unable to perform either test on the left leg. His right leg was unaffected, and testing was normal.
Imaging Findings
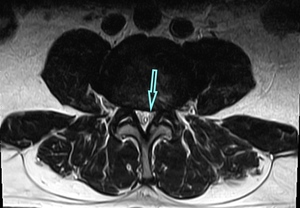
We therefore believed that LDH with nerve root compression was present; therefore, an MRI was obtained. The following are the significant findings. Sagittal left paracentral T2 image and axial T2 images at the L3-4 disc level (Figure 1) and just caudal to the disc level (Figure 2) reveal a large left paracentral/subarticular extruded herniation that measures 10mm AP with 19mm of caudal migration resulting in marked left L3-4 lateral recess stenosis and compression of the traversing L4 nerve root and moderate central spinal canal stenosis. (Figure 3) shows the left paracentral lumbar sagittal view.
Treatment Plan
Our case was treated with spinal manipulation therapy (chiropractic adjustment), including instrument-assisted adjusting and drop table, electrical muscle stimulation therapy (EMS), mechanical massage commonly referred to as a “chiropractic roller table”, and at-home exercises. The physiological mechanisms of these modalities used are expanded upon in the discussion section of this paper. Our paper follows the recommendations seen in “Lumbar Disc Nomenclature: Version 2.0: Recommendations of the Combined Task Force of the North American Spine Society, The American Society of Spine Radiology, and the American Society of Neuroradiology.”9
The recommended comprehensive plan of chiropractic care included spinal manipulation to the thoracic, lumbar, and pelvic regions of the spine using a handheld adjusting instrument and drop table techniques. Though the segments of herniation were within the lumbopelvic region, thoracic spinal manipulation was included to improve global spinal biomechanics. Mobilizing the adjacent spinal region (thoracic) aids in the stabilization of the lumbopelvic region.10 It also included EMS applied to the lumbar paraspinals for eight minutes and full spine mechanical massage applied for 8 minutes per session. At-home recommendations consisted of McKenzie exercises, heel walking, and lower extremity flexor stretching. The frequency and duration included two in-office visits per week until there was subjective improvement, such as reported pain reductions and objective improvement to include functional testing improvement, improved palpatory findings, and negative orthopedic tests that were previously positive.
Patient Outcome
During care, the patient had many ups and downs. The first noticeable improvement was on visit number 14, 7 weeks from the initial examination, when he reported pain improvement from a 9/10 to a 4/10 and improved toe walking. After the 24th visit during the 12th week, his condition had lasting result. His subjective pain decreased from an initial 9/10 to a 3/10, all previously positive orthopedic tests were negative, palpatory findings decreased, and the patient could now perform heel walking without issue. His frequency was dropped to once per week and was seen 11 more times over the next 12 weeks to maintain results. After the 35th total visit and 6-months had passed, a repeat MRI was performed with the following findings of significant improvement. Sagittal left paracentral T2 image and axial T2 images at (Figure 4) and just caudal (Figure 5) to the L3-4 level corresponding to the initial images reveal significant regression of the previously diagnosed disc extrusion with no history of surgery. (Figure 6) shows the left paracentral lumbar sagittal view post-treatment. This disc herniation reduced to 4.7mm AP with 12mm of caudal migration resulting in less severe L4 nerve root impingement and more mild central spinal canal stenosis.
DISCUSSION
Similar Case Reports
We found 13 case studies where the clinical symptoms of LDH improved with spinal manipulation.11–24 Of these publications, 3 obtained post-imaging.11,21,24 And of these publications, 2 showed a measurable reduction of the herniation.11,24 The first case study11 demonstrated the reduction of a disc herniation clinically presenting as orchialgia using spinal manipulation and adjunct therapies to treat. The paper does not mention the herniation measurement; however, it was just large enough for indentation of the thecal sac. The post image showed regression of the previous thecal sac displacement. The second report24 demonstrated an 11mm extrusion that was completely resorbed at a 13-month follow up MRI. The patient received 4-weeks of chiropractic care to include spinal manipulation. He had no neurological or functional deficit, and his only complaint was pain. The clinical improvement in function plus the significant reduction of the massive extrusion in our case makes our case unique among the existing literature.
Treatment Methods Discussion
Professional Guidance for LDH Management
Both The North American Spine Society (NASS) and The Japanese Society for Spine Surgery and Related Research (JSSSRR) have published papers and guidelines on care for LDH. NASS25 has published an extensive review, but we have summarized the findings as relevant to our case: Many, but not all, papers have demonstrated a clinical improvement with decreased size of disc herniation. In the absence of reliable evidence, it is the work group’s opinion that a limited course of structured exercise is an option for patients with mild to moderate symptoms from lumbar disc herniation with radiculopathy. Spinal manipulation is an option for symptomatic relief in patients with lumbar disc herniation with radiculopathy. There is insufficient evidence to make a recommendation for or against the use of spinal manipulation to improve functional outcomes in patients with lumbar disc herniation with radiculopathy. There is insufficient evidence to make a recommendation for or against the use of spinal manipulation as an alternative to discectomy in patients with lumbar disc herniation with radiculopathy whose symptoms warrant surgery. Surgical intervention prior to 6 months is suggested in patients with symptomatic lumbar disc herniation whose symptoms are severe enough to warrant surgery.
JSSSRR26 published the following summary as relevant to our case: Conservative treatment is chosen initially out of principle. Surgery should be offered if conservative treatment fails. Prompt surgery should be chosen for cases with severe neurological deficit or cauda equina syndrome.
Author’s Comments on the Above NASS and JSSSRR Guidance
Neither guideline discusses herniation size as a factor of management.
Spinal Manipulation for LDH management.
Santilli et al27 produce a randomized controlled trial (RCT) on spinal manipulation for acute back pain and sciatica with disc protrusion. Their findings showed significance for pain reduction. Burton et al28 produced an RCT on spinal manipulation versus chemonucleolysis for patients with sciatica due to confirmed lumbar disc herniation. Both groups had significant improvements. The authors concluded that manipulation is a safe and effective treatment option for patients with lumbar radicular syndrome due to lumbar disc herniation, in the absence of clear indications for surgical intervention. McMorland et al29 studied the clinical efficacy of spinal manipulation versus microdiscectomy in patients with sciatica secondary to lumbar disc herniation. The authors concluded that of patients with sciatica that fail 3 months of medical management, 60% will benefit from spinal manipulation to the same degree as if they undergo surgical intervention. A 2018 systematic review found spinal manipulation to have a higher effective rate in LDH compared to acupuncture or lumbar traction.30 A retrospective study of United States healthcare records found spinal manipulation when used at newly diagnosed LDH reduced the odds of lumbar discectomy.31
Hypothesis
We hypothesize that the spinal manipulation treatment aided in a certain degree of the objectively viewed disc resorption through the following mechanisms. Firstly, spinal manipulation increases apophyseal (facet) joint range of motion.32,33 The increased motion allows for greater resorption of extracellular fluid. Second, the spinal manipulation may have modulated the production of inflammatory components, leading to both a direct and indirect aid to resorption.34 Further research is needed to effectively test these hypotheses.
CONCLUSION
This paper documents the successful MRI-shown evidence of a massive LDH extrusion reducing in size following a comprehensive plan of chiropractic care. The patient achieved clinical improvement with his function and symptoms as well. Because there is a natural history toward resorption regardless of conservative treatment choice, and this being a singular case, we are not suggesting that the treatment outlined resulted in the resorption.25,35 However, our case shows that not all large LDHs require surgery, and that chiropractic care is not contraindicated.
The clinical import of our paper suggessts that disc extrusion size is not a factor when determining treatment and that chiropractic care to include spinal manipulation is not contraindicated.
AUTHORS’ CONTRIBUTIONS
CR was the treating clinician and gathered the data.
TS consolidated the data, performed the literature review, and prepared the manuscript.
SF prepared the radiology reports.





_post-tx_(right)_left_paracentral_sagittal_view_of_lumbar_spine_for_comparison.png)






_post-tx_(right)_left_paracentral_sagittal_view_of_lumbar_spine_for_comparison.png)