INTRODUCTION
Thoracic Outlet Syndrome (TOS) is a condition characterized by compression of the brachial plexus and/or subclavian vessels as they pass through the thoracic outlet. It can be classified into neurogenic, venous, and arterial subtypes, with neurogenic TOS (nTOS) accounting for approximately 90% of cases. The etiology of TOS includes congenital anomalies (such as cervical ribs), trauma, repetitive stress injuries, and postural abnormalities. Surgical intervention, including first rib resection, is considered when conservative management fails to relieve symptoms.
Chiropractic care, including low-force spinal adjustments and McKenzie cervical retraction exercises, played a valuable role in symptom management and care coordination in this case. However, the persistence of symptoms despite conservative treatment emphasized the importance of diagnostic imaging and interdisciplinary referral. This case illustrates the collaborative role chiropractic providers can play in identifying structural causes of TOS and supporting optimal surgical outcomes.
Treatment of TOS varies depending on the subtype and severity. Conservative management is the first-line approach and may include physical therapy, posture correction, chiropractic care, and activity modification.1–3 When symptoms persist despite conservative care, surgical options such as first rib resection and scalenectomy may be indicated. Surgical outcomes are generally favorable but may be complicated by incomplete resection or scar tissue formation.4
Thoracic Outlet Syndrome (TOS) is a neurovascular condition involving compression of the brachial plexus and/or subclavian vessels as they pass through the thoracic outlet. TOS can be categorized into neurogenic, venous, and arterial types, with neurogenic TOS (nTOS) accounting for over 90% of cases.1 The condition may arise from anatomical anomalies, such as cervical ribs or fibrous bands, postural dysfunction, repetitive trauma, or post-surgical changes.2 Symptoms often include pain, paresthesia, weakness, and vascular changes in the upper extremity. Diagnosis is primarily clinical but may be supplemented by imaging and electrodiagnostic studies.
Case Report
Patient Information: A 30-year-old male hadprogressive neck pain and upper extremity symptoms that had persisted for over 5 years. His symptoms included numbness, tingling, shooting pain, and a squeezing sensation in the left upper extremity, rated at 6/10 in severity. He reported worsening symptoms in the past several months, exacerbated by overhead activities, prolonged sitting, driving, and certain sleeping positions.
The patient’s medical history was significant for bilateral first rib resections in 2019, which provided right-sided symptom resolution and only partial relief on his left side. He had undergone physical therapy, nerve blocks, and medication management with minimal improvement. Cervical arthritis was suspected based on previous imaging.
Clinical Examination: On evaluation, his symptoms were exacerbated by upright posture and improved with slouching, suggesting a postural component to his discomfort. Cervical range of motion was notably limited, with painful extension restricted to 20 degrees and left rotation to 45 degrees. Orthopedic testing revealed a positive cervical compression test and a positive Wright’s test on the left side, consistent with neurovascular compression typical of thoracic outlet syndrome. Palpation elicited marked tenderness in the left intrascapular region and mid-cervical spine, accompanied by taut paraspinal musculature. Functional assessment using the Oswestry Disability Index (ODI) indicated moderate to severe impairment, with a score falling between 41–60%.
He reported left upper extremity symptoms including numbness and shooting pain radiating primarily along the C7 and C8 dermatomes. These symptoms were most pronounced during activity, especially overhead movements and prolonged postures such as sitting and driving. At rest, symptoms decreased but were not completely resolved. He rated his pain as 6/10 during activity. Symptoms were also worsened by sleeping in a supine position with the arm overhead, while a fetal position provided temporary relief. He had previously been diagnosed with neurogenic thoracic outlet syndrome, which prompted bilateral first rib resections in 2019. These initial surgeries provided only partial relief.
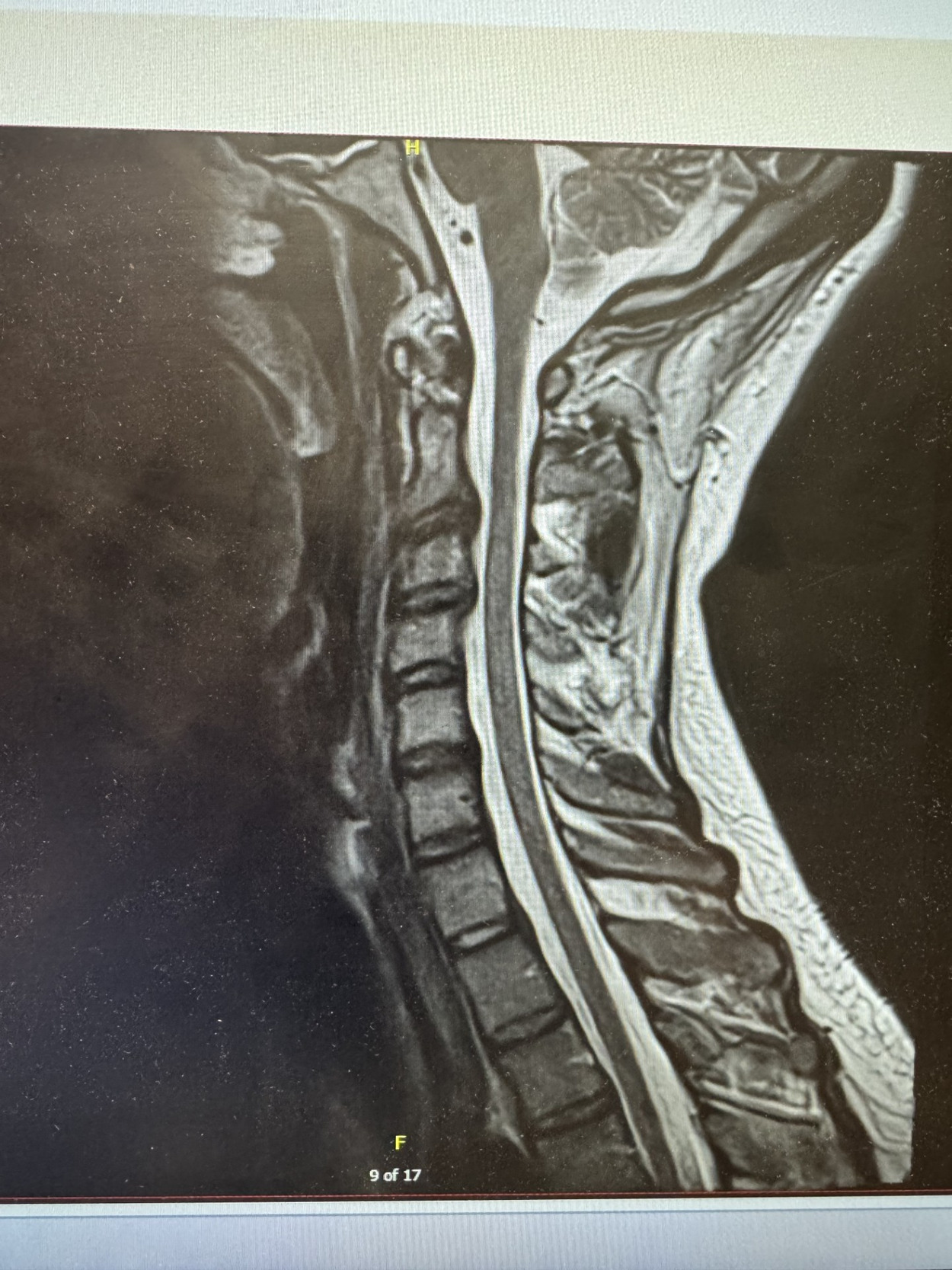
Diagnostic Assessment: Radiographic imaging was instrumental in identifying structural contributors to the patient’s ongoing symptoms. Thoracic X-rays revealed dextroscoliosis at the T5/T6 level, with visible surgical clips at the right T1 rib and a residual segment of the first rib remaining on the left side, suggesting an incomplete prior resection (see Figure 1). Further evaluation with cervical MRI demonstrated mild degenerative changes, including canal stenosis at C3-C4 and mild right neural foraminal stenosis at the same level. Additionally, a disc osteophyte complex was identified at C2-C3, causing effacement of the ventral thecal sac (see Figure 2). Subsequent surgical intervention confirmed the presence of the residual first rib segment on the left, which was successfully excised during the revision procedure (see Figure 3).
Treatment and Intervention: The patient underwent a trial of chiropractic care aimed at reducing neurogenic symptoms and improving cervical function. Treatment included gentle, low-force spinal manipulation targeting the mid-cervical region to address joint dysfunction and reduce biomechanical stress. In addition, McKenzie cervical retraction exercises were prescribed to promote postural correction and alleviate neural tension. Despite some symptomatic relief, the persistence of neurovascular complaints and the findings on diagnostic imaging warranted further investigation. As a result, the patient was referred to a vascular surgeon for comprehensive evaluation and surgical consideration.
Chiropractic evaluation revealed postural asymmetry, limited cervical range of motion, and segmental dysfunction in the mid-cervical spine. Palpation identified joint restriction and muscle hypertonicity at C5-C6. Orthopedic testing revealed positive Wright’s and cervical compression tests on the left side, consistent with neurogenic thoracic outlet syndrome. Based on these findings, treatment included low-force cervical adjustments using both diversified manual technique and the Activator Method. McKenzie cervical retraction exercises were prescribed along with postural correction strategies to reduce neural tension and improve ergonomics. The patient was seen twice weekly for 3 weeks prior to referral. The Oswestry Disability Index (ODI) initially measured 48%, which improved to 28% post-surgery. Following surgical resection of the residual rib segment, chiropractic care was paused for 4 weeks and then resumed once weekly for supportive care. The patient was instructed to perform cervical retractions, consisting of 10 repetitions each 2 hours while awake.
Discussion
This case highlights the critical role of chiropractic evaluation in identifying complex presentations of TOS. Neurogenic TOS (nTOS) accounts for approximately 90% of all TOS cases and remains a diagnostic challenge due to its variable symptomatology.2 While conservative care, including chiropractic management, may provide symptomatic relief, it is crucial to recognize when symptoms persist due to structural anomalies that require surgical correction. Residual rib segments following first rib resection are an uncommon but recognized cause of persistent nTOS symptoms.5 Early recognition and referral for appropriate surgical management can significantly improve patient outcomes.6
This case underscores the importance of a thorough chiropractic assessment in the co-management of complex presentations of thoracic outlet syndrome. Neurogenic TOS is the most common form and can present with a broad range of symptoms, often mimicking other cervical radiculopathies. In this case, imaging played a critical role in identifying a residual rib segment that had been missed during the initial surgical resection. Early identification of this structural contributor allowed for timely surgical referral and resolution of the patient’s symptoms.
Previous literature supports the value of conservative approaches such as physical therapy and chiropractic care in managing TOS symptoms. Case reports have demonstrated success with spinal manipulation and postural exercises in reducing symptoms and improving function, although these are typically effective only in non-structural cases. In contrast, persistent or worsening symptoms may require surgical intervention. This case aligns with similar reports where chiropractic care was instrumental in detecting structural causes and facilitating appropriate referrals.
Imaging remains a crucial component of evaluation, particularly when previous surgical intervention has failed to fully resolve symptoms. In this case, thoracic radiography clearly revealed the residual rib segment, prompting a surgical referral that ultimately resolved the patient’s symptoms. This highlights the need for conservative providers to maintain a high index of suspicion for structural anomalies and to utilize diagnostic imaging accordingly.
Further research is needed to establish standardized diagnostic criteria for post-surgical residual TOS cases and to determine the optimal timing for surgical re-evaluation in patients with recurrent symptoms. Enhanced collaboration between conservative care providers and vascular surgeons may improve early detection and management of residual TOS cases. Previous literature has documented the importance of a multidisciplinary approach in TOS management. While physical therapy, chiropractic care, and medical pain management can address functional impairments, surgical intervention remains the definitive treatment for structural compression. In this case, chiropractic care provided symptomatic relief but also facilitated timely surgical referral, ultimately leading to complete symptom resolution.
Further research is needed to establish standardized diagnostic criteria for post-surgical residual TOS cases and to determine the optimal timing for surgical re-evaluation in patients with recurrent symptoms.
Conclusion
Chiropractic care, including spinal adjustments and therapeutic exercises, can play a role in symptom management for TOS. However, persistent symptoms despite conservative treatment should prompt further diagnostic investigation. This case underscores the importance of a collaborative approach in identifying structural causes of TOS and ensuring timely referral for surgical correction when necessary.
Chiropractic care, including low-force spinal adjustments and McKenzie cervical retraction exercises, played a valuable role in symptom management and care coordination in this case. However, the persistence of symptoms despite conservative treatment emphasized the importance of diagnostic imaging and interdisciplinary referral. This case illustrates the collaborative role chiropractic providers can play in identifying structural causes of TOS and supporting optimal surgical outcomes.