Introduction
Psychosocial factors alongside maladaptive neuroplasticity in response to spinal dysfunction contribute to the development of musculoskeletal pain.1,2 irrespective of pain location, chronicity and/or severity.3–5 These factors continue to impact an individual’s psychological well-being and anxiety levels.,6,7 sleep quality,8,9 and health-related quality of life10–12 following the onset of musculoskeletal pain. The severity of musculoskeletal pain is associated with the co-morbidity of insomnia,13 anxiety, or both.6 It has also been reported that individuals with chronic musculoskeletal pain and anxiety have lower health-related quality of life compared to those without a comorbidity of anxiety.7,10
A previous feasibility study found that individuals with chronic musculoskeletal problems in combination with occipito-atlantal (C0-C1) joint dysfunction(s) had neck-pain related disability, moderate to high anxiety, subthreshold insomnia, along with poor quality of life and generic health status.14 Past work has indicated that high-velocity low amplitude (HVLA) thrusts directed at dysfunctional vertebral spinal regions normalizes sensory feedback and improves central processing,1,15 which may influence pain mechanisms associated with the psychosocial factors (e.g. autonomic arousal, sympathetic nervous system reactivity, and neuroimmune function).16–18 The administration of HVLA manipulation to dysfunctional C0-C1 joint(s)19 in addition to other areas of restricted spinal movement, is known as the One-to-Zero (OTZ) system.14,19 The OTZ system lead to improvements in frozen shoulder syndrome in individuals who had C0-C1 joint dysfunction(s) accompanying their frozen shoulder.19 This system of spinal adjustments is administered until the C0-C1 joint dysfunction no longer requires treatment, which is dependent on the severity of each individual’s symptoms.14,19 After undergoing the OTZ system intervention, individuals with C0-C1 joint dysfunction(s) who experienced unilateral or bilateral chronic musculoskeletal pain and/or reduced shoulder mobility reported no neck disability, low state anxiety, no clinically significant insomnia, and improved perception of their health.14 This was confirmed using validated self-report measures, such as the Neck Disability Index, Beck Anxiety Inventory, Insomnia Severity Index, and 36-item Short Form Health survey.14 The observed changes in self-report measures could not attributed solely to the OTZ system as participants also received adjunct treatments (i.e. physiotherapy) as part of their pragmatic treatment plan. Thus, a cause-effect relationship could not be confirmed with that study design, revealing the need to conduct a randomized control design, to confirm findings.
The objectives of this pragmatic randomized control trial were to determine the effectiveness of the OTZ system on pain-related disability, anxiety, severity of insomnia, and generic functional health status (assessed via validated questionnaires) compared to a wait list control group (2-week control period) in those with a chronic musculoskeletal pain who also presented with C0-C1 joint dysfunction(s). It was hypothesized that the treatment group would exhibit improvements in outcomes that were impaired to begin with, while the control group would show little to no change following a 2-week wait period.
Methods
This pragmatic randomized control trial used a parallel group trial design with a 1:1 allocation ratio.
Power Calculation – Required Sample Size
A priori power analysis for a 2 x 2 repeated measures within-between interaction was performed in G*Power 3.1.9.7 software.20 With a medium effect size (f = 0.23; calculated using Cohen’s d acquired from previous study (14)), alpha of 0.05, a power of 0.90 (set high to minimize the chance of a type II error), and correlation among repeated measures of 0.5, a sample size of 52 (26 participants/group) would be needed. Sixty-two to Sixty-four participants were recruited, to allow for dropouts.
Criteria
Participants aged 18 to 65 experiencing reduced unilateral or bilateral shoulder mobility,19 and persistent unilateral and/or bilateral musculoskeletal problems14 were screened by a chiropractor at a private practice to affirm the presence of occipito-atlantal joint dysfunction(s). Joint dysfunction is characterized by joint tenderness upon palpation, restricted intersegmental motion, asymmetrical muscle tension between vertebrae, and abnormalities or blocked joint play and end-feel.21 The treating chiropractor performed a skull glide along the orientation of the occipital condyles to confirm restricted intersegmental motion at the occipito-atlantal joint complex.19 Participants who informed the treating chiropractor that they received treatment in the past month, and had recent neurological problems, and/or contraindications to spinal manipulation (e.g. inflammatory conditions or rheumatoid arthritis, fracture or dislocation to the shoulder or spine, recent head trauma or injury or stroke, uncontrolled hypertension, cancer, infection or systemic disease related to neck pain, bleeding disorders, individuals on anticoagulant medications, etc.) were ineligible for the study. The chiropractor confirmed the presence of residual neurological symptoms and/or contraindications to spinal manipulation via additional history questions and/or tests assessing sensorimotor impairments.
Participants
Sixty-three participants (42.56 ± 13.88 years of age) were deemed eligible by the chiropractor. The treating clinician informed the student researcher who then obtained online informed consent after enrolling into the pragmatic randomized control trial via email and before completing the self-report measures online by clicking “I agree to participate”.
This study was approved and conducted in accordance with the Ontario Tech University Research Ethics Board (File No: 15908). This pragmatic randomized control trial was prospectively registered with the Australian New Zealand Clinical Trials Registry (Trial ID: ACTRN12621001191886). The reporting of this randomized control trial (RCT) adhered to the 2010 version of the Consolidated Standards of Reporting Trials (CONSORT) statement, and the CONSORT Patient-Reported Outcome (PRO) extension.
Randomization & Allocation
A simple randomization method was employed. The random allocation sequence, with an equal number of participants assigned to control and treatment groups, was generated using the random function in Excel. This sequence was prepared by the lead researcher, who was initially blinded to the group assignment. The group assignments were placed into sealed, sequentially numbered opaque envelopes. Within 72-hours of completing the self-report outcome measures (after confirmation of study eligibility by the chiropractor and study enrollment), participants were assigned to either the treatment or control group. This was performed by the student researcher who selected the envelope in sequential order and informed participants of their group assignment. At that point, the lead researcher was unblinded to the group assignments to allow for timely distribution of questionnaires at follow-up, i.e. after treatment or two-week wait period.
Experimental Protocol
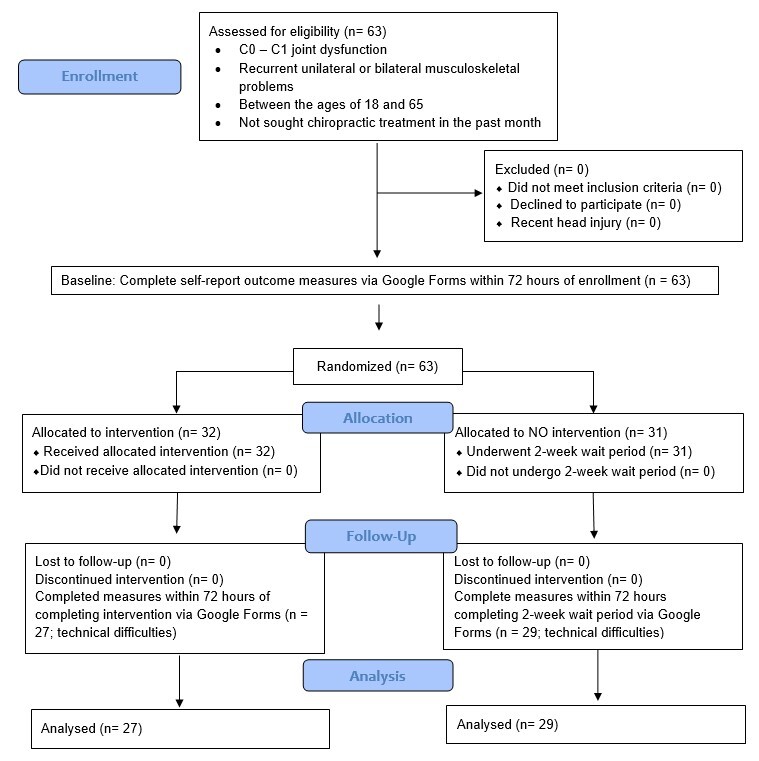
Participants completed a demographic and behavioral survey, and five self-reported measures at baseline, and at follow-up, either post-intervention or control period. The researcher sent a Google Form link (containing the questionnaires) via email, immediately after enrollment and the intervention or control period. Participants were required to complete them in one sitting within 72 hours of it being sent. Figure 1 provides the experimental flow of the RCT.
Neck Disability Index (NDI)
The NDI, a 10-item scale rated on a 6-response Likert scale (0 to 5), has been validated22 (good internal consistency of items,23 and scale22–26) and found reliable in people with neck pain.22,23,25 The NDI was administered to assess changes in self-reported neck disability.23,27 The total score (sum of item scores; out of 50) reflects the degree of neck disability, where a score between 5 and 14 is mild, 15 to 24 is moderate, 25 to 34 is severe, and ≥ 35 is complete.23,27 A 3.5-point change from baseline is the threshold for minimal clinically important difference, and a 5 point or 10%-point change from baseline is defined the minimum detectable change.28
Von Korff Chronic Pain Grade Scale (CPGS)
The Von Korff chronic pain grade scale, a 7-item validated tool, was used to assess changes in self-reported pain severity and pain-related disability.29 The scoring of three subscales provide insight into pain intensity (characteristic pain intensity (CPI)) and pain-related disability (disability score and disability days points).29 Pain intensity is rated using three items on a 10-point Likert scale, generating a CPI score out of 100.29 Pain-related disability is quantified by summing the transformed 4-point score (0 to 3) of the disability score (calculated from 3 items, initially out of 100) and self-reported disability days.29 The combining of pain intensity and pain-related disability scores are used to classify the pain grade.29
Beck Anxiety Inventory (BAI)
The BAI, a 21-item self-report inventory rated on a 4-response Likert scale (0 to 3), has been found reliable30,31 and valid32 in measuring current psychopathology states with high internal consistency30,31,33 in anxiety disorders with a strong physiological component or non-clinical samples who are anxious.31,32 The BAI was administered to assess changes in levels and severity of self-reported state anxiety.30 The total score (sum of each item; out of 63) reflects the severity of their anxiety, where a score between 0 and 21 is low, 22 to 35 is moderate, and 36 to 63 is high.30
Insomnia Severity Index (ISI)
The ISI, a 7-item scale rated on a 5-response Likert scale (0-4), has been found reliable and valid,34–36 with high internal consistency35,36 in documenting perceived, and changes in insomnia severity following treatment in community and clinical samples. The ISI was administered to assess changes in sleeping patterns, severity and impact of insomnia on both nocturnal and diurnal life.34 The total score (sum of item scores; out of 28), reflects severity of insomnia, where a 0 to 7 is nonclinically significant, 8 to 14 is subthreshold, 15 to 21 is clinical/moderate severity, and 22 to 28 is clinical/severe.34
Short Form-36 Health Survey (Sf-36)
The Sf-36 Health Survey, a 36-item questionnaire, has been well-documented as a reliable and valid tool37–41 in assessing quality of life with good internal consistency.40–47 The Sf-36 was administered to document changes in self-reported quality of life/generic functional health status.39,48,49 Participants were instructed to choose one appropriate choice for each item. Item responses were transformed to a score between 0 and 100, where a higher score reflects greater functional capacity.38 The 35 item scores were grouped into 8 subscales, which are: 1) physical functioning; 2) role limitations due to physical health; 3) bodily pain; 4) general health; 5) vitality; 6) social functioning; 7) role limitations due to emotional problems; and 8) mental health. The scores of the 8 subscales were used to calculate the physical component score and the mental component score.37 The one item score provided the participant’s perception of their change in health status.
Intervention: OTZ System vs. No Treatment
Participants allocated to the treatment group received spinal manipulation using the OTZ system that targeted their individual regions of dysfunction. This intervention aimed to correct dysfunctional C0-C1 joint(s) in addition to addressing other dysfunctional joints within the spine and the extremities.14,19 Joint/spine dysfunction, region for applying spinal manipulation, was indicated by biomechanical characteristics, including joint tenderness, restricted intersegmental mobility, asymmetrical intervertebral muscle tension, and abnormal or blocked joint play and end-feel.21 Those characteristics determined whether it was clinically necessary to deliver spinal manipulation, and if joints no longer required treatment. The OTZ system prioritized C0-C1 dysfunction until the joint no longer required a high-velocity, low-amplitude (HVLA) manipulation, and the participant’s initial symptoms (e.g., joint dysfunction or complaints) had improved by at least 80%. This endpoint was selected to standardize the timing of the post-intervention outcome measures, as given that participants had different presenting symptoms and symptom duration, it was expected that the number of treatments needed would vary between individuals (see below for additional details). No other manual treatments or modalities were provided, except for the OTZ system.
Prior to adjusting the C0-C1 joint dysfunction (starting with the side exhibiting the greatest restriction), the clinician used a skull glide to identify the orientation of the dysfunctional C0-C1 joint(s)19,50 while the participant was seated with their hands in their lap. Upon identification, a HVLA thrust was directed at the dysfunctional C0-C1 joint complex, known as the One to Zero (OTZ) tension adjustment.14,19 The line of drive for this HLVA thrust was “posterior to anterior, lateral to medial, and slightly superior to inferior along the orientation of the C0-C1 articulation”,19 see Figure 2 for point of contact. After the C0-C1 adjustment(s), the skull glide palpation was performed again to confirm the dysfunction(s) were corrected, reflected by improved joint mobility.14,19 The treating chiropractor then directed HVLA adjustments and/or mobilization to other dysfunctional segments with restricted movement, based on static joint challenge and motion palpation.21 These adjustments started from the mid-thoracic and lumbosacral regions, progressing to other areas of joint dysfunction. This sequence of adjustments, known as the OTZ system, was conducted at each treatment session, as clinically indicated. As part of the clinician’s standard practice, participants were advised to walk for 30-minutes within 24-hours of receiving the OTZ treatment.
Given the diverse range of presenting symptoms, treatment endpoints differ between participants as the number of treatments provided was dependent on the chronicity and severity of the presenting symptoms. Treatment sessions were performed twice a week for 2 to 6 weeks (i.e. 4 to 11 sessions), with one participant requiring 29 visits over 10 weeks. The treatment endpoint was defined as 80% improvement in initial symptoms, with the C0-C1 dysfunction no longer requiring the OTZ tension adjustment and accompanying joint dysfunction(s) subsiding. The 80% improvement point was measured using a global rating of function and pain (i.e. modified progress assessment that combines the numeric and verbal rating scale51). These validated tools have been used in various settings in individuals with musculoskeletal pain, to determine pain levels/intensity at administration,51,52 and changes in response to an intervention.53 The modified progress assessment permits the chiropractor, to standardize the level of improvement across participants (i.e. decrease in score over time equates to greater improvement compared to their initially defined state), define the endpoint for when post-measures can be performed, and capture the participant’s response to the intervention.
Prior to starting the treatment, the chiropractor verbally administered the global rating of function and pain, where participants were asked to define their current state, by considering their symptomology, mobility levels, and pain levels. This baseline state was recorded as a 10/10 (worse state possible) in the chiropractor’s medical notes. At subsequent treatment sessions, the chiropractor asked the participant how they were feeling relative to their initial visit. Once the participant reported a score of 2 (i.e. 80% recovery) relative to their initial visit, and the clinician confirmed that the C0-C1 joint complex no longer requires treatment by assessing joint functionality, participants were considered ready for the post-OTZ measures.
Participants allocated to the control group completed the baseline survey followed by a two-week wait period, where they did not receive any intervention. This wait period was chosen to mimic the minimum treatment duration of the treatment group. A six-week wait period was avoided to improve participant retention, as many individuals were unwilling to wait that long to see the chiropractor. The wait period’s duration was not expected to affect outcomes, as its purpose was to confirm that, in the absence of treatment, there would be no changes or continued deficiencies in the outcome measures assessed in this pragmatic RCT.
Statistical Analysis
Fifty-six complete datasets with no missing data in all self-reported outcome measures were available. Statistical analysis was conducted on the 56 datasets. Normality of the self-reported measures were assessed using the Kolmogorov-Smirnov test, i.e. n > 50.
Non-normal datasets were transformed using a square root transformation, which included: NDI, disability points of the CPGS, BAI, and the SF-36 (change in health status and physical component score). 2 (time: baseline vs. follow-up) x 2 (group: treatment vs control) repeated measures analysis of variance with pre-planned contrast to baseline were performed for each self-report measure, and subgroup analyses of the ISI and BAI.
Statistical tests were conducted in SPSS® version 26 (Armonk, New York, NY, USA),54 and statistical significance was set at p < 0.05. A correction, Benjamini-Hochberg test, was applied to correct for the 10 outcomes of the Sf-36, which are independent from one another.55 The test adjusts the p-value to control for false positive findings and compares against the false discovery rate (proportionate of type I error), which was set at ≤ 0.20. It is advised to choose a fairly high false discovery rate to avoid a false negative (i.e. missing a potential important discovery).56 The adjusted p-values of the time by group interaction are reported in the results sections as it was used to determined statistical significance. Effect sizes were reported in partial eta-squared (ƞp2), where 0.01 denotes a small effect size, 0.06 denotes a medium effect size, and 0.14 denotes a large effect size.57 The 95% Confidence Interval (CI) was reported for time by group interactions.58 The main effect of time was reported if it was statistically significant.
Results
The recruitment period was September 19th, 2020, to May 8th, 2021, where 63 participants enrolled into the RCT, with 32 participants randomized into the treatment group and 31 participants into the control group. All participants completed the baseline self-reported outcome measures and adhered to their allocation requirements (2-week no-treatment for the control group and pragmatic treatment for treatment group), achieving 100% compliance rate. At the follow-up, 56 participants completed the self-reported outcomes since 7 participants (control: 2; treatment: 5) had technical difficulties (i.e. poor Wi-Fi, browser exit, etc.). None of the participants reported adverse events following the initiation of the intervention. The baseline demographic and clinical characteristics for each group are provided in Table 1, and table 2, respectively.
Neck Pain & Dysfunction
NDI
Self-reported neck disability decreased by 45.21% in the treatment group and 12.60% in the control group, with a significant time by group interaction (F (1,54) = 7.503, p = 0.008, ƞp2 = 0.122; 95% CI: 9.16, 14.22). Only 42 out of 63 participants experienced neck pain, i.e. 21 participants/group. Twenty-one participants in the treatment group had 4.81 ± 4.06 change in points, surpassing the criterion for minimal clinical important difference (> 3.5 points) but not minimum detectable change (> 5 points or 10%-point change). Twenty-one participants in the control group had a 3.33 ± 3.09 change in points, which did not meet both criteria. Table 3 provides the mean score for each group at each time point.
CPGS
Self-reported pain intensity decreased by 43.22% in the treatment group and 6.25% in the control group, with a significant time by group interaction (F (1,54) = 7.146, p = 0.010, ƞp2 = 0.117; 95% CI: -94.06, 61.79). Self-reported pain-related disability decreased by 50.00% in the treatment group and 8.00% in the control group, with no time by group interaction (F (1,54) = 0.683, p = 0.412, ƞp2 = 0.012; 95% CI: -2.18, 1.80). Table 3 provides the characteristic pain intensity and disability points at each time point, and for each group.
Beck Anxiety Inventory (BAI)
Self-reported anxiety decreased by 39.25% in the treatment group and 26.42% in the control group, with an effect of time (F (1,54) = 24.205, p < 0.001, ƞp2 = 0.310), and no time by group interaction (F (1,54) = 0.251, p = 0.619, ƞp2 = 0.005;95% CI: -15.80, 13.25). In participants with moderate anxiety, self-reported anxiety decreased by 37.25% in the treatment group and 25.93% in the control group, revealing an effect of time (F (1,7) = 10.776, p = 0.013, ƞp2 = 0.606) but no time by group interaction (F (1,7) = 0.247, p = 0.634, ƞp2 = 0.034; 95% CI: -25.75, 20.74). Tables 3 and 4 present the group mean scores at each time point and the number of participants at each anxiety level per group, respectively.
Insomnia Severity Index (ISI)
Self-reported insomnia severity decreased by 21.39% in the treatment group and 3.58% in the control group, with no significant time by group interaction (F (1,54) = 1.036, p = 0.313, ƞp2 = 0.019; 95% CI: 9.63, 11.90). In participants with subthreshold insomnia and higher, insomnia severity decreased by 27.64% in the treatment group and 9.54% in the control group, with an effect of time (F (1,29) = 7.299, p = 0.011, ƞp2 = 0.201) but no time by group interaction (F (1,29) = 1.680, p = 0.205, ƞp2 = 0.055 ;95% CI: -14.16, 10.39). Tables 3 and 5 present the group mean scores at each time point and the number of participants at each insomnia severity level per group, respectively.
36-Item Short Form Health Survey (SF-36)
There was a time by group interaction for all subscales, component summary scores and change in health status, determined by the Benjamini-Hochberg correction. See table 9 for mean ± standard deviation (SD), adjusted p-value of the time by group interaction and associated 95% CI.
Discussion
This pragmatic RCT revealed that individuals with chronic musculoskeletal pain and C0-C1 joint dysfunction(s) who received the intervention reported improvements in outcomes of several of the self-report measures, while in the absence of treatment, there was no change in these outcomes. Self-reported neck pain-related disability (NDI), pain intensity (CPI of CPGS), and quality of life (Sf-36) showed a time by group interaction, where self-report measures decreased following treatment. The effectiveness of the OTZ system in reducing self-reported neck-related disability was confirmed by achieving the minimum clinically important difference.28 The treatment group had a greater reduction in self-reported state anxiety levels, and severity of insomnia compared to the control group, however, this did not yield a time by group interaction. These selective improvements in only some outcome measures is likely because many measures were not impaired at baseline, and thus had no room to show clinical improvement.
Selectively Improved Outcomes (Neck Disability and Pain Intensity, and Sf-36)
The post-intervention scores of the NDI and Sf-36 correspond to past work that administered the OTZ system in a population with chronic musculoskeletal problems and C0- C1 joint dysfunction(s).14 The baseline scores of the NDI and Sf-36 in both groups differ from past work,14 which suggests that this RCT comprised of a uniform sample who are not as impaired as the previous study that had a sample with greater symptom severity. The comparison of post-intervention and post-control scores on the NDI and SF-36 shows that simply retaking the measures after 2 weeks has little impact on self-reported neck pain disability or health-related quality of life, in comparison to those who received treatment with the OTZ system who improved in both measures. This is further proved by the NDI scores in the treatment group achieving the minimal clinically important difference.
The large decrease in the CPI of the Von Korff CPGS in the treatment group resembles literature of treatment on pain-related disability and intensity.59–61 The similarity in scores between groups at baseline, and the post-control period score surpassing the baseline score of the treatment group indicates that the OTZ system was effective at improving self-reported pain intensity in this population.
Theoretical Mechanisms
This in combination with the manipulation of dysfunctional spinal segments may have improved central integration of normalized sensory feedback from original areas of dysfunction, with a subsequent enhancement in sensorimotor integration.1,15,62,63 Given the literature linking chronic pain and autonomic reactivity,16–18 it is possible that improvements in autonomic reactivity are responsible for the improvements in the Sf-36. The interplay between these mechanisms and improved joint mobility following the intervention may have reduced pain levels and pain-related disability, resulting in minimal clinical important difference of the NDI scores and reduction in CPI score of the CPGS.
BAI and ISI
The post-intervention scores of the BAI and ISI surpassed and met the scores documented in past work that used the OTZ system on people with chronic musculoskeletal problems and C0- C1 joint dysfunction(s), respectively.14 The baseline scores for both of these measures were similar between groups and close to past work.14 The post-control scores of the ISI surpassed the treatment group’s ISI baseline scores. Despite the greater decreases in the treatment group compared to the control group, neither self-report measures yielded a significant time by group interaction. This could be attributed to the fact that most participants in both groups had low to moderate anxiety, and subthreshold to non-clinically significant insomnia. There were only two participants/group who had moderate severity clinical insomnia and one participant in the control group who had severe clinical insomnia. In fact, there is an effect of time but no time by group interaction with both, ISI and BAI, when examining the participants who had moderate anxiety or subthreshold to severe clinical insomnia. This suggests self-reported change in anxiety and insomnia may not be observed if there are were no problems in these areas to begin with.64 It is likely that participants with greater initial levels of anxiety or severity of insomnia would show greater reductions in these outcomes, as seen in past work,14 but further research is needed to confirm this suspected outcome.
Strengths
The strength of this study is the pragmatic treatment approach, allowing for patient specific care. It is due to the standard percent improvement (80% recovery from baseline symptomology) that the post-intervention responses of the self-report measures can provide insight compared to an arbitrary pre-defined term where the percent improvement may vary across individuals. The findings from this pragmatic RCT are consistent with a previous repeated measures study design that implemented the same intervention on the sample population,14 indicating that the OTZ system induces positive changes in the self-report outcomes that are greatly impaired at baseline. It is interesting that one individual required 29 treatments to reach 80% recovery while the remained ranged between xx and xx. It may be that this person had a previous severe injury. Interestingly, the fact that they were able to recover by 80% highlights the value of using 80% recovery as the endpoint rather than a fixed number of treatments.
Limitations
The results from this study cannot be generalized for individuals below 18 or above 65 years of age. The individual outcome measures assess only 1 aspect of pain and its impact on psychosocial functioning, limiting a multi-dimensional analysis of the biopsychosocial model of pain. However, combining the 5 self-report outcome measures offers insight into how participants’ symptoms may be interconnected, and how this intervention may, or may not, impact the interconnected domains.
The limitation of this pragmatic RCT was that the control group underwent a wait period as opposed to receiving an active control intervention. As this study did not compare the OTZ system to other forms of spinal manipulative therapy, it cannot be stated with certainty that the reported effects are due to the specific method that was used or spinal manipulative therapy in general. Future studies should consider comparing: (1) the OTZ system to other forms of spinal manipulative therapy excluding treatment of the C0-C1 joint, and (2) the OTZ system plus usual care (e.g. exercise or NSAID) against usual care alone. The trial would also have benefitted from a longer follow-up. Unfortunately, as the data was collected during the Covid-19 pandemic, to minimize risk of participants being exposed to Covid, we were not allowed to have patients attend additional sessions where treatment and/or clinical assessments were not being collected. As indicated in Table 1, patients had a number of areas affected. It would have been interesting to do sub-group analysis but most participants indicated that they experienced pain in more than one body region. This also highlights a limitation of the use of the NDI. We had originally thought that that the majority of participants would have neck pain. Given the diversity of areas affected, it would have been good to use a more global outcome measure instead of the NDI. The global approach was accounted for somewhat in the use of the global rating of function and pain, which was administered by the practitioner.
Additionally, as this was a pragmatic trial, the practitioner maintained their usual advice to go for a 30 minute walk within 24 hours of each treatment. It is possible that walking may also be responsible for some of the treatment effects.
Conclusion
This pragmatic RCT demonstrated that the OTZ system, a spinal manipulation-based approach, effectively improves some pain outcomes (i.e. neck pain, disability, and quality of life) in individuals with musculoskeletal pain and C0-C1 joint dysfunction(s) compared to the control group. Further research with appropriate subgroup analyses or regression modeling is needed to determine whether baseline impairment severity influences treatment response. The findings of this study contribute to existing literature for treating musculoskeletal pain that also presents with C0-C1 joint dysfunctions. This work highlights the importance of evaluating and addressing C0-C1 joint dysfunction in addition to other regions of dysfunction in a subset of individuals presenting with this condition, which may inform evidence-based practice, and promote safe and effective complementary therapy interventions.
Acknowledgements
We would also like to acknowledge the efforts of Dr. Patricia McCord for treating the individuals that participated in this study.
Author contributions
All persons who meet authorship criteria are listed as authors, and all authors certify that they made substantial contribution in the work and be held accountable for this work. The individua contributions of each author are, as follows:
-
Conceptualization: USHANI AMBALAVANAR, BERNADETTE MURPHY
-
Data curation: HALIMA HOSSINZEHI
-
Formal analysis: USHANI AMBALAVANAR
-
Funding acquisition: BERNADETTE MURPHY
-
Investigation: HALIMA HOSSINZEHI
-
Methodology: USHANI AMBALAVANAR
-
Project administration: HALIMA HOSSINZEHI, USHANI AMBALAVANAR
-
Resources: BERNADETTE MURPHY
-
Supervision: BERNADETTE MURPHY
-
Validation: USHANI AMBALAVANAR
-
Visualization: USHANI AMBALAVANAR
-
Roles/Writing - original draft: USHANI AMBALAVANAR
-
Writing - review & editing: USHANI AMBALAVANAR, BERNADETTE MURPHY
Funding
This work was supported by Mitacs Canada, and they were not involved in any aspect of the research process.
Competing interests
The author(s) declare no competing interests.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, BM, upon reasonable request but due to the nature of the research/ethics supporting data is not available.