Introduction
The ability to move in accordance with the external environment relies on an accurate internal representation of the body. Muscle spindles are the principal proprioceptors, while joint receptors assist by signaling limits of anatomical integrity,1 and skin receptors contribute minimally.2 Proprioception and other somatosensory inputs (e.g. vestibular, tactile, etc.), along with vision and sound provide the neural bases of the mental representation of position and body movement, known as body schema.3,4
In order to assess body position sense or proprioception, joint position sense (JPS)5 is measured. The assessment of perceived limb or body position in the absence of vision allows for the assessment of the internal mental representation of the body as the change in muscle length is relied on to determine the spatial position of the body part.6 In contrast, matching a target angle permits for the assessment of sensorimotor feedback loops6 as it requires one to compare the actual motor output to the intended motor command, to allow for online corrections of a movement. The use of head repositioning accuracy tests, such as the repositioning to the neutral head position (NHP) test and repositioning to the target head position (THP) test,7 where the vision is occluded, and the participant is required to match an angle (0° (neutral), or percentage of their maximum range of motion (target), provides insight into body schema, and sensorimotor feedback loops.
Transient changes in somatosensory input via experimentally induced fatigue of the dorsal neck muscles increased error in neck flexion/extension repositioning,8 while fatigue of the muscles that elevate the scapulae increased absolute and variable error in right and left head rotation.9 Individuals with recurrent neck pain demonstrate THP impairments (50% of maximum range of motion), but to a lesser extent compared to the NHP, and show a positive association between cervicocephalic kinesthesia NHP in the transverse and sagittal plane, and frequency of pain episode s.10 Impaired cervical kinesthesia is also observed in individuals who experienced whiplash injuries,11,12 and chronic neck pain,13,14 with the NHP task.
Dysfunction(s) of the occipito-atlantal (C0-C1) joint could impact cervical kinesthesia, given that 50% of all proprioceptors in the body are located in the suboccipital muscles,15,16 which project to the caudal brainstem, rostral spinal cord and ipsilateral lateral cuneate nucleus via the dorsal column medial meniscus pathway, alongside the cuneocerebellar and rostral spinocerebellar tracts.17 These projections are critical for conscious proprioception and motor control of the limbs.17 Altered sensory feedback from the upper cervical regions, in addition to physiological changes in neck musculature would likely impact central processing of somatosensory information from the upper limb and vestibular system, as there is a decrease in deep neck muscle activation in those with a neck dysfunction.18,19 Sensory feedback from the sternocleidomastoid muscle (SCM) and trapezius is used by the central nervous system to stabilize the C0-C1 joint, in order to achieve stable vision in the sagittal and coronal plane and assess head position.16,20 As both the SCM and the trapezius attach to the occiput, it is likely that C0-C1 joint dysfunction would alter neck proprioception by altering the body schema given the importance of occipital position for sensorimotor integration (SMI).21,22
The persistent presence of spinal motion segment dysfunction is reflected by reduced joint mobility23 and local tenderness24 and provides a natural “experimental condition” to assess the impact of long-term alterations in sensory input. The administration of high-velocity, low amplitude (HVLA) thrusts directed at the dysfunctional motion segment25 allows for investigation of maladaptive changes in SMI and motor control that may occur in response to joint dysfunction.26 Improved repositioning accuracy is seen after a single session of spinal manipulation27 and after 3 to 5 weeks of treatment28,29 in those with chronic neck pain. Normalized input from muscle spindle afferents,25,30 may have contributed to a more accurate body schema. (31 32) leading to improved motor performance, and in turn, increased accuracy. However, it is unknown whether addressing occipito-atlantal (C0-C1) joint dysfunction would yield improvements in proprioceptive sensibility. The administration of the One-to-Zero (OTZ) tension adjustment (OTZ Health Education Systems, Dallas, TX) alongside thoracic spinal HVLA adjustments have been shown to improve pain and shoulder abduction range in those who had frozen shoulder syndrome.31 Due to the focus of the OTZ adjustment on the C0-C1 joint and the muscles that attach to the occiput, it may improve cervical kinesthesia, as well.
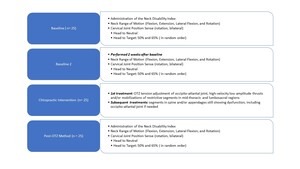
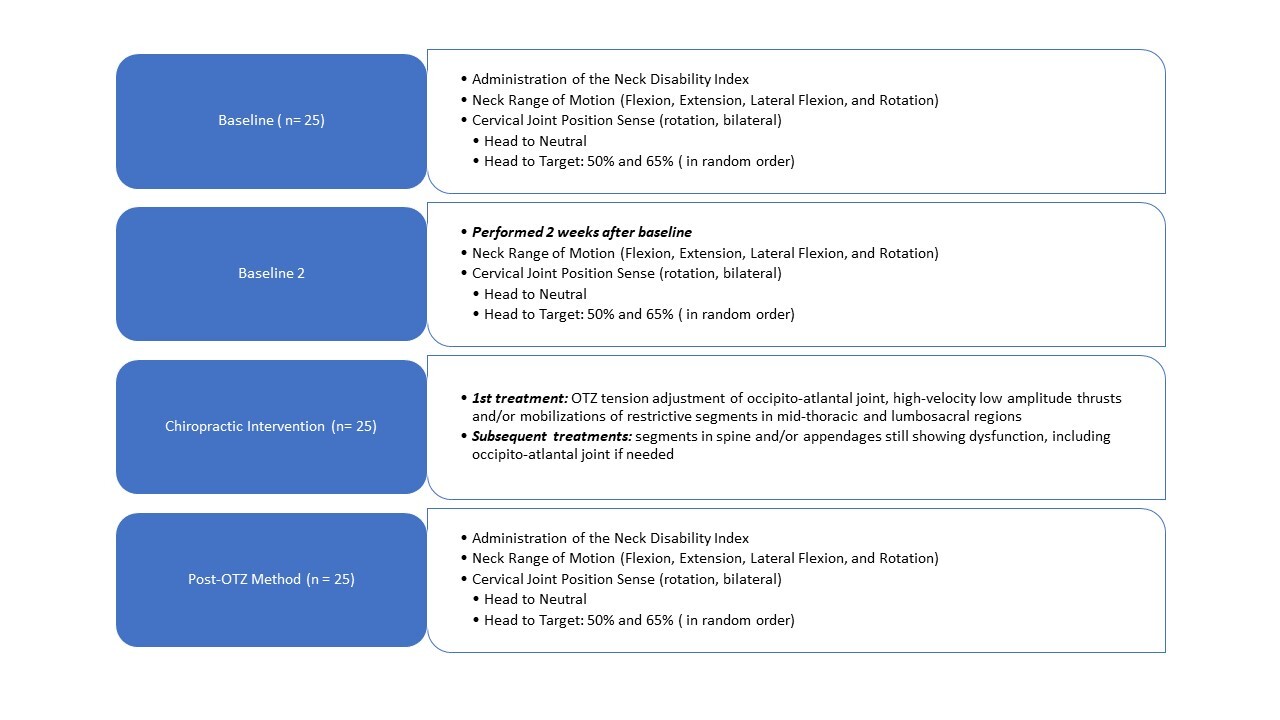
There is literature investigating the impact of cervical kinesthesia in those with a neck dysfunction of varying chronicity and severity, but there is little to no research on the impact from upper cervical C0-C1 joint dysfunction. This is of particular interest, as the C0-C1 joint is the last joint in the spinal kinematic chain and is therefore likely to be of importance in cervical kinesthesia. It is also unknown whether adjustments at the upper cervical spine (C0-C1) in addition to other areas of dysfunction would result in improvements in proprioceptive sensibility. This prospective, quasi-experimental repeated measures study design, with each participant acting as his or her own control (i.e. double baseline completed 2 weeks apart), sought to document initial impairments and any changes in neck mobility, and head and neck repositioning accuracy (NHP, and THP at 50% and 65% of maximum head rotation) following the OTZ method. The main hypothesis of this study was that post-OTZ there would be1: decreases in absolute and variable error in head and neck repositioning accuracy tests, with minimal change to constant error, and2 increased neck mobility in all neck ranges of motion, with the secondary hypotheses that there would be no improvements in between the 2-week control period.
Method
Participants
Power calculations were performed using G*Power.32 Repeated Measures ANOVA within factors statistical test (3 repeated measures with 1 group) was chosen with large effect size set at 0.4, alpha error probability set at 0.05 and Power (1-β) set at 0.95 (to minimize chance of a type II error). These parameters indicated that 18 participants would be needed for this study. To allow for dropouts and/or non-compliance with treatment 25 participants were recruited.
25 participants between the ages of 18 and 65 seeking treatment from a private practice in Toronto, Canada were eligible if they had any of following symptoms in conjunction with C0-C1 joint dysfunction(s): recurrent unilateral musculoskeletal problems (e.g. pain and/or stiffness of the neck, shoulder, back, knee, ankle, wrist, etc.), reduced shoulder ROM,31 and/or full body stiffness (i.e. reduced bilaterally). Long term dysfunction of one side of C0-C1 vertebral motion segment is more likely to result in unilateral musculoskeletal problems. If the head can move freely to one side but not the other, individuals are more likely to have asymmetric proprioception and strength issues.33 Changes in the position of the head and neck have been shown to introduce a systematic deviation in upper limb proprioceptive tasks.34 Unilateral proprioceptive deficits in the upper or lower limb, and the progression of unilateral musculoskeletal problems are closely related.35 The body may compensate in response to the unilateral dysfunction, leading to the progression to bilateral symptomology (e.g. full body stiffness via poor end feel of joints).36
Eligibility was confirmed by the chiropractor, who took the participant’s medical history and conducted a physical examination, which included orthopedic and neurological examination, if clinically indicated. They also affirmed whether participants met the inclusion criteria of having the C0-C1 joint restriction(s) symptomology. The chiropractor confirmed the presence of joint dysfunction(s) in C0-C1 via manual palpation of the joint complex, using a skull glide along the orientation of the occipital condyles to confirm restricted motion.31 Those with recent neurological problems (e.g. traumatic brain injury within the past 5 years, residual symptoms from concussion), and/or neurological disorders (e.g. Parkinson’s), or diagnosed with balance or vestibular disorders, or contraindications to chiropractic care (e.g. history of spine trauma or injury within last 3 months, history of stroke, transient ischemic attacks, cancer, inflammatory conditions or rheumatoid arthritis, infection or systemic disease related to neck pain, fracture or dislocation to the shoulder or spine, bleeding disorders, individuals on anticoagulant medications, etc.) were excluded from the study.
Once the chiropractor confirmed eligibility, the researchers informed the participant of the study details (e.g. right to participate/withdraw, study expectations, etc.). Participants were informed that the participation was entirely voluntary, and the choice to withdraw would not affect their chiropractic treatment plan. All 25 participants provided written and oral informed consent prior to study enrollment. Participants were recruited between October 27th, 2020 - May 2nd, 2021. This research was conducted at a private practice in Toronto, Canada, and in accordance with the Declaration of Helsinki. The study protocol was approved by Ontario Tech University’s Research Ethics Board (REB #: 14817 and REB #: 15908). The reporting of this repeated measures /longitudinal observational study adhered to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist.
Intervention: OTZ Method
Participants received a customized chiropractic intervention that was intended to correct their dysfunctional C0-C1 joint(s) followed by other dysfunctional joints within the spine and/or the extremities, as clinically warranted.
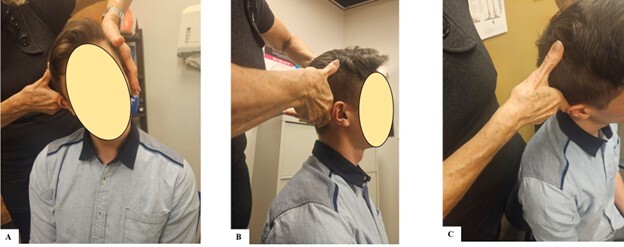
In the first treatment session, the OTZ tension adjustment was administered on the side with the greatest degree of restriction followed by the other side, if also showing restricted mobility. The OTZ tension adjustment consisted of a HVLA thrust administered to the C0-C1 joint complex as described by Murphy,31 which can be performed either supine or seated. The general line of drive was posterior to anterior, lateral to medial, and slightly superior to inferior along the C0-C1 articulation.31 The exact orientation of the C0-C1 dysfunction was determined using a specific skull glide palpation as described by Murphy31 and performed in a similar manner to other studies that have employed this technique.31,37 This was performed before administering the OTZ adjustment, while the patient was seated in a chair, as per the chiropractor’s preference, see Figure 1 for point of contact. During this first intervention session, HVLA adjustments, and/or mobilization of restricted segments within the mid-thoracic and lumbosacral region were also administered, as clinically warranted. In subsequent intervention sessions, the C0-C1 joint complex is manipulated again if the skull glide assessment indicated that the dysfunction was not corrected in the previous treatment session, followed by treatment of other regions of spinal dysfunction, which were addressed with HVLA thrusts (i.e. adjustments), as indicated by restricted joint mobility. The OTZ method addresses the C0-C1 dysfunction prior to other dysfunctional regions, and treatment continues until the C0-C1 dysfunction is resolved. Participants were not given any other manual treatments or modalities, rather advised that they walk for 30-minutes within 24 hours of receiving the OTZ adjustment, as this was the standard advice the chiropractor gave all patients. Participants were treated twice a week for a span of 2 to 6 weeks, where the number of treatments was dependent on the chronicity and severity of their presenting problems.
At the beginning of the first treatment session, the chiropractor administered a global measure of function and/or pain (i.e. a modified numeric and verbal rating scale). This permitted the clinician to capture the participant’s response to their individualized treatment plan, standardize the rate of improvement across patients, and determine an endpoint at which participants were ready to perform the post-treatment outcome measures. Participants were asked to define their current state, by considering mobility, and pain of symptoms. This was defined as their baseline level, reflected by a score of 10/10. At the beginning of subsequent treatment sessions, the participants were asked to re-define their current state at that time. Once participants reported a score of 2 (i.e. 80% recovery) relative to their baseline reporting, the chiropractor informed both the participant and the researchers that the participant was ready for their post-OTZ method measurement session. The post-OTZ method measurements took place between December 5th, 2020, and May 15th, 2021.
Experimental Protocol
Upon confirmation of eligibility, the researchers reached out to the participants via email communication to obtain informed consent prior to booking them in for their baseline collection.
Participants attended 3 data collection sessions with the researcher(s). At each measurement session, the researchers measured the participant’s neck range of motion (ROM) and cervical JPS (neutral head position (NHP) test, and target head position (THP) test (50% and 65% of maximum head rotation)), using a cervical ROM (CROM) device (CROM 3, Performance Attainment Associates, Roseville, MN). Following the completion of the baseline collection, the researcher booked in the participant for their second baseline measurement session (conducted before first intervention), which was set for 2 weeks after the baseline collection. During this 2-week period, participants were instructed not to receive any intervention of any sort. Immediately after completing the baseline 2 collection, participants attended their first treatment session with the chiropractor. Within a week of the participant’s last treatment session, they attended the post-OTZ data collection session, which was booked using email communication (researcher reached out to participant). The chiropractor assisted in the recruitment, ensured that participants met the inclusion criteria, and provided treatment to participants.
The neck disability index (NDI) self-report questionnaire was administered at the baseline and post-OTZ collection measures. Figure 2 provides the flow of the experimental protocol.
Neck Disability Index (NDI)
The NDI consists of 10-items with each item measured on a 6-response Likert scale (0 to 5).38 The summative score, calculated by adding the score of each of the items, is indicative of the degree of neck-pain related disability on activities of daily living.38 A score between 0 and 4 is considered no disability, 5 and 14 is mild disability, 15 and 24 is moderate disability, 25 and 34 is severe disability and a score greater than 35 is indicative of complete disability.38 A minimally clinically important difference (MCID) was set at a change of 3.5 points from baseline.39 The total score at baseline and post-OTZ method for each participant was used in statistical analysis.
Neck Range of Motion (ROM)
Participants were asked to actively move their neck through their pain-free ROM (resist moving past the initiation of pain or discomfort) while wearing the CROM device, to measure neck flexion, neck extension, lateral flexion (left and right), and rotation (left and right). Patients were seated upright with their back pressed against the back rest of a chair, feet planted on the floor and arms resting by their sides. The CROM device was referenced to 0 before and after the completion of each movement, to ensure the plane of interest was not impacted by angle changes in other planes. The researcher and research assistant ensured that there was no shoulder movement or thoracic spine involvement during lateral neck flexion and neck rotation, by having the research assistant stabilize the shoulders while standing behind the participant. A warm-up was provided where participant actively moved through each motion once. Two trials were performed for each motion, and the position where they reached their maximum range was recorded by the researcher. The average of those trials were utilized for statistical analyses.
Cervical Proprioception
Participants were assessed for cervical proprioception using a CROM device40,41 while their eyes were closed (without vision). In order to assess head to target repositioning accuracy, a relative neck rotation angle of 50%10,42,43 and 65%8 of maximum neck rotation was used.
A familiarization trial was provided for both NHP and THP repositioning tests, to ensure participants understood the task.
Repositioning of NHP
The CROM device was secured to the participant’s head and zeroed (goniometer in the main plane set to 0°) to participant’s self-selected neutral, starting and reference position. Participants were then instructed to actively rotate their maximum ROM on the right side before returning to their self-selected neutral position, completed thrice. Prior to testing the left side, participants were asked to actively move their head to end ROM on both sides, then look to the right then the left, to eliminate thixotropic effects. Figure 3 demonstrates a single trial on how NHP repositioning was performed.
Repositioning of THP
Similar to the NHP test, participants were secured with the CROM device and asked to look straight ahead, to set the dial in the main plane to their self-selected neutral position. Participants were passively rotated to either 50% or 65% of maximum neck rotation on the right side, and held for 3 seconds before moving their head to the neutral position. The participant was then asked to actively replicate this target angle thrice. Prior to starting this procedure on the left side, the researcher moved the participant’s head to the right until the end ROM and did the same on the left side. This entire protocol was replicated utilizing either 50% or 65% of their max ROM, if 50% was presented first on the right then it was 65% on the right, and vice versa. The order in which the 50% or 65% of maximum neck rotation was performed, was randomized, to avoid a learning effect. Figure 4 demonstrates a single trial on how THP repositioning was performed.
Data Analysis
The primary outcome measures were the NDI score, neck ROM, and proprioceptive errors.
The position participants returned to was measured by the CROM in the main plane of movement and recorded by the researcher.
For NHP, error was calculated as the difference from the starting neutral position to the returning position. For THP tests, error was calculated as the difference from the target position to the returning position. The error of the three trials was used to calculate absolute, constant and variable error, for all JPS tests. Absolute error (magnitude of error) was calculated by taking the average absolute value of each of the three errors.44 Constant error, reflective of directional bias, was calculated by taking an average of the three errors.7 Variable error, reflective of variability, was calculated by squaring the difference between each error and the associated constant error, followed by the average of the three, before taking the square root.7 The average of each error was used in the statistical analysis.
Statistical Analysis
The primary outcome measures were the NDI score, neck ROM, and proprioceptive errors.
There were 25 complete datasets available for NDI, neck ROM, NHP, and THP (50% and 65%). Normality was assessed using Shapiro-Wilk test. A square root transformation was applied for datasets that violated normality, which included: absolute error for all JPS tests, variable error for NHP, and constant error for THP at 50%, prior to running repeated measures ANOVA, with pre-planned contrasts to baseline. For datasets that violated sphericity (Mauchly’s test), Greenhouse-Geisser corrections were reported. Only statistically significant findings (p <0.05) are reported.
NDI: A paired T-test was performed for NDI scores. ROM: A repeated measures ANOVA with pre-planned contrast to baseline was conducted for neck flexion. A 3 (time) x 2 (sides) repeated measures ANOVA with pre-planned contrast to baseline 1 was conducted for lateral neck flexion and rotation. Proprioception: A 3 x 2 repeated measures ANOVA with pre-planned contrast to baseline 1 was conducted for all proprioceptive errors with NHP testing and THP testing (50% of maxROM and 65% of maxROM) using the CROM, each run separately.
All statistical tests were run using SPSS® version 26.45 Statistical significance was set at p ≤ 0.05. Estimates of effect size were reported as partial eta-squared (ƞp2) or Cohen’s d. Cohen’s d of 0.2 was a small, 0.5 a medium, and 0.8 a large effect size,46 whereas a ƞp2 of 0.01 was noted as a small, 0.06 as medium, and 0.14 as large effects.47
Normalization Process
Percent change from baseline 1 was calculated for neck extension as the baseline measures had large individual variability. A paired t-test was conducted. The equation used to calculate percent change:
PercentChange(%)=TimePoint−Baseline1Baseline1x100%
Results
Demographic and Clinical Characteristics
The demographic of the sample is provided in Table 1, and clinical characteristics are provided in table 2.
NDI
There was a statistically significant decrease from baseline (9.560 ± 5.679) to post-OTZ method (4.400 ± 4.062) measures (t(24) = 5.006, p < 0.001, d = 1.001), with an average change in points of 5.640 ± 4.600 (beyond MCID of 3.5).
Neck ROM
See table 3 for mean ± standard deviation, at each time point.
Head Repositioning Accuracy
See table 4 for mean ± standard deviation at each time point, and per side for each repositioning test.
NHP: Absolute error had a main effect of time (F(2,48) = 7.073, p = 0.002, ƞp2 = 0.228), and for the post-OTZ method contrast to baseline (F(1,24) = 12.083, p = 0.002, ƞp2 = 0.335), figure 5a. Variable error had a main effect of time (F(2,48) = 4.056, p = 0.024, ƞp2 = 0.145), and post-OTZ to baseline contrast (F(1,24) = 6.560, p = 0.017, ƞp2 = 0.215), figure 5b.
THP - 50% of max Rotation: Absolute error had a main effect of time (F (2,48) = 13.840, p < 0.001, ƞp2 = 0.366), and post-OTZ contrast to baseline (F(1,24) = 14.180, p < 0.001, ƞp2 = 0.371), figure 6a. Constant error had a main effect of time (F (2,48) = 4.097, p = 0.023, ƞp2 = 0.146), and post-OTZ contrast to baseline (F(1,24) = 5.011, p = 0.035, ƞp2 = 0.173), figure 6b.
THP - 65% of max Rotation: Absolute error had a main effect of time (F ~(1.515, 36.358)~ = 5.586, p = 0.013, ƞp2 = 0.189), and post-OTZ contrast to baseline (F(1,24) = 5.987, p = 0.022, ƞp2 = 0.200), figure 7a. Constant error had a main effect of time (F (1.53,36.723) = 4.205, p = 0.032, ƞp2 = 0.149), and post-OTZ contrast to baseline (F(1,24) = 5.412, p = 0.029, ƞp2 = 0.184), figure 7b.
Discussion
This repeated measure study demonstrated significant decreases in absolute error in all head and neck repositioning tasks following the OTZ method. The NHP repositioning accuracy test demonstrated decreased variability in repositioning error, following the OTZ method when compared to baseline. Constant error (directional bias in error) decreased following OTZ when compared to baseline in both THP repositioning tests. Neck extension, lateral neck flexion and neck rotation improved. The lack of statistical difference with neck flexion, could be the result of the minimal involvement of the upper cervical spine in this motion.48–50 Relative to normative values of healthy controls, there was poor neck mobility51 and cervical kinesthesia52 at baseline, with no differences between the 2 baselines, suggesting that C0-C1 joint dysfunction and accompanying joint dysfunction may have altered muscle spindle feedback. In addition, the lack of change in between the 2-week control periods suggests that the post OTZ changes were due to the intervention and not just due to getting better at the task. The changes observed suggest that C0-C1 joint dysfunction may have altered muscle spindle feedback, seen as poor proprioceptive error and mobility at the two baselines, followed by an increase in performance and mobility once the spine was re-aligned via the OTZ method.
Neck Disability and Mobility Improvements
The improvement in self-reported neck pain and disability corresponds with past work that has examined the effects of spinal manipulation on neck disability. (27 39) The average change in NDI was beyond the threshold of 3.5 (MCID), suggesting that the OTZ method resulted in clinically important changes in the impact of neck disability on activities of daily living, similar toAmbalavanar.37
The increase in neck extension, lateral flexion and rotation post-OTZ is consistent with studies that examined the immediate and short-term effect of spinal manipulation on active neck ROM.53,54 Martínez-Segura53 demonstrated that a single cervical high-velocity low amplitude manipulation in those with mechanical neck pain improved neck ROM. Meanwhile, Saavedra-Hernández54 found similar improvements in neck ROM with no difference at 1-week follow-up regardless of random allocation to cervical manipulation or combined cervical and upper thoracic spine manipulation. Changes seen post OTZ resemble improvements observed in studies that implemented C0-C1mobilization55,56 or C0-C1 dorsal gliding manual therapy57 but not all ROMs of the neck improved in this study. Neck flexion improved post-OTZ but the change was minimal and not statistically significant. The MCID of neck ROM based on individuals who received physiotherapy for 4 months are as follows: 6° for neck flexion, 4° for extension, 10° for right rotation, 5° for left rotation, 3° for right lateral flexion, and 5° for left lateral flexion.58 Left neck rotation was the only measure to surpass the MCID threshold (5°), suggesting that the improvements in response to the OTZ method are selective.
The observed improvements could be due to improved sternocleidomastoid muscle function as proposed by Murphy.31 The unilateral activation of this muscle is involved in ipsilateral flexion, and contralateral rotation, while bilateral activation results in neck flexion and neck extension.49 The lack of statistical change with neck flexion could be due to the fact that the bilateral activation causes flexion of the lower cervical spine,59 whereas the HVLA adjustments in the current study were directed towards the upper cervical spine.
Proprioceptive Enhancements
The decrease in absolute error post- OTZ with the NHP repositioning task are consistent with García-Pérez-Juana,27 who also demonstrated improvements in proprioceptive awareness in the transverse plane, immediately after a HVLA thrust to the C3 and C4 segments. This is also in line with cervical and cervicothoracic manipulation for 3 to 4 weeks in those with chronic neck pain,29 and those adjusted for 3 to 5 sessions.28 Those studies did not look at absolute, constant or variable error, defining error in terms of distance or score improvement. Although the analysis method was different, those studies are similar to the current study in that the chiropractic care provided included adjustments of cervical and cervicothoracic regions and not just one region of dysfunction in the cervical spine. The OTZ method may have improved cervical kinesthesia due to improved sensory feedback in response to stimulation of the deep paraspinal tissues.25,30 The differences in variable error could be attributed to more consistent kinesthesia, whereas the lack of statistical difference with constant error indicates that there was no directional bias in global error with an NHP repositioning task.
While no past studies have investigated THP in response to cervico-thoracic HVLA adjustments, the decrease in absolute error is consistent with work that look at NHP repositioning accuracy.27–29 The decrease in constant error, alongside decreased absolute error at both 50% and 65% of an individual’s maximum neck rotation, suggests that this intervention may have influenced the accuracy of body perception, most likely by normalized sensory input from the suboccipital muscles, since an accurate body schema is essential to proprioception.60
Potential Mechanisms
The increase in neck ROM, and the improvements in head and neck JPS could be due to the restoration of correct sensory feedback arising from muscle spindles in the suboccipital region. The increase in neck mobility could be due to improved SMI following normalized sensory feedback from neck muscle proprioceptors, since these muscles are involved in neck flexion, extension, lateral flexion, and/or rotation.49 The improved biomechanics and subsequent stimulation of the muscle spindle and Golgi tendon organ afferents via HVLA adjustments of C0-C1, could have improved disordered SMI25,30,61 via restored sensory input from the suboccipital muscles. This restoration of accurate sensory feedback from the neck musculature would have normalized body perception and improved cervical JPS,30 since JPS is dependent on an accurate body awareness.3,4 Given the high density of muscle spindles within the suboccipital muscles (rectus capitis posterior major, rectus capitis posterior minor, obliquus capitis superior, and obliquus capitis inferior), deep muscles which mobilize and stabilize the C0 – C1 joint complex,16,62 it is plausible that the increase in kinesthetic awareness was the result of integrating the increased sensory feedback which is used to update ongoing updating of the internal body schema or body awareness. Central processing may have improved given the suboccipital muscles’ neuronal projections to somatosensory cortex from the dorsal column nuclei via the lateral cuneate nucleus in the medulla.17 It is now known that accurate body awareness is achieved through processing somatosensory inputs (highly dependent on muscle spindle inputs when vision is excluded) in multiple central networks.63 Given that there are deficits in cervical proprioceptive awareness, and cervical SMI and control64–66 due to altered sensory input acquired from muscle spindles with a neck dysfunction (pain, disorders, etc.), it is plausible that the improvements observed in both repositioning accuracy tests could be the result of normalized sensory input following the OTZ method.
Limitations
A potential limitation of this study was the absence of a control group, which could have permitted a comparison between post-OTZ measurements and post-no intervention measurements. The two-week control period showed no change, but to determine that OTZ caused the improvements in neck mobility and JPS would require a randomized controlled design. A global rating of change (GRC) instrument could have been administered in addition to the 80% improvement criterion, to measure and statistically analyze the general progress during the treatment. However, GRCs themselves have limitations (e.g. construct validity, recall bias, etc.),67–69 but variability can be minimized when the administration and the GRC itself is standardized (e.g. explicit mention of specific-condition, construct, and time anchor point in the question).68 Given the main inclusion criteria of C0-C1 joint dysfunction, and the focus on addressing C0-C1 first, suggest that the changes are likely the result of correcting C0-C1 dysfunction, as this was the only adjustment administered to all participants, however this cannot be stated with certainty. Currently, there are no studies on the reliability and validity of the skull glide technique for assessing C0-C1 dysfunction. This should be addressed in future studies.
Future Research Directions
The effect sizes acquired from this study could be used to determine required sample sizes for a future longitudinal studies or randomized control trials. Future work could confirm whether there are alterations in cortical, cerebellar and/or central processing by using various neurophysiological techniques.
Conclusion
This quasi-experimental repeated measure study demonstrated improvements in neck extension, lateral flexion and rotation, as well as, absolute and variable error in HtoN and, absolute and constant error in both HtoT tests following the OTZ method.

__(a)_starting_position__self-selected_n.jpeg)
_for_50__of_maximum_head_rotation__(a)_s.jpeg)
__baseline_2_(blue_diagonal_stripes)_and_post-otz_(orang.jpeg)
_-_mean_of_baseline_(navy_blue)__baseline_2_(blue_diagon.jpeg)
_-_mean_of_baseline_(navy_blue)__baseline_2_(blue_diagon.jpeg)
__(a)_starting_position__self-selected_n.jpeg)
_for_50__of_maximum_head_rotation__(a)_s.jpeg)
__baseline_2_(blue_diagonal_stripes)_and_post-otz_(orang.jpeg)
_-_mean_of_baseline_(navy_blue)__baseline_2_(blue_diagon.jpeg)
_-_mean_of_baseline_(navy_blue)__baseline_2_(blue_diagon.jpeg)