INTRODUCTION
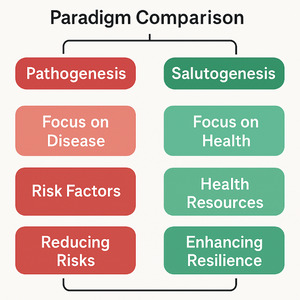
The 21st century has witnessed an unusual rise in lifestyle-related and chronic diseases—cardiovascular disorders, diabetes, obesity, depression, and stress-related conditions—that collectively account for the majority of global morbidity and mortality. Despite extraordinary biomedical advances, the prevailing health model remains pathogenic, oriented toward identifying, managing, and fixing disease rather than creating and sustaining health. The result is a self-contradiction: health systems consume enormous resources to treat illness, yet the global population continues to grow sicker, more sedentary, and psychologically fragile.1–3
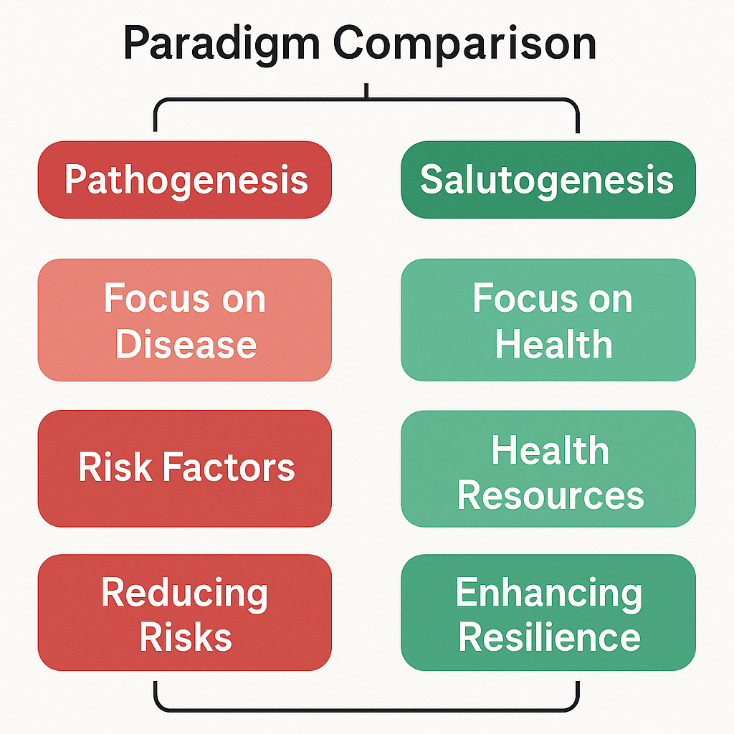
Modern preventive care, though conceptually proactive, often functions within the same risk-based logic as curative medicine—seeking to predict, detect, and mitigate disease before it occurs. While valuable, this approach rarely addresses the positive forces that generate and sustain health.3 This pathology-oriented worldview inadvertently narrows the definition of prevention to risk management, thereby neglecting the broader psychosocial and spiritual dimensions of human flourishing. As Antonovsky1 observed, such a system answers the question “What causes disease?” but fails to ask “What causes health?”
In addition, the dominance of the biomedical model in funding, research, and education reinforces fragmentation: mind is separated from body, individual from community, and biology from meaning.4–6 Consequently, health professionals often focus on modifying risk factors without cultivating resilience, coherence, or purpose—the very elements that enable people to remain well despite adversity.
Aaron Antonovsky’s Salutogenic Model1,4 offers an intellectually robust and empirically supported alternative. Rooted in sociology and stress theory, the model redefines health as a continuum between ease (health) and dis-ease (illness), emphasizing the human capacity to adapt, manage, and find meaning in life’s challenges. Central to this framework is the concept of Sense of Coherence (SOC)—a global orientation that expresses how people perceive life as comprehensible, manageable, and meaningful2. Individuals with strong SOC demonstrate greater resilience, psychological stability, and physiological adaptability across a range of health conditions.7,8
Salutogenesis thus shifts the focus from fixing deficits to building resources—emotional, cognitive, behavioral, and social.9 It recognizes health as a dynamic process sustained by the interplay between individual agency, community support, and environmental conditions.10 This perspective resonates with emerging paradigms such as positive health,9 lifestyle medicine,4 and the biopsychosocial model11—all of which seek to move beyond reductionism toward systems-based, integrative prevention.
The relevance of the Salutogenic Model in the 21st century cannot be overstated. Contemporary health challenges—chronic stress, social isolation, burnout, and inequality—cannot be “fixed” with medication alone. They require a paradigm that empowers individuals and communities to build adaptive capacity and meaning in their daily lives. Recent evidence demonstrates that programs based on SOC and salutogenic principles improve stress management, enhance patient engagement, and foster long-term well-being.2,6 Incorporating this model into preventive care reframes public health from a surveillance-and-risk discipline into a resource-oriented movement—one that cultivates coherence, participation, and hope.
The purpose of this literature review is to explore how the Salutogenic Model can be applied to 21st-century preventive care to shift focus from fixing disease to building health. By synthesizing empirical and theoretical literature across multiple disciplines, this paper aims to:
-
Examine the evolution of the Salutogenic Model and its key constructs.
-
Evaluate evidence supporting its application in preventive care and health promotion.
-
Identify challenges and opportunities for integrating salutogenic principles into health systems and policies.
-
Propose a conceptual framework for operationalizing “health creation” as the foundation of modern prevention.
The following sections present the methodology of this review, the key themes emerging from the literature, and a conceptual model illustrating how salutogenesis can transform preventive care into a system of health empowerment.
METHODS
This study employed an integrative literature review design, enabling the synthesis of empirical research, theoretical discussions, and policy frameworks that explore or apply the Salutogenic Model within preventive health and health-promotion contexts. The integrative review method was chosen for its capacity to incorporate diverse evidence types—quantitative, qualitative, conceptual, and mixed-methods—thereby generating a holistic understanding of a complex and evolving paradigm.12,13
This approach was particularly appropriate because the Salutogenic Model spans multiple domains—ranging from behavioral science and psychosocial theory to public policy and healthcare delivery—requiring a methodology capable of reconciling conceptual breadth with empirical precision. Unlike systematic reviews that emphasize intervention outcomes, the integrative framework allows for theoretical synthesis, identifying how salutogenic constructs such as the Sense of Coherence (SOC) and Generalized Resistance Resources (GRRs) are conceptualized, measured, and applied across disciplines. It also accommodates the interdisciplinary and developmental nature of salutogenesis, capturing both its historical evolution and its emerging applications in 21st-century preventive care.
Furthermore, the integrative approach fosters conceptual innovation, allowing the reviewer to not only aggregate evidence but also identify conceptual gaps, tensions, and future research directions.14 In doing so, it supports a more nuanced understanding of how salutogenesis functions as both a theoretical framework and a practical orientation for health creation. This methodological choice aligns with the review’s purpose—to clarify, integrate, and extend knowledge on the salutogenic paradigm as a foundation for sustainable, non-drug preventive health strategies.
Research Design
The review followed the framework of Whittemore and Knafl,13 which involves five systematic stages:
Problem identification – establishing the need for a paradigm shift in preventive care from disease-fixing to health creation
Literature search – employing structured database queries and inclusion/exclusion criteria
Data evaluation – assessing methodological rigor using standardized tools (e.g., JBI, CASP56)
Data analysis – conducting thematic synthesis across conceptual and empirical studies; and
Presentation – organizing findings into emerging themes and developing a conceptual model for salutogenic preventive care.
Search Strategy
This approach allowed for both breadth and depth of analysis, bridging empirical data with theoretical constructs to illuminate how salutogenesis can transform preventive care.
The central review question guiding this analysis was: How can the Salutogenic Model be applied to 21st-century preventive care to shift health systems from fixing disease to building health?
Sub-questions included:
What evidence links Sense of Coherence (SOC) to preventive health outcomes?
How have salutogenic principles been operationalized in health-promotion and preventive frameworks?
What challenges and opportunities exist for integrating salutogenesis into health systems and policy?
A structured, multi-database search was conducted between January and September 2024, encompassing both peer-reviewed journals and institutional reports.
Databases included: PubMed, PsycINFO, Scopus, CINAHL, Web of Science, and the WHO Global Health Library.
Keywords and Boolean Combinations: “Salutogenesis” OR “Sense of Coherence” OR “Antonovsky” AND “Preventive Care” OR “Health Promotion” OR “Public Health” OR “Health Creation” OR “Resilience” OR “Positive Health” OR “Lifestyle Medicine.”
Supplementary Searches: Backward and forward citation chaining identified additional foundational or highly cited works, including the Handbook of Salutogenesis6 and contemporary applications in organizational and policy contexts.
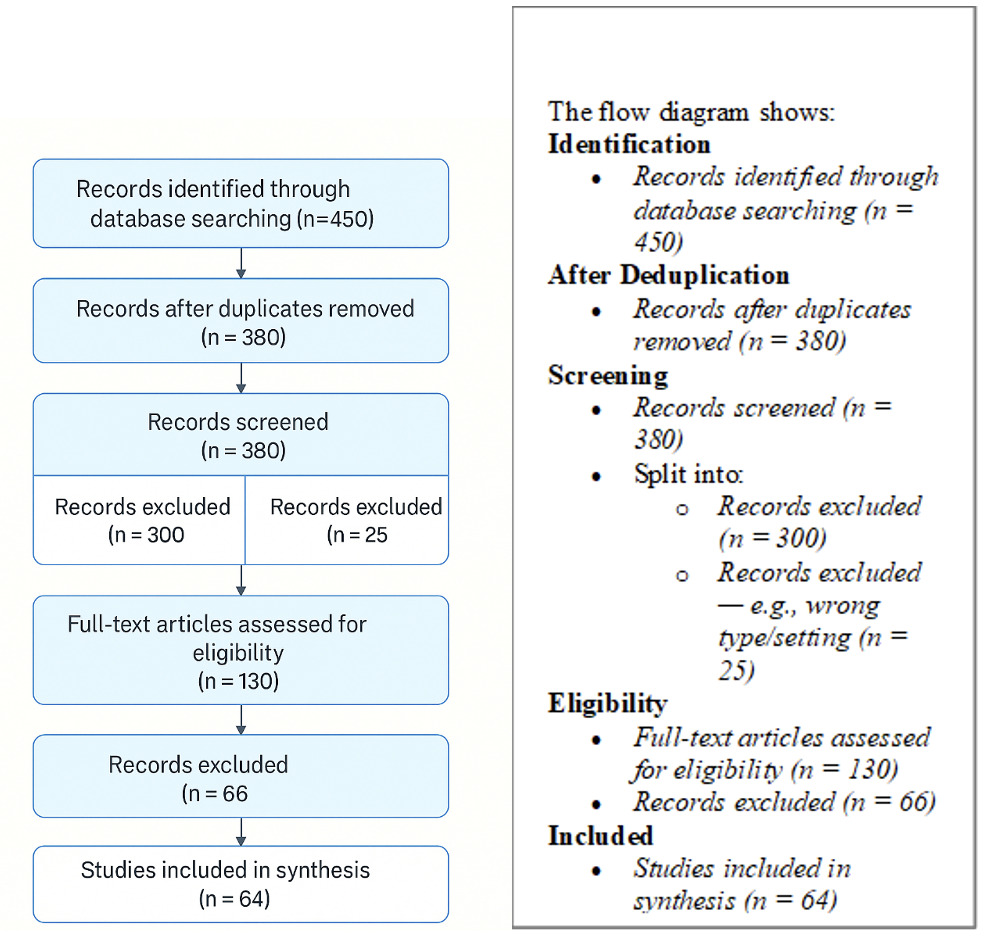
Search results were imported into Zotero for organization and duplicate removal. PRISMA guidelines15 were adapted to ensure transparency in the identification, screening, and inclusion process.
Inclusion and Exclusion Criteria: Studies were included if they:
Were published in English between 1980 and 2024
Were peer-reviewed or derived from reputable institutional sources such as the World Health Organization (WHO) or Centers for Disease Control and Prevention (CDC).16
Discussed or empirically tested the Salutogenic Model, Sense of Coherence (SOC), or related health-promotion frameworks.7–9
Focused on preventive health, public health, workplace health, or community wellness.2,6
Offered theoretical, empirical, or applied insights relevant to health creation rather than disease prevention.3
Sources were excluded if they: focused exclusively on pathogenic, biomedical, or pharmacological interventions11; they were non-human or laboratory-based studies, if they provided commentary or opinion without conceptual or methodological grounding14; or if they duplicated data already represented in larger or more comprehensive studies.15
Screening and Quality Appraisal
Following duplicate removal, all titles and abstracts were screened for relevance. Full texts were then evaluated against the inclusion criteria, resulting in 64 studies retained for analysis: 30 empirical (quantitative or mixed methods), 22 qualitative, 8 conceptual /theoretical, 4 policy frameworks or institutional models.
To ensure methodological credibility, empirical studies were evaluated using the Joanna Briggs Institute (JBI) critical appraisal tools.12. Qualitative and conceptual studies were assessed using Critical Appraisal Skills Programme (CASP) checklists.17 Conceptual relevance, theoretical clarity, and alignment with salutogenic principles were weighted equally with methodological rigor to capture intellectual depth.
Discrepancies during appraisal were resolved through consensus and re-evaluation of study relevance.
Data Extraction and Analysis
A data extraction matrix was developed in Microsoft Excel to systematically record key information from each included study, which included: Author(s), year, country, and publication type, Study design or theoretical framework, Population or context of study, Health domain (e.g., workplace, community, education, clinical prevention), Key findings relating to SOC, resilience, or preventive outcomes, Identified Generalized Resistance Resources (GRRs) (e.g., social support, meaning, autonomy) and Practical or policy implications.
Analysis followed an inductive thematic synthesis approach,18 identifying recurring concepts and relationships across studies. Codes and emerging themes were categorized into three overarching domains1: Salutogenesis as a theory of health creation2 SOC as a measurable construct in preventive practice3 Systemic applications in health-promotion policy and design.
The NVivo 14 software was used for qualitative coding, pattern recognition, and mapping out concepts across sources.
Ethical Considerations
This is a literature-based study, which did not involve human participants. Data was derived from publicly available scholarly and institutional sources. Ethical rigor was ensured by citing the 2025 Vancouver edition accurately, maintaining transparency in documenting the search and the synthesis processes, and maintaining self-examination to minimize interpretive bias.
Results
A total of 64 studies met inclusion criteria, encompassing quantitative, qualitative, and theoretical investigations conducted between 1980 and 2024.
The studies represented a wide range of contexts including public health, occupational wellness, community resilience, education, nursing, and policy design.
Analysis revealed strong convergence around three interrelated domains that collectively illustrate how the Salutogenic Model can transform 21st-century preventive care.
Salutogenesis as the Theoretical Foundation for Health Creation
Across the literature, salutogenesis consistently emerged as a profound paradigm shift from pathogenesis, reframing the central inquiry of health sciences from “What causes disease?” to “What creates health?” (Antonovsky 19794; Lindström & Eriksson 20107). This reorientation challenges the dominant biomedical assumption that health can be understood merely through the elimination of pathology. Instead, it posits that human well-being is shaped by the interaction between stress, resources, and meaning, and that individuals are active agents navigating a dynamic continuum between ease and dis-ease (Antonovsky 1987).1
Within this framework, health is not defined by the absence of illness but by the capacity to adapt, find coherence, and use internal and external resources to manage life’s inherent unpredictability. Salutogenesis thus provides the theoretical foundation for health creation, emphasizing that the origins of health lie not in risk avoidance but in the development of resilience, purpose, and competence to cope with challenges across the lifespan.
Health as a Dynamic Process The literature emphasizes that health is not a fixed state but a continually evolving process of adaptation, meaning making, and coping with stressors (Antonovsky 19871; Eriksson & Lindström 20067). The Salutogenic Model suggests that every person constantly moves along a continuum of health, and one’s position on that continuum depends on how well they mobilize available resources to maintain or restore balance. This view replaces the dichotomous “sick or well” mindset with a developmental and functional understanding of health as a living, adaptive process that can be strengthened at any point, regardless of diagnosis or circumstance.
Generalized Resistance Resources (GRRs)
Central to Antonovsky’s theory are Generalized Resistance Resources (GRRs)—the internal, external, and contextual factors that enable people to manage stress and maintain well-being. These include social networks, spiritual faith, education, financial security, cultural stability, and a sense of autonomy (Lindström & Eriksson 200519; Mittelmark et al. 20226). The literature consistently demonstrates that individuals with strong GRRs exhibit greater resilience, higher Sense of Coherence (SOC) scores, and improved recovery from adversity. GRRs also interact with environmental conditions, highlighting that societies fostering equity, empowerment, and social capital tend to produce healthier and more adaptive populations.
Health Creation vs. Disease Prevention
A major insight across studies is the distinction between health creation and disease prevention. While traditional preventive care seeks to minimize exposure to risk factors, the salutogenic approach focuses on cultivating resources that generate health, such as empowerment, literacy, optimism, and supportive relationships.2,8 The difference is philosophical as much as practical: prevention reacts to potential harm, whereas health creation proactively builds capability and coherence. This conceptual shift redefines wellness as an outcome of capacity building rather than risk management, offering a more sustainable and human-centered model for population health.
The literature positions salutogenesis as a theoretical cornerstone for redefining preventive care in the 21st century. It provides a language and logic for understanding how individuals and societies build health rather than merely combat disease. By foregrounding coherence, meaning, and resource utilization, salutogenesis establishes the philosophical and empirical foundation for a shift from reactive medicine to proactive health creation—the central concern of this review.
Salutogenesis provides the theoretical spine for preventive care: it redefines prevention not as the avoidance of disease but as the ongoing creation of coherence, capability, and resilience within individuals, organizations, and societies. By integrating empowerment, adaptability, and social inclusion into health policy and practice, it transforms prevention from a defensive act to a creative, generative process of human flourishing. This orientation positions the Salutogenic Model as an essential foundation for 21st-century preventive frameworks seeking sustainability, equity, and whole-person health.
Theme 2: Sense of Coherence (SOC) as a Predictor of Preventive Health Outcomes
The Sense of Coherence (SOC) construct—comprising comprehensibility, manageability, and meaningfulness—was consistently validated in the literature as a robust psychological predictor of preventive health behaviors and subjective well-being. Developed by Antonovsky1 as the central mechanism of the Salutogenic Model, SOC reflects an enduring orientation toward perceiving life as structured, predictable, and meaningful, while maintaining confidence in one’s ability to meet challenges using available resources. Across studies, SOC emerged not only as a measure of mental resilience but also as a determinant of physical, emotional, and social health outcomes relevant to prevention and long-term adaptation.
SOC in Preventive Practice
The practical relevance of SOC has been demonstrated across multiple health-promotion contexts, where it influences both preventive motivation and professional effectiveness as summarized in the table below.
Measurement Tools
Antonovsky’s SOC-29 and SOC-13 scales remain the most used assessment tools. However, newer versions (e.g., SOC-E, SOC-SF) allow more context-specific adaptation for community and workplace settings (Super et al. 2016).8
This has implications since Sense of Coherence (SOC) is not merely a psychological trait but a preventive health capacity. It is a measurable determinant of how individuals manage and maintain well-being across life’s continuum. Its consistent association with resilience and adaptability underscores its potential as a core metric for preventive health programs.
Systemic Applications of the Salutogenic Model in Health Systems and Policy
Beyond influencing individual health behavior, salutogenic thinking has increasingly shaped systemic and institutional approaches to preventive health, policy, and environmental design. The reviewed literature reveals that embedding salutogenic principles into the structure of public health, education, workplaces, and care systems can make prevention not only more effective but also structurally sustainable and contextually responsive. This expansion reflects a growing recognition that coherence and resource orientation must be cultivated not only in individuals but also in the systems that govern and support them.
The following areas have been identified for salutogenic model applications. The table below not only shows how to apply it but its effect.
These outcomes illustrate that salutogenesis operates not only as a health framework but also as a socio-cultural development model, strengthening the relational fabric that underpins sustainable well-being.
Policy-Level Outcomes
Integration of salutogenic logic within public policy has yielded measurable structural benefits. Health systems informed by resource-oriented principles tend to be more proactive, participatory, and adaptive—prioritizing capacity building over crisis management. By reframing citizens as empowered participants and focusing on determinants such as education, equity, and social inclusion, these systems foster resilient populations that require fewer reactive interventions.22 According to the World Health Organization,16 policies grounded in empowerment and resource mobilization contribute to long-term sustainability by reducing dependence on high-cost curative interventions and strengthening community self-reliance. In essence, salutogenesis provides the philosophical and structural scaffolding for the next evolution of preventive health systems—those capable of learning, adapting, and thriving amid uncertainty.
Implication
The systemic integration of the Salutogenic Model moves prevention beyond the narrow confines of personal behavior change toward a cultural and institutional transformation. It redefines the mission of health systems from “treating illness” to “building health capacity,” where every policy, environment, and professional relationship contributes to human coherence. This shift represents a paradigm of governance that values empowerment over control and sustainability over intervention—a foundational principle for 21st-century health promotion and reform.
Discussion
The findings of this review affirm that the Salutogenic Model, pioneered by Aaron Antonovsky,1,4 provides not merely an alternative theory of health but a transformative framework for reimagining preventive care in the 21st century.
Across four decades of evidence, salutogenesis consistently demonstrates its capacity to explain why some people remain healthy despite adversity and to guide practical strategies for building resilience, coherence, and sustainable well-being.
This discussion interprets the results through four major lenses1: theoretical implications for the concept of prevention,2 integration with contemporary health paradigms,3 mechanisms of salutogenic prevention, and4 barriers and opportunities for implementation.
Theoretical Implications: Redefining Prevention as Health Creation
Traditional models of prevention—primary, secondary, and tertiary—have long been anchored in the pathogenic paradigm, emphasizing the identification and mitigation of disease risks. While effective for infectious disease control, this risk-based logic is insufficient for chronic, lifestyle, and psychosocial conditions that now dominate global health burdens.9,16
The Salutogenic Model transcends this limitation by repositioning prevention as a process of health creation, not merely disease avoidance.2,19 Rather than focusing on eradicating risks, it emphasizes strengthening Generalized Resistance Resources (GRRs)—such as social networks, self-esteem, cultural stability, and spiritual meaning—which enhance adaptability and resilience across contexts.
This reconceptualization reframes the goal of public health from fixing what is broken to cultivating what sustains life. It moves healthcare philosophy closer to positive health, where well-being arises from balance, purpose, and adaptive functioning rather than the absence of pathology.9 Thus, salutogenesis offers the theoretical scaffolding for an ecology of health, in which biological, psychological, social, and spiritual dimensions are interdependent and mutually reinforcing.
Integration with Contemporary Health Paradigms
The Salutogenic Model aligns naturally with—and significantly enriches—several emerging paradigms in modern health science. Rather than replacing established frameworks, salutogenesis complements and extends them by adding a philosophical and motivational dimension: the understanding that health is not merely maintained through control of risk factors but through the cultivation of coherence, meaning, and adaptive capability.
By translating abstract determinants of health into measurable and experiential constructs, the salutogenic perspective serves as an integrative meta-framework, harmonizing contemporary health approaches across clinical, behavioral, and systemic levels.
Cross-Disciplinary Relevance
The universality of salutogenesis is evidenced by its integration across multiple disciplines. In nursing, it guides patient-centered care that emphasizes empowerment and holistic recovery. In organizational psychology, it informs models of workplace well-being and burnout prevention through meaning, autonomy, and support.28 Community development programs use salutogenic principles to strengthen collective efficacy and social cohesion, while education systems have incorporated them to promote resilience and emotional literacy among students.30 This broad applicability underscores that salutogenesis is not merely a health theory but a comprehensive human-development paradigm that aligns personal, social, and systemic dimensions of thriving.
Biopsychosocial Model
Building on Engel’s seminal Biopsychosocial Model,31 which conceptualized health as a dynamic interaction among biological, psychological, and social systems, salutogenesis provides the operational and empirical complement to this theory. Where Engel proposed a multidimensional structure, Antonovsky offered a mechanism of integration—the Sense of Coherence (SOC)—to explain how individuals navigate and balance these dimensions through comprehension, manageability, and meaning.
The biopsychosocial framework defines the domains of influence on health, but salutogenesis elucidates their interaction by describing how a coherent mindset transforms stressors into manageable challenges rather than threats. For instance, individuals with higher SOC demonstrate stronger physiological stress regulation, healthier coping behaviors, and better social functioning, thereby linking psychological coherence with biological adaptation and social participation.6,7 In this sense, salutogenesis “animates” the biopsychosocial model—providing the motivational and cognitive engine that drives the system toward health creation rather than disease management.
Positive Health and Lifestyle Medicine
The concept of Positive Health, introduced by Huber et al.,9 defines health as the ability to adapt and self-manage amid social, physical, and emotional challenges. Likewise, lifestyle medicine emphasizes the modification of diet, exercise, sleep, and stress behaviors as the foundation of disease prevention.32 Both paradigms represent an important departure from pathology-centered medicine, yet they often remain behaviorally prescriptive—focusing on what individuals should do rather than why they sustain healthy behaviors over time.
Here, salutogenesis deepens both paradigms by addressing the existential and motivational roots of behavior—the inner coherence that gives meaning to self-care. Research shows that individuals with stronger SOC are more likely to maintain healthy lifestyles not out of obligation, but because such behaviors align with their values and identity.8,25 This intrinsic motivation differentiates salutogenic health creation from compliance-based prevention. Moreover, by framing health as a process of meaning-making, salutogenesis connects psychological well-being with biological and social functioning, providing the missing philosophical depth within the positive health and lifestyle medicine movements.
Public Health and Sustainable Development
At the population level, the Salutogenic Model provides a scientific and ethical foundation for the principles articulated in the World Health Organization’s Ottawa Charter (1986), which defines health promotion as enabling people to increase control over their health and improve it. Salutogenesis operationalizes this vision by linking coherence, empowerment, and participation—the psychological and social engines of sustainable well-being.6,19,24
In public health policy, salutogenesis aligns directly with WHO’s Sustainable Development Goal 3 (Good Health and Well-being) and the Health in All Policies movement, which advocates embedding health promotion across all sectors of governance.16 By emphasizing the creation of supportive environments, participatory decision-making, and resilience-building communities, salutogenic governance shifts the focus from treatment systems to societal ecosystems of health creation. The integration of salutogenic principles into national and regional strategies—such as in Finland, Norway, and Canada—illustrates how resource-oriented health policy can enhance equity and collective capacity to adapt in the face of crises such as pandemics and climate stress.11
Synthesis
In essence, salutogenesis provides the unifying language for contemporary health paradigms—bridging clinical care, public health, and population-level wellness through a shared focus on meaningful adaptation. It translates the abstract ideals of empowerment, self-management, and participation into a coherent scientific model grounded in measurable constructs like Sense of Coherence (SOC) and Generalized Resistance Resources (GRRs). By enriching the biopsychosocial, positive health, and sustainability frameworks with a motivational core, salutogenesis offers a meta-theoretical framework capable of guiding the next generation of preventive health and policy innovation.
Mechanisms of Salutogenic Prevention
While traditional prevention often focuses on mitigating risk factors or modifying external exposures, salutogenic prevention operates through a fundamentally different logic. Rather than working against disease, it works toward health creation by mobilizing the individual’s and community’s inherent capacity to adapt, interpret, and find meaning in life’s challenges. Across the reviewed literature, four interrelated mechanisms emerged as the primary pathways through which salutogenesis fosters prevention: psychological coherence, behavioral self-regulation, social connectedness, and environmental support. Together, these mechanisms form a dynamic and reciprocal system that builds resilience and well-being at multiple levels of human experience.
At its core, salutogenic prevention is not an intervention but a process of empowerment—the strengthening of individuals’ and systems’ capacity to perceive stressors as meaningful and manageable rather than overwhelming or pathological.1,29 This shift reframes prevention as an active, ongoing engagement with one’s context, where health is continuously constructed through relationships, resources, and reflection. The goal is not simply to reduce exposure to risk but to expand access to resources of coherence—the cognitive, emotional, social, and structural assets that enable adaptive functioning.
Each mechanism functions within an integrated continuum of influence. Psychological coherence provides the internal lens through which experiences are interpreted; behavioral self-regulation translates meaning into consistent health actions; social connectedness embeds individuals within supportive relationships that amplify resilience; and environmental support ensures that physical and institutional settings reinforce manageability and participation. When these mechanisms operate in synergy, they create a self-reinforcing cycle of health creation—one that sustains preventive behavior even amid uncertainty and change.2,6
Ultimately, the mechanisms of salutogenic prevention represent a shift in preventive logic: from control to capability, from compliance to coherence, and from avoidance to adaptation. Understanding how these mechanisms interact provides a foundation for designing preventive strategies that are not only effective but sustainable—anchored in human meaning, relational strength, and systemic support.
Psychological Mechanism: Coherence and Meaning-Making
At the psychological level, salutogenic prevention operates through the cultivation of a strong Sense of Coherence (SOC)—a global orientation that enables individuals to perceive life as structured, predictable, and meaningful. This inner framework comprises three interdependent components: comprehensibility (cognitive clarity and understanding of events), manageability (confidence in one’s ability to use available resources), and meaningfulness (the motivational belief that life’s challenges are worthy of engagement).1,7
Empirical studies demonstrate that individuals with higher SOC display greater resilience, engagement, and self-regulation, even under chronic stress or adversity.8,24 These individuals interpret stressors not as threats but as manageable demands that can be understood and acted upon. The capacity for meaning-making thus becomes the engine of health maintenance, transforming challenge into growth and stress into adaptation. From a preventive perspective, strengthening psychological coherence equips individuals to sustain health-promoting behaviors over the long term—because they experience such actions as aligned with their values and identity.
In essence, coherence serves as the psychological “software” of prevention: it organizes perception, regulates emotion, and directs motivation toward purposeful engagement with health. This mechanism explains why education and information alone are insufficient for prevention—without meaning, knowledge lacks motivational traction. Salutogenic prevention therefore begins within cognition and purpose, turning knowing what to do into wanting to do it consistently.
Behavioral Mechanism: Self-Efficacy and Consistency
The behavioral dimension of salutogenic prevention centers on self-efficacy—the confidence that one can successfully manage life’s demands and health behaviors. Individuals with higher Sense of Coherence (SOC) demonstrate greater persistence and adherence to preventive behaviors such as regular physical activity, balanced nutrition, stress management, and responsible medication use.8 Unlike externally enforced behavior change, salutogenic prevention builds intrinsic motivation, where behavior arises from internal coherence rather than external pressure or fear of disease.
The literature shows that coherence enhances behavioral consistency by connecting actions to meaning. For example, exercise is not simply performed to prevent illness but experienced as a means of expressing vitality and autonomy.25 Likewise, dietary regulation or adherence to medical routines becomes a reflection of one’s capacity to manage life effectively. This transformation from compliance to coherence explains why salutogenic frameworks produce more sustainable health outcomes than directive or fear-based approaches.29
Moreover, salutogenic interventions often incorporate reflective practices—such as journaling, coaching, or mindfulness—that reinforce self-regulatory awareness, linking emotional and cognitive states to actionable health goals. Behavior thus becomes a feedback loop within the salutogenic system: coherence fuels self-efficacy, which reinforces healthy behavior, which in turn strengthens coherence.
Social Mechanism: Connectedness and Participation
At the social level, salutogenesis emphasizes that health is a collective resource rather than an individual possession. The presence of social capital, supportive relationships, and opportunities for participation significantly enhances both manageability and meaningfulness.2,28 Individuals embedded within cohesive social networks report stronger SOC, greater resilience, and lower levels of burnout and psychological distress.
Participation—whether through family, workplace, or community engagement—creates a sense of belonging and shared purpose that acts as a buffer against isolation. These social interactions not only provide emotional support but also supply tangible resources such as information, assistance, and encouragement that enhance one’s ability to manage stress. Salutogenic social structures are therefore interactive health systems in themselves, continually regenerating resilience through shared meaning and mutual accountability.
Community-based interventions grounded in salutogenic theory have shown improvements in collective coping, civic participation, and mental health outcomes, particularly in marginalized populations.6,21 This underscores that the social mechanism of prevention operates not only through networks but also through culture—the shared narratives and values that make coherence possible at the collective level.
Environmental Mechanism: Designing Health-Supportive Ecosystems
The fourth mechanism extends salutogenesis into the physical and institutional environment, recognizing that coherence is influenced by the spaces and systems people inhabit. Salutogenic design refers to the intentional creation of environments—whether workplaces, schools, hospitals, or cities—that support coherence, accessibility, safety, and connection.21,29 Such environments reduce cognitive overload and stress by being organized, aesthetically pleasing, and supportive of autonomy and participation.
For example, health-promoting workplaces incorporate natural light, communal spaces, and participatory governance, fostering both physical comfort and psychological engagement. Schools designed around salutogenic principles emphasize emotional safety, creativity, and self-directed learning, enabling children to experience education as meaningful rather than obligatory. Similarly, urban planning that integrates green spaces, walkability, and social hubs contributes to collective coherence and public resilience.2
In policy and system design, salutogenic environments also include organizational ecosystems—institutions that empower rather than control, cultivating trust and transparency as structural resources for well-being. Environmental coherence thus completes the salutogenic circle: it externalizes meaning-making into design and governance, embedding prevention into the very fabric of daily life.
Summary
Collectively, these four mechanisms demonstrate that preventive health is not a program but a process of cultivating coherence—a systemic, adaptive capacity operating simultaneously at psychological, behavioral, social, and environmental levels. Each mechanism amplifies the others in a continuous feedback loop: psychological meaning fosters behavioral consistency; behavioral mastery strengthens social participation; social belonging enhances environmental engagement; and supportive environments reinforce psychological coherence. This interdependence reflects the core of the Salutogenic Model: health is not built by eliminating risk but by nurturing the capacity to live meaningfully and adaptively within complexity.
Barriers to Implementation
Despite its growing empirical support, the salutogenic paradigm faces several challenges in mainstream adoption.
Critiques and Theoretical Limitations of the Salutogenic Model
Although the Salutogenic Model has gained wide interdisciplinary traction, several scholars have identified conceptual, methodological, and contextual limitations that warrant critical reflection. Recognizing these boundaries strengthens theoretical clarity and guides more rigorous application in preventive-care research and practice.
Conceptual Ambiguity
A recurring critique concerns the model’s conceptual breadth. Antonovsky’s framework,1 though intellectually compelling, can appear too inclusive to provide precise operational boundaries. Constructs such as Generalized Resistance Resources (GRRs) encompass a wide range of social, psychological, and spiritual assets, making empirical differentiation difficult.30 This conceptual looseness can result in inconsistent interpretations across disciplines, with some studies reducing salutogenesis to mere “positive thinking” rather than a structured theory of adaptation.19
Measurement Challenges
The Sense of Coherence (SOC) scale remains the principal operational tool for measuring salutogenic capacity. However, its psychometric generalizability continues to be debated. Researchers note variations in internal consistency across age groups and cultural contexts.7 In collectivist or faith-based societies, coherence may emerge from shared meaning and communal resilience rather than individual cognition, suggesting that the classic SOC-13 or SOC-29 instruments may under-represent culturally embedded forms of coherence.8,23
Cultural and Philosophical Bias
Salutogenesis arose within a Western sociological tradition emphasizing autonomy, rational control, and self-directed meaning-making. Critics caution that this orientation may not fully align with worldviews that prioritize interdependence, spirituality, or collective identity.21 Consequently, universalizing the model without cultural adaptation risks marginalizing indigenous or faith-based epistemologies of health. Recent scholarship calls for contextualized salutogenesis—frameworks that integrate local narratives of purpose, relational harmony, and spiritual coherence.29
Empirical and Systemic Limitations
Despite robust theoretical development, large-scale longitudinal or policy-level evidence demonstrating systemic salutogenic outcomes remains scarce. Most existing studies are cross-sectional and correlational, limiting causal inference.2 Furthermore, while salutogenesis aligns with “Health in All Policies” principles, operational translation into national or institutional health systems is still emerging.6 The absence of standardized policy metrics for coherence and resilience constrains comparative evaluation across regions.
Integration with Biomedical Paradigms
Another tension lies in the interface between salutogenesis and biomedical reductionism. Health systems organized around diagnosis, pharmacology, and cost efficiency often find it difficult to integrate constructs like meaning or coherence into outcome-based frameworks.31 Without clear indicators or reimbursement pathways, salutogenic approaches risk being perceived as philosophically appealing but operationally peripheral. Bridging this gap requires methodological innovation that quantifies coherence without compromising its existential depth.
CONCLUSION
Overall, these critiques underscore that salutogenesis, while transformative, is not yet a fully mature paradigm. Its strength lies in its integrative vision; its limitation lies in measurement, cultural generalizability, and policy translation. Addressing these issues through refined tools, pluralistic models, and multi-level empirical studies will enable salutogenesis to evolve from an inspiring theory into a global framework for sustainable health creation.
Emerging Opportunities and Future Direction
Despite persistent structural and cultural barriers, the transition toward a salutogenic preventive paradigm is both necessary and achievable. The growing recognition that health cannot be sustained through risk avoidance alone has created fertile ground for models emphasizing adaptability, empowerment, and systemic coherence. Emerging evidence suggests that integrating salutogenic principles into existing frameworks—clinical practice, professional education, public policy, and digital innovation—can operationalize the next generation of preventive health.
Clinical Practice: Strength-Based Assessment and Personalized Prevention
In clinical settings, Sense of Coherence (SOC)–based assessments could be implemented alongside traditional risk screening to identify patient strengths, coping strategies, and contextual resources.6,29 These instruments would complement biomedical indicators with psychosocial insight, allowing practitioners to tailor interventions not only to physiological conditions but also to the patient’s capacity for meaning and manageability. For example, a patient demonstrating low manageability might benefit from structured coaching or peer-support programs, whereas one with low meaningfulness could engage in purpose-driven health counseling. Such personalized, resource-oriented approaches have been shown to improve treatment adherence, recovery rates, and long-term resilience.26
Education: Re-shaping Professional Formation
In health-professional education, integrating salutogenic thinking into curricula can train future practitioners to view prevention as empowerment rather than control. Courses emphasizing the psychosocial foundations of health, narrative medicine, and community engagement can cultivate the capacity to see patients as partners in health creation.24,33 Simulation-based learning that includes reflection on coherence and meaning-making enhances empathy and resilience among students, reducing burnout and increasing their sense of purpose in caregiving roles. In this way, the educational system itself becomes a salutogenic environment, equipping professionals not merely with technical knowledge but with the mindset required for transformational practice.
Public Policy: Investing in Coherence Infrastructure
At the policy level, governments and institutions can apply salutogenic metrics to guide investment decisions toward resilience-building infrastructures—initiatives that expand collective capacity rather than solely control disease. Examples include community programs that strengthen social connection, equitable access to education, participatory urban design, and national campaigns for health literacy.2,16 Policies informed by Generalized Resistance Resources (GRRs)—such as trust, equity, and participation—can be evaluated for their impact on population coherence, creating an evidence-based model of “Health in All Policies.” This reorientation transforms preventive policy into a strategy of empowerment, shifting the economic logic of health systems from treatment expenditure to capability investment.
Technology: Digital Coherence and Adaptive Feedback Systems
Emerging digital health technologies and AI-driven platforms offer new frontiers for applying the salutogenic model. Mobile wellness applications, wearable devices, and interactive dashboards can assess SOC proxies—such as stress perception, emotional balance, and engagement—and provide personalized, adaptive feedback loops that reinforce self-awareness and coherence.2 When designed ethically, such technologies could enable continuous preventive monitoring while preserving autonomy and meaning. For instance, adaptive interfaces can encourage reflection rather than compliance, guiding users to recognize patterns between life balance, social connection, and physiological indicators. In this way, technology becomes a facilitator of coherence, integrating data-driven insight with human agency.
Global Shift: From Reactive Medicine to Proactive Meaning-Making
At the global level, the rise of salutogenesis signals a philosophical and structural shift—from reactive medicine centered on disease control to proactive meaning-making that cultivates wholeness. This paradigm transcends health-care reform; it calls for the re-humanization of science, policy, and education through the recognition that health is a lived experience of coherence. By embedding salutogenic logic within global health governance, societies can move from managing illness to building sustainable human flourishing—a form of prevention that strengthens the fabric of individuals, communities, and nations alike.
Synthesis: From Pathogenesis to Salutogenesis
Ultimately, this review confirms that salutogenesis provides the philosophical, theoretical, and practical foundation for a new generation of preventive health systems. Where the pathogenic model treats disease as deviation, the salutogenic model treats health as potential. It restores human experience—meaning, coherence, connection—to the center of healthcare philosophy. Thus, prevention becomes not a technical act of control but a moral and social project of building a coherent, flourishing society.
The Salutogenic Preventive Care Continuum
Overview of the Model
The Salutogenic Preventive Care Continuum (SPCC) proposed in this review synthesizes empirical evidence and theoretical insights from across health psychology, public health, systems science, and health promotion into a dynamic, resource-oriented framework for modern preventive care. It reconceptualizes prevention not as a reactive response to risk but as a continuous, self-organizing process of coherence-building, in which health emerges through the interaction of psychological, social, and environmental resources. In this model, the focus shifts from “reducing disease incidence” to strengthening adaptive capacity, aligning prevention with growth, learning, and meaning rather than control or fear.1,29
Unlike traditional, linear models of prevention—which segment care into discrete categories of primary, secondary, and tertiary interventions—the SPCC envisions prevention as a cyclical and adaptive continuum. Health is understood as a trajectory rather than a state, maintained through ongoing processes of sense-making, participation, and environmental alignment.2,6 Within this framework, the individual is not a passive recipient of services but an active participant whose capacity for coherence determines how effectively internal and external resources are mobilized toward well-being.
The continuum operates through interconnected domains—psychological, behavioral, social, and environmental—each representing both a dimension of experience and a field for intervention. These domains are not hierarchical but recursive, continuously influencing one another through feedback loops that enhance resilience and coherence over time. For instance, increased social support reinforces psychological meaning-making, which in turn motivates consistent behavior and engagement with supportive environments. The SPCC thus captures the nonlinear, self-reinforcing nature of health creation, depicting prevention as an evolving system of relationships rather than a fixed set of actions.
The Model Integrates Three Major Domains Identified in the Literature1: Determinants of Coherence (Inputs),2 Salutogenic Processes (Transformations),3 Health-Building Outcomes (Outputs)
Determinants of Coherence (Inputs)
At the foundation of the Salutogenic Preventive Care Continuum (SPCC) lie the Determinants of Coherence—the essential personal, relational, and contextual resources that empower individuals and communities to interpret, manage, and find meaning in life’s challenges. These determinants represent the inputs of the salutogenic system, forming the cognitive, behavioral, and motivational substrate upon which all health-promoting processes are built. Drawing directly from Antonovsky’s conceptualization of the Sense of Coherence (SOC,1 these determinants explain how people sustain order within complexity, transforming uncertainty into understanding and adversity into adaptive strength.
The determinants of coherence operate across multiple levels—individual, social, and systemic—reflecting the interdependence of personal meaning and environmental structure. When strengthened, they act as Generalized Resistance Resources (GRRs) that buffer against stress, enhance coping, and amplify resilience19 Conversely, when absent or weakened, they increase vulnerability to fragmentation, helplessness, and chronic stress. Within the SPCC, coherence is not a static trait but a developable capacity, cultivated through supportive systems, equitable policies, and purposeful relationships that sustain human flourishing.
Comprehensibility – The Cognitive Dimension
Comprehensibility refers to the cognitive clarity and sense of predictability that allows individuals to perceive their environment as structured, consistent, and intelligible. When people understand the forces shaping their lives, they can organize experiences into coherent narratives rather than chaotic events. Education, transparent communication, and access to reliable information are therefore critical determinants of this dimension.1,7
In preventive health, clear and trustworthy communication—from government guidelines to patient–clinician interactions—plays a decisive role in fostering comprehension and public trust. Health systems that use inclusive language, culturally adapted messages, and consistent feedback loops enhance both comprehension and engagement. In contrast, fragmented or fear-based messaging increases anxiety and erodes coherence. Thus, comprehensibility functions as the cognitive anchor of prevention, enabling individuals to interpret risks, opportunities, and responsibilities with confidence and understanding.
Manageability – The Behavioral Dimension
Manageability reflects the degree to which individuals believe they possess adequate resources—personal, social, or institutional—to meet life’s challenges. It is the behavioral dimension of coherence, expressed through agency, self-efficacy, and problem-solving.7 Internal factors such as emotional regulation, adaptability, and learned competence combine with external supports—social networks, accessible healthcare, and equitable policies—to create a sense of doability.
Preventive systems that are designed around empowerment rather than compliance reinforce manageability by positioning individuals as capable partners in their own well-being. Programs that develop skills in self-regulation, stress management, and resource mobilization strengthen the belief that health can be actively maintained rather than externally imposed. In essence, manageability represents the behavioral bridge between knowledge and action: it translates comprehension into sustained preventive behavior through confidence and capability.
Meaningfulness – The Motivational Dimension
The third determinant, Meaningfulness, is the motivational and existential core of coherence—the conviction that life is emotionally worthwhile and that challenges deserve engagement. It arises from purpose, belonging, moral conviction, and spiritual alignment, serving as the fuel that drives preventive behavior.1,8,27 People who perceive health as meaningful—an expression of stewardship, responsibility, or vocation—are more likely to maintain preventive behaviors even when they are difficult or inconvenient.
From a salutogenic perspective, meaningfulness transforms health from duty into calling. It instills preventive action with emotional depth and moral coherence, linking personal well-being to broader social and ethical narratives. In clinical, educational, and community contexts, interventions that reconnect individuals to their sense of purpose—through reflective dialogue, values-based goal setting, or spiritual support—enhance motivation and resilience. Meaningfulness thus operates as the energizing force of the SPCC, sustaining engagement and continuity in the health-creation process.
Synthesis: The Resource Foundation of Health Creation
Collectively, Comprehensibility, Manageability, and Meaningfulness form the triadic structure of coherence, the entry point through which preventive health processes are activated. These determinants correspond to both individual cognition and systemic design—meaning that societies, like individuals, can be more or less coherent depending on how they structure understanding, agency, and purpose.2 When reinforced across all levels, these determinants create a synergistic environment where prevention is self-perpetuating: comprehension informs management, management reinforces meaning, and meaning motivates further comprehension.
Within the Salutogenic Preventive Care Continuum (SPCC), these determinants function as the inputs that sustain the health-creation cycle. They provide the psychological and structural scaffolding upon which all subsequent processes—adaptation, participation, and transformation—depend. In this sense, coherence is both the starting point and the goal of prevention: it is the condition through which life organizes itself toward health.
Salutogenic Processes (Transformations)
The transformational core of the SPCC describes how coherence becomes embodied in daily life. While the determinants of coherence (comprehensibility, manageability, and meaningfulness) represent the inputs to health creation, the salutogenic processes illustrate how these resources are activated, internalized, and expressed in practice.
Through ongoing psychological, behavioral, social, and environmental interactions, individuals continuously translate resources into resilience, and resilience into sustained health. In this sense, salutogenic prevention is not a one-time intervention but an adaptive life process—a system of feedback loops where meaning drives behavior, behavior reinforces connection, and connection reshapes perception.6,29
These transformations occur within a dynamic continuum that allows for movement along the health–ease–dis-ease spectrum. Rather than eliminating stressors, the SPCC emphasizes learning to integrate and transform them through coherence. It is in this movement—from confusion to clarity, helplessness to manageability, fragmentation to meaning—that prevention becomes lived health.
The following sub-sections outline the four core transformation domains that embody the salutogenic process:
-
Psychological adaptation
-
Behavioral regulation
-
Social participation
-
Systemic alignment
Each represents a phase of ongoing transformation where health is continuously recreated through experience and response.
Psychological Adaptation
At the center of salutogenic transformation lies psychological adaptation—the cognitive and emotional capacity to interpret stressors as manageable and meaningful challenges rather than overwhelming threats. This adaptive reframing, rooted in Antonovsky’s1 concept of the Sense of Coherence (SOC), serves as the first and most essential step in the transformation of experience into health.
Individuals with strong SOC exhibit a higher tolerance for ambiguity, a greater sense of agency, and an enhanced ability to learn from difficulty. Through the process of meaning-making, stressors are cognitively reorganized into understandable patterns and emotionally reframed as opportunities for mastery.7 This reframing moderates the physiological stress response—reducing chronic cortisol activation, balancing neuroendocrine function, and improving emotional stability.29
Research in positive psychology and neurobehavioral health supports this pathway: adaptive meaning-making correlates with enhanced immune function, lower inflammation, and improved mental health outcomes.27,32 By perceiving difficulty as purposeful, individuals maintain psychological flexibility and optimism—two qualities consistently linked to preventive resilience and recovery.
Within preventive health systems, interventions that enhance psychological adaptation—such as cognitive reframing, mindfulness, narrative therapy, and reflective coaching—activate this mechanism. These practices strengthen coherence by integrating thoughts, emotions, and actions into a unified experience of control and purpose. The outcome is a self-regulating cycle: perception shapes physiology, physiology reinforces perception, and together they sustain adaptive balance.
Ultimately, psychological adaptation transforms prevention from avoidance into engagement. It allows individuals to face uncertainty without disintegration, to act purposefully under pressure, and to construct meaning from disruption. This process represents the inner engine of the SPCC, converting resources into lived coherence—the capacity to stay whole in a changing world.
Behavioral Regulation
Behavioral regulation represents the outward expression of coherence through consistent, self-directed health actions. Individuals with strong Sense of Coherence (SOC) demonstrate higher self-efficacy, persistence, and the ability to align actions with values.8 This mechanism transforms understanding and motivation into observable preventive practices—such as maintaining balanced nutrition, regular exercise, sleep hygiene, and responsible healthcare utilization.
Salutogenic behavioral transformation occurs when individuals shift from reactive compliance to proactive ownership of health. Preventive behaviors become meaningful expressions of identity and purpose rather than imposed duties. Systems that support reflection, feedback, and skill development—through coaching, digital tracking, or peer mentorship—strengthen this loop of intentional, value-driven behavior that sustains health creation over time.29
Social Participation
Social participation embodies the collective dimension of salutogenic transformation. Health is cultivated through meaningful interaction and inclusion within supportive social systems. Engagement in families, workplaces, communities, and civic life fosters belonging, shared purpose, and mutual accountability—conditions that reinforce both manageability and meaningfulness.33
Empirical studies show that individuals embedded in cohesive networks exhibit lower stress, greater emotional resilience, and higher adherence to preventive behaviors. Participation thus functions as both a buffer and an amplifier—it cushions individuals against isolation while expanding access to shared resources and motivation. At the community level, participatory health initiatives that promote dialogue, trust, and collaboration serve as living examples of coherence made social.2
Systemic Alignment
Systemic alignment refers to the process through which institutions and environments become coherent—structuring policies, practices, and spaces that make health accessible, equitable, and meaningful. In salutogenic systems, coherence is embedded in design: clear communication, fair procedures, participatory governance, and supportive environments enable individuals to navigate complexity without disempowerment.6,28
Health-supportive systems act as macro-level resistance resources, reducing social stressors and enhancing public trust. For example, cities designed with green spaces, inclusive education systems, and transparent healthcare pathways create coherence at population scale. Systemic alignment completes the SPCC cycle by ensuring that external environments reflect and reinforce internal coherence, closing the loop between personal adaptation and structural support.
Health-Building Outcomes (Outputs)
The Salutogenic Preventive Care Continuum (SPCC) proposes that when coherence is cultivated through adaptive processes—psychological, behavioral, social, and systemic—health evolves from a fragile condition into a sustainable capacity for resilience and flourishing. These outputs appear at three reinforcing levels—individual, community, and systemic. Together, they define what it means to build health rather than merely prevent disease.
Synthesis
Together, these outcomes demonstrate that sustainable health creation is achievable when coherence operates at every level of society. Individuals thrive, communities self-organize, and systems adapt—together forming a self-reinforcing cycle of wellness that defines the ultimate aim of salutogenic preventive care.
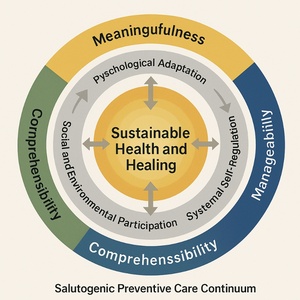
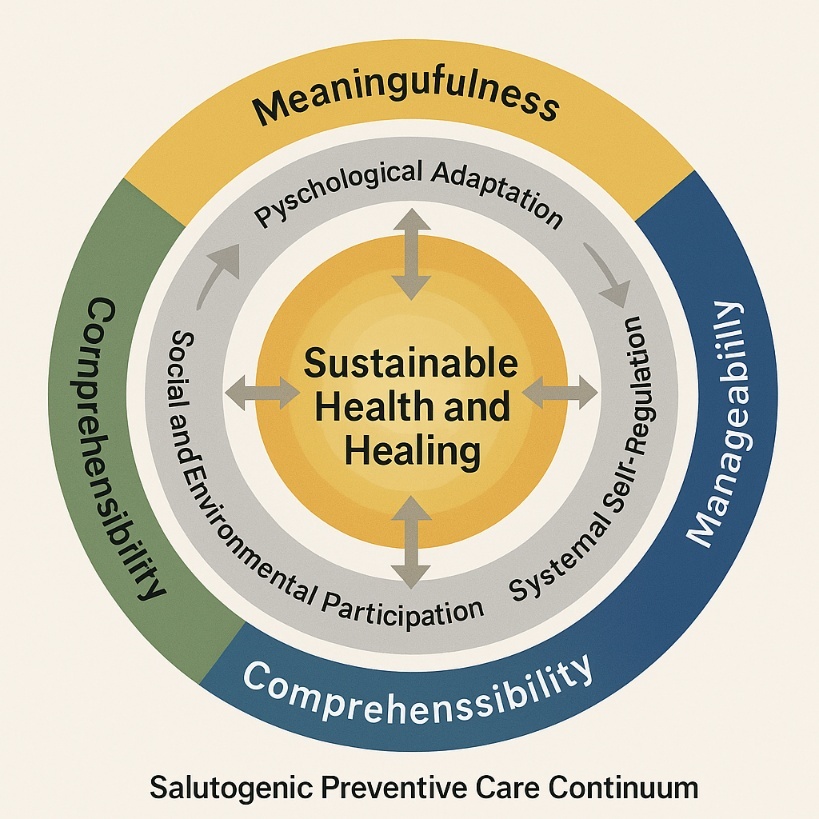
The Salutogenic Preventive Care Continuum (SPCC) Model
The Salutogenic Preventive Care Continuum can be represented as a flowing circular model, capturing the dynamic and self-reinforcing nature of health creation.
Outer Layer – Determinants of Coherence: Encircling the model are the foundational factors—meaningfulness, manageability, and comprehensibility—each represented as a colored band (gold, blue, and green).
Middle Layer – Salutogenic Processes: Arrows illustrate cyclical interactions between adaptation, behavioral regulation, social participation, and systemic integration. These processes turn raw resources into active resilience.
Inner Core – Health-Building Outcomes: The glowing center symbolizes Sustainable Health and Healing, representing a dynamic state of resilience, coherence, and thriving rather than static wellness.
Feedback Loops: Arrows flow back from the inner core to the outer layer, signifying that each cycle of coherence strengthens future adaptability—the more coherence achieved, the greater the capacity for preventive living.
This circular, self-reinforcing design contrasts sharply with the linear pathogenic model of disease progression, embodying the philosophy of continual health creation.
Conceptual Contribution
The proposed SPCC advances the literature by:
-
Integrating salutogenic theory with modern preventive care frameworks.
-
Providing a multilevel model applicable to individuals, communities, and systems.
-
Introducing “coherence” as a measurable and cultivable determinant of prevention.
-
Offering a visual and conceptual map for policymakers, educators, and clinicians seeking to operationalize salutogenesis in practice.
By framing prevention as a dynamic continuum rather than a static goal, this model situates health as an ever-renewing capacity—the ability to meet life’s demands with clarity, purpose, and resilience.
Ethical Considerations, Limitations, and Conclusion
Ethical Considerations
As a literature-based study, this review did not involve human subjects or primary data collection and therefore required no formal institutional ethics approval. However, ethical rigor was maintained throughout in alignment with academic research integrity standards.
Scholarly Integrity
All sources were cited according to the using the latest (2025) revision of the Vancouver style, formally known as the ICMJE (International Committee of Medical Journal Editors) guidelines to ensure proper attribution and intellectual honesty. Every attempt was made to represent authors’ ideas faithfully, avoiding selective interpretation or contextual distortion.
Reflexivity and Positionality
The review acknowledges that salutogenesis, while a universal concept, has cultural and philosophical dimensions that may influence interpretation. The researcher’s perspective—valuing holistic, human-centered paradigms—was consciously bracketed to maintain neutrality. The emphasis was on synthesizing diverse evidence rather than promoting a single ideology of health.
Inclusivity and Representation
Where possible, the literature included contributions from multiple continents and sociocultural contexts, reflecting salutogenesis as a globally relevant framework. The review also gave equal weight to conceptual, qualitative, and quantitative studies to ensure methodological pluralism, consistent with integrative review ethics.13
Limitations
Despite rigorous procedures, certain limitations must be recognized to contextualize the findings.
Scope and Language Bias
The review included only English-language publications, potentially excluding valuable work published in Scandinavian, Asian, or Latin American languages—regions where salutogenic research has flourished.20 Future reviews should incorporate multilingual sources or employ translation to expand inclusivity.
Conceptual Variability
Salutogenesis is inherently interdisciplinary, leading to variability in how constructs such as Sense of Coherence (SOC) or Generalized Resistance Resources (GRRs) are operationalized across fields. This diversity enriches the framework but can complicate direct comparison or meta-analysis.
Empirical Gaps
While the relationship between SOC and health outcomes is well established, few studies have evaluated systemic-level salutogenic interventions in national or institutional settings. The transition from theory to policy remains underdeveloped, limiting large-scale generalizability.2
Temporal Boundaries
This review included literature up to 2024. As salutogenic applications in digital health, AI-based prevention, and sustainability are rapidly emerging, future studies will need to update and expand these findings.
Conclusion
The findings of this review highlight a clear and urgent truth: the pathogenic model of healthcare—focused on fixing diseases—is insufficient for the health challenges of our time. The Salutogenic Model offers not merely a supplement to biomedical prevention but a philosophical and operational adaptation toward the creation and maintenance of health as a living process.
Salutogenesis calls for a paradigm shift in healthcare with emphasis on prevention, where individuals and systems thrive through adaptability, participation, and meaning. It reframes the central question of health sciences from “How do we prevent illness?” to “How do we build and sustain well-being?”1
This shift—from treating pathology to cultivating potential—has profound implications for every dimension of health and society.
For health professionals, adopting a salutogenic lens means shifting focus from symptom management to resource enhancement. For policymakers, it invites re-evaluation of success metrics—from reduced mortality to increased adaptability, participation, and quality of life. For educators, it encourages teaching health as a capacity to create order and purpose amid uncertainty.1
When applied systemically, this framework leads to sustainable health systems that conserve resources not by restraint or self-denial, but by cultivating resilient, coherent populations who require less corrective care.
Future Directions
To advance this paradigm, future research should:
Develop and validate salutogenic policy indicators, such as community coherence indices.
Investigate longitudinal effects of SOC-based interventions on chronic disease outcomes.
Explore integration of salutogenesis with digital health technologies for personalized, adaptive prevention.
Promote interprofessional education that unites medicine, psychology, public health, and theology under a shared vision of health creation.
As Antonovsky envisioned, health is not a destination but a lifelong movement along the continuum of coherence.1 In an age of chronic stress, environmental instability, and global inequity, the world no longer needs systems that merely repair the broken. It needs systems that cultivate coherence, meaning, and participation—systems that teach humanity to flourish, not just function.
Acknowledgement
Portions of this paper—including editing, organization, and refinement of tables and references—were developed with the assistance of an AI language model (ChatGPT). All interpretations, final decisions, and substantive scholarly contributions are the author’s own.