Introduction
Occipital neuralgia is defined as electric or shock-like pain over the posterior head, in regions innervated by the 3 branches of the occipital nerve (ON): the greater occipital nerve (GON), lesser occipital nerve (LON) and third occipital nerve (TON). It can affect 1 or all branches. The etiology of ON is unknown. It is paroxysmal in nature, usually affecting people over 50 years of age.1 Diagnosis is confirmed using diagnostic imaging or nerve block injections. Nonsurgical interventions largely consist of nerve blocks, pulsed radiofrequency ablations, botulinum toxin injections, acupuncture, or manual therapy.1
CASE REPORT
A 57-year-old female sought care for acute left suboccipital pain that traveled up the posterior aspect of her head. She was diagnosed with COVID-19 2 weeks prior to the onset of symptoms. She had since tested negative but was still experiencing minor cold-like symptoms. No other physician was seen for the suboccipital complaint, and no radiographic imaging had been ordered prior to her initial visit for this complaint.
Clinical Findings
During the initial examination, she stated the pain was a constant throbbing feeling, rated as a 2/10, with frequent, short episodes of an excruciating electric-like shooting pain, rated as a 9/10 on the Visual Analogue Scale (VAS). The frequency was roughly 20 times per hour. The throbbing pain was present throughout the day, while the shooting pain would present randomly. The patient denied a specific provocation. Lying prone was moderately relieving. She stated she would lie prone, or sleep, on a home massage table that allowed her to relax in a neutral spine position.
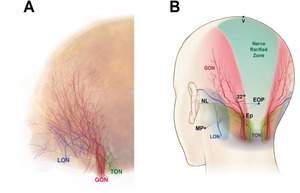
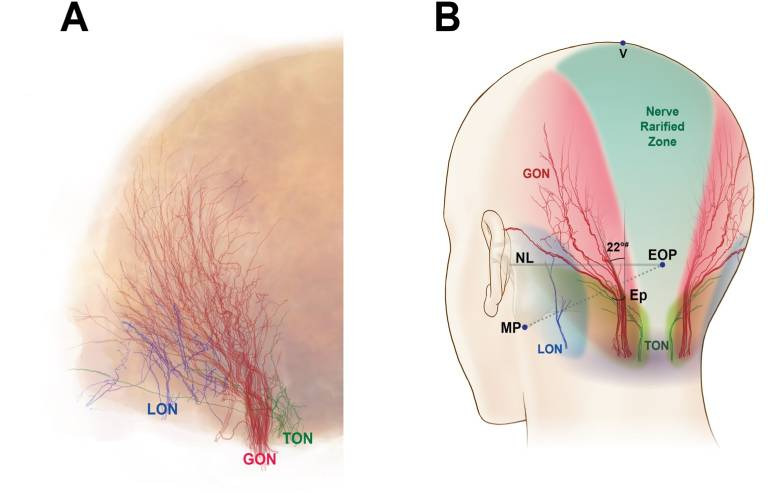
Initial examination of the patient included vital signs, visual inspection, palpation, upper extremity muscle strength assessment, deep tendon reflexes, sensory function, active and passive range of motion, orthopedic testing of the head/cervical region, and a cranial nerve examination. Her blood pressure was elevated, at 132/80mmHg. Both active and passive cervical flexion reproduced her chief complaint of shocking pulsations traveling from the left side of the upper cervical spine to the left ear and behind the left eye. Maximal foraminal compression test reproduced local pain when performed on the left side, producing a “pulling feeling” on the left side of the upper cervical region with left rotation and extension. Chin flexion test reproduced the pulsating/throbbing pain. Tinel tap test over the left suboccipital region between the left C1 transverse process and the left lateral occipital ridge was positive for reproduction of acute pain and numbness over the left side of the head. Tinel’s tap test also elicited an intense episode of shooting/electric-like pain traveling from the left suboccipital region to the left side of her head. Palpatory findings demonstrated hypertonicity of the left suboccipital musculature, and segmental and somatic dysfunction of the cervical spine. The patient’s description and location of symptomatology is consistent with the Greater Occipital Nerve referral pattern (Fig. 1).2,3
The Pain Disability Questionnaire (PDQ) score was 86/150 (moderate disability), and the Yellow Flag Questionnaire score was 71 (High risk of chronic pain & disability).
Differential diagnosis included Migraine headache, C2 arthrosis, and Occipital Neuralgia. It was noted that this patient has no prior history of migraines.
Diagnostic Assessment
The patient was referred for a head MRI and a brain MRA to assess vascular structures due to the recent COVID-19 illness and symptoms related to the chief complaint. Cervical radiographs, consisting of AP lower cervical, lateral and APOM views, were taken to rule out any structural causes of occipital neuralgia. Imaging was normal and unremarkable for congenital defect.
Therapeutic Intervention
The patient was seen once weekly for 8 weeks, with treatment consisting of low-level laser therapy delivered 1.4 J/s at 85% duty cycle for a total dose of 1.19 J/s in the bilateral suboccipital region, for a total of 8 minutes. Manual therapy was not tolerated well by the patient, due to the reproduction of the acute shock-like symptoms, so laser was the most conservative option. The second and subsequent visits consisted of the same low-level laser therapy on the suboccipital musculature. She reported no pain or other symptoms on the third visit. The patient was complaint to treatment for the remainder of the care plan with no additional pain or complaints. (Table 1)
At re-examination, the previous positive findings were now negative (Tinel tap, Active and Passive ROM, and chin flexion Test, maximal foraminal compression) with no new objective findings. Palpatory assessment of the cervical spine and occipital region was unremarkable. The Pain Disability Questionnaire (PDQ) score reduced from 86/150 on the initial visit to 0/150 at the re-evaluation. The Yellow Flag Questionnaire score was reduced from 71 to 30 (low risk of chronic disability).
Discussion
The International Headache Society classifies ON as a headache, with unique referral patterns based on which branch of the Occipital nerve is affected.2 The GON derives from the C2 primary rami and innervates the posterior and superior region of Occiput, with the foramen located in the medial suboccipital region, lateral to the external occipital protuberance (EOP). Pain from the GON refers from the Occipital region to the crown of the head. The Lesser Occipital Nerve (LON) also originates from the C2 rami, with distribution more laterally to the posterior auricular area. The Third Occipital Nerve (TON) derives from the C3 primary rami, and is located most inferiorly between the EOP and largest branch of the GON.
Identifying which nerve is involved in ON is based on the pain referral patterns (Fig 1).4 Researchers have identified areas of muscle compression that may cause entrapment symptoms consistent with those described by patients. These areas of muscle compression occur where the GON travels through the semispinalis capitis mm., oblique capitis inferior mm., and the suboccipital fibers of the trapezius mm.3 Fascial tissue changes in the suboccipital region could also provide compressive forces on these nerves. Stecco et. al. discusses immunohistological research involving the “aponeurotic fascia”, like the thoracolumbar fascia at the sacrum, or the occipital
aponeurosis of the trapezius. Aponeurotic fascia is highly innervated and in communication with adjacent mechanoreceptors, which react to movements in the surrounding muscle layers. Fascial constrictions within the various muscle layers which terminate in the suboccipital aponeurosis may indeed contribute to the onset of ON.5
Treatment of ON is largely nonsurgical, but can consist of nerve blocks, pulsed radiofrequency ablation, tissue debridement, even fascial hydrodissection.2,6–8 Clinical goals with local corticosteroid injection are 40-50% reduction in symptoms, over a 6-week period.3 This level of perceived clinical success may be frustrating for patients with ON, as the symptoms can be quite debilitating. Other non-invasive treatments include acupuncture, manual therapy and NSAIDS. Of those modalities, acupuncture has the most robust representation in the literature and demonstrated good benefits for treatment of ON.6 Low level laser therapy for ON is not well documented in the literature.
CONCLUSION
Despite the paucity of evidence for laser therapy for incidence of ON, this case study demonstrated successful treatment for an acute onset. Further studies are warranted to determine the role of low-level laser as a non-surgical, non-invasive treatment for patients with Occipital Neuralgia.