INTRODUCTION
Chronic low back pain is the single leading cause of workplace disability in the United States, requiring upward of $50 billion in health costs annually.1 With the addition of lost wages, the economic cost of associated with chronic low back pain rises to an estimated $100 billion.2,3 Researchers estimate that 80% of the population will experience low back pain at some point in their lives.4 There are various forms of interventions in common use for the treatment of chronic and acute low back pain. These include pharmaceutical medical intervention, including nonsteroidal anti-inflammatory drugs (NSAIDs), various forms of manual therapies, and spinal manipulative therapy.5,6 Cox® Technic flexion-distraction decompression is a form of spinal manipulation that has shown success in the treatment of chronic low back pain, including for disc herniations and spinal stenosis.7,8
The purpose of this paper is to discuss the use of a side-lying position for Cox® Technic flexion-distraction decompression for low back pain relief in a patient who was unable to lay prone due to pain. This type of accommodation for patient comfort may be helpful for applying flexion-distraction in similar patient conditions.
CASE REPORT
An 80-year-old female sought chiropractic care for the management of her low back pain, which she described as having a dull, achy, and burning quality. She could not recall the mechanism of onset or any recent trauma that could have provoked her pain. She rated her pain as a constant 8 out of 10 on the numeric pain rating scale (NRS), whereas “0” represents “no pain” and “10” represents “the worst pain possible.” She described her pain as chronic (ongoing for several years) in duration, but flared over the 2 weeks prior to her evaluation. She reported that her activities of daily living were limited due to her low back pain, and walking, sitting, standing, and sleeping were especially limited. Her history included diabetes, hypertension, and chronic low back pain. She reported an episode of sciatica 2 years prior treated with physical therapy with fair results. Foot drop was present and is the major contributor to her need to use a cane.
She stood 5’ 2" tall and weighed 150 pounds. She had bilateral foot drop and she walked using a cane. Her lumbar spine ranges of motion were all reduced and provoked pain, with the most marked reported during extension. The orthopedic exam revealed the following positive tests (shown in Table 1).
She was unable to lie in the prone or supine position, due to severe low back pain. Lower extremity muscle testing (myotome testing) were all normal and graded 5/5, with the exception of bilateral dorsiflexion being slightly weak and graded as 4/5. Lower extremity deep tendon reflexes revealed the patellar reflex to be 2+ and the Achilles’ reflex was 1+, bilaterally. Palpation revealed tenderness at the lumbosacral region of the spine (L3–S1 levels). Hypertonicity was palpated in the lower lumbar paraspinal muscles, along with the quadratus lumborum and piriformis muscles, bilaterally.
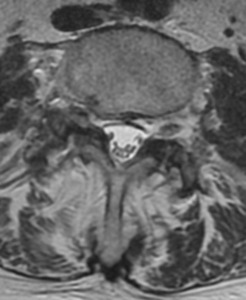
Her MRI images are presented in table 2 and figures 1 and 2. They demonstrate the presence of a number of findings.
The treatment schedule and plan were set for 3 times per week for a 4-week period, totaling 12 treatment visits. We used Cox® Technic flexion-distraction decompression spinal manipulation, with the goal of achieving a 50% improvement in the patient’s pain (via NRS) and objective clinical improvement. As per Cox protocols, when 50% improvement is reached, treatment frequency will be reduced by half and continue to be reduced by half with each 50% subjective and objective improvement measured.9 Subjective measures included verbal rating scale and objective measures included Kemp’s test, range of motion documentation, and straight leg raise test.
Since the patient was unable to lay prone comfortably, we treated her with Cox Technic flexion-distraction decompression in the side-lying position for Protocol I and II treatments. When performing the Cox Technic protocols in the side-lying position, the table’s lateral flexion capability becomes an anatomical flexion motion and the instruments flexion capability becomes a lateral flexion motion, thereby allowing the ranges of motion which would normally be performed with the patient in the prone position.
Electrical muscle stimulation and infrared light therapy were also involved in this treatment plan and were administered in-office at each visit. A home exercise program was also prescribed; this program focused on stretching and XYZ movements were recommended. Other home care recommendations included ice applications, a lumbosacral brace support, and lifestyle modification. She responded well to the treatment plan. After a total of 16 visits, she reported an absence of lower extremity radicular pain and rated her pain having dropped to a 3 out of 10 on the NRS. She also self-reported improved sleep, improved walking ability, increased ability to climb steps, and less discomfort with prolonged sitting during travel.
DISCUSSION
In older adults, lumbar spinal stenosis is the leading cause of disability, pain, and loss of independence.10 The most common presentation is caused by age-related spinal degenerative changes that narrow the spinal canal; these changes may result in direct compression and/or diminished blood flow to the lumbar nerve roots, resulting in back pain and lower extremity paresthesia.11 Limited walking is often the most severe form of impairment. This can lead to a sedentary lifestyle and decline in overall health status.12 Limited walking is often a result of neurogenic claudication, characterized by bilateral or unilateral lower extremity pain, heaviness, numbness, tingling or weakness, relieved by sitting and forward flexion.11,13 Increased disability can result as a consequence of depression levels, hopelessness, and anxiety that is associated with spinal stenosis and concurrent symptoms.14 Effective treatments for spinal stenosis include physical therapy, oral anti-inflammatory medications, and epidural steroid injections.15,16 Although there are short-term benefits, lumbar epidural steroid injections do not demonstrate long-term improvement of pain and disability in lumbar spinal stenosis patients. Lumbar corsets may also be used for temporary relief of pain.17 More recently, structured comprehensive training procedures with conservative treatments show benefit for spinal stenosis.18 Treatments included patient education, exercise therapy, manual therapies, and self-directed at-home training exercises.18
Cox Technic protocol I is utilized for radicular pain that extends below the patient’s knee.9 The patient will be in a prone position on the flexion-distraction table. After tolerance testing is applied (i.e. the flexion-distraction motion does not increase radicular symptoms, Cox® Technic protocol I is performed. With more clinical experience, protocol I may be performed using doctor-controlled, automated, long-y axis distraction during the flexion stage of this process. Protocol I includes the application of distraction to the specific lumbar segments affected with 5 4-second “pumps” of flexion repeated 3 times. Between each set of flexion and distraction, trigger-point therapy to the paravertebral spine musculature is applied, particularly to dermatome-involved nerves and the gemelli-obturator internus complex, through which the sciatic nerve passes.19 Use of this protocol has shown restoration of physiologic motions to the lumbar spinal segments.20
In certain circumstances, patients seeking care for treatment for low back pain, however exhibit difficulties laying prone or supine. Often pregnancy, respiratory difficulties, or severe pain prohibits patients from assuming this position, which is the normal position for use of Cox® Technic flexion-distraction decompression. By using a lumbar segment of the flexion-distraction table that can traverse left and right lateral flexion, extension, and the flexion planes of motion, the practitioner can achieve flexion and extension motions. Further, this position may still permit the practitioner to achieve the fundamental goals of reducing the intradiscal pressure and restoring physiologic motion during treatment.
This side-lying postural approach to flexion-distraction decompression is not isolated to just the elderly. A similar case demonstrated effective treatment with side-lying Cox® Technic for a pregnant 26-year-old woman.21 She had low back pain and radiculopathy. She could not lie prone, so side-lying Cox® Technic flexion-distraction decompression was administered.21 She experienced complete resolution of her condition after 8 visits.21
These 2 reports serve as a foundation for the necessity of continued case studies using this modified Cox® Technic flexion-distraction decompression for patients who cannot lie prone.19 These demonstrate the necessity of biomechanical research for Cox® Technic flexion-distraction decompression in the side-lying position to evaluate intradiscal pressure that may or may not correlate with previous research demonstrating changes in the prone position.22
Limitations
There are a variety of limitation identified within this single case study. First, clinically objective measurable findings were absent outside of the patient’s verbal pain scale. This absence limits empirically valuable information regarding the patient’s response to pain. However, studies have emphasized the importance that subjective response can have over empirical findings.23 While it is possible that Cox® Technic flexion-distraction decompression assisted in the relief of pain for this patient, other generators and treatment methods cannot be excluded. The gemelli-obturator internus muscle can also generate pain in the retrotrochanteric gluteal space and, as in this case, trigger-point therapy was used for this anatomic region. Also, electronic stimulation, heat therapy, low-level laser, and at-home exercises were prescribed. It would be prudent to note that previous research demonstrated patients had more significant pain relief with flexion-distraction than active exercise alone.21
CONCLUSION
Chronic low back pain and spinal stenosis are conditions affecting many and has an economic cost in the billions of dollars.1–3 For many practitioners, flexion-distraction manual spinal manipulation is the preferred choice of treatment for this condition.18 This treatment process typically requires patients to assume the prone position for treatment.9 For patients with low back pain that are unable to lie prone, use of a side-lying posture may serve as an effective alternative for Cox® Technic flexion-distraction decompression. Although this single case study does not verify the efficacy of the side-lying treatment for Cox® Technic flexion-distraction decompression, the study certainly opens the door for further research using this protocol for patients who cannot lie prone.