Introduction
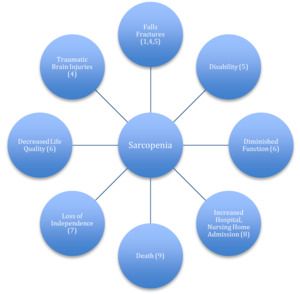
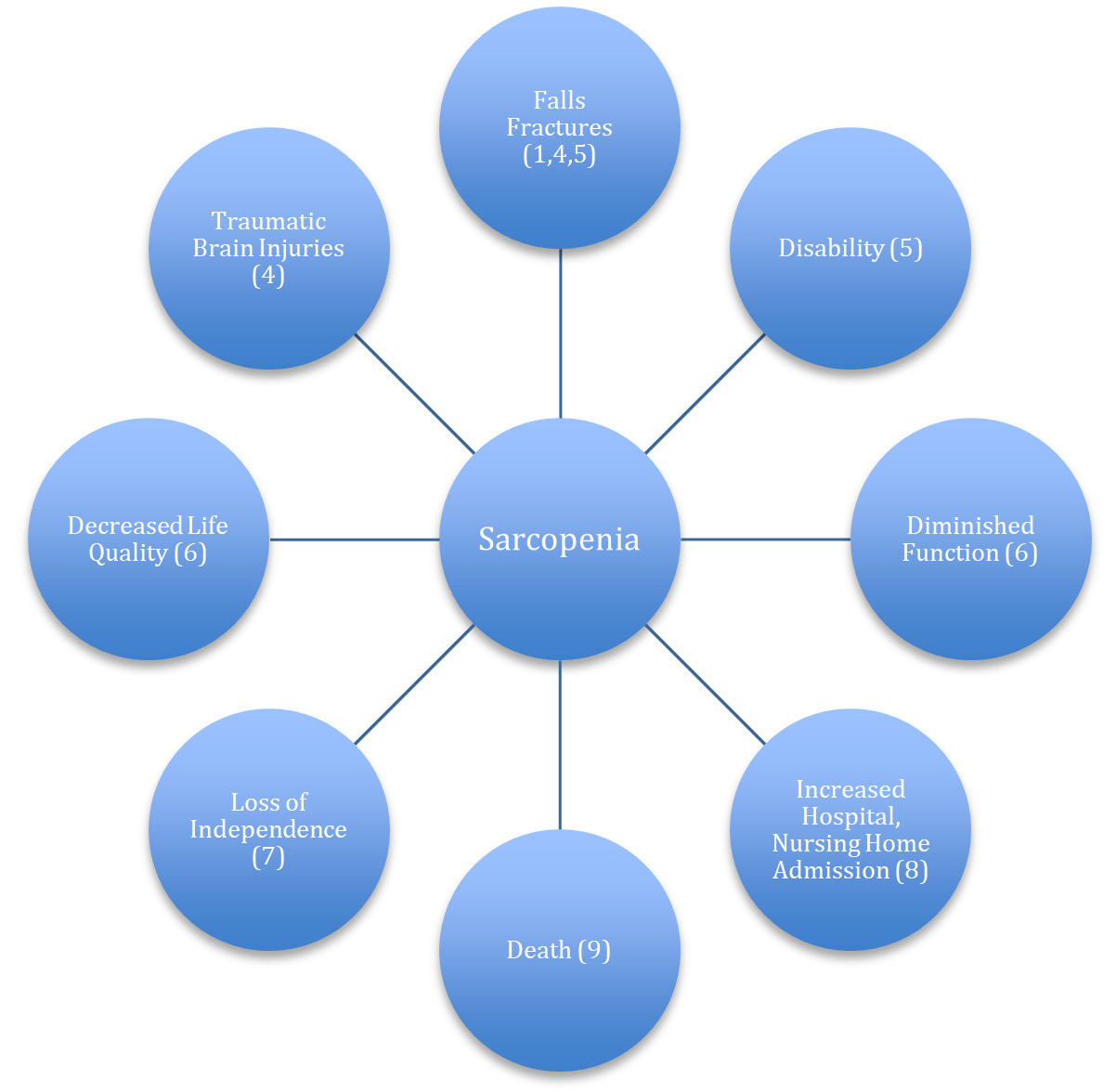
In 2010, a consensus group known as The European Working Group on Sarcopenia (EWGOS) defined sarcopenia as a progressive, generalized loss of skeletal muscle mass and strength with risk of adverse outcomes such as physical disability, poor quality of life and death.1 In the intervening decade additional operational definitions have been proposed,2,3 each unique, but all implicating diminished muscle mass, strength loss, and low physical performance as parameters of sarcopenia. Figure 1 shows the health risks linked to sarcopenia.
Sarcopenia is also associated with a greater incidence of cognitive impairment1 cardiovascular disease4–8 type 2 diabetes7 obesity7 osteoporosis7,8 arthritis8 and depression.9
Discussion
A search of the PubMed, Medline and Scopus data base for the period of January 1, 1995-January 31, 2021 was conducted using search terms sarcopenia, low muscle mass, low strength, low function, assessment and aging. English language papers addressing screening tools, diagnosis, predictive validity, specificity, sensitivity, prevalence and burden related to sarcopenia were incorporated. Papers were included that were pertinent to chiropractors and chiropractic settings. Studies fulfilling inclusion criteria reported on at least one predictive validity measure representing the effectiveness of a screening tool for detecting sarcopenia in older adults. Emphasis was on use of controlled clinical trials evaluating specificity, sensitivity, positive predictive value, negative predictive value and accuracy.
The search criteria identified 36 papers reporting on 5 common screening tools for sarcopenia. Results of the papers are summarized within.
Discussion
Prevalence
The prevalence of sarcopenia has been estimated at 6-24% for adults 50-70 years of age and up to 50% for those over 80.10 Although it’s separate from frailness, sarcopenia is estimated to exist in 50-70% of frail individuals11 and estimated to affect up to 33% of adults in community health settings.7 Targeted muscle loss, which can have a bearing on health outcomes, is common with sarcopenia. The cross sectional area of thigh muscle of sarcopenic adults has been found to be reduced by 40% by the age of 60, increasing the risk of hip fractures by 50-60% independent of bone density.12 Overall the decline of muscle mass between 40-80 years of age has been documented at 30-50%.7
Functional capacity, including the ability to perform normal activities of daily living, an important parameter for maintaining independence, diminishes 3% per year beginning at the age of 60 in sarcopenic adults. Sarcopenic individuals lose an estimated 30% of physical function by the age of 75.7 This loss increases the risk of falls and mortality.13 Older adults with sarcopenia are 2-5 times more likely to become disabled than non-sarcopenic adults.14 The pattern of age-related decline across the lifespan is similar in men and women and independent of race.15
Sarcopenia is a progressive disorder marked by subtle changes that may go unnoticed in its earliest phase. Although many think of it as a geriatric condition, there is evidence that its characteristic muscle wasting, strength and functional losses may begin as early as the third decade16 and become more pronounced in the latter stages of life. Estimates indicate 35% of the U.S. population over age 60 possess a moderate degree of sarcopenia, while 10% over 60 have severe sarcopenia.14
Health Burden
Health care costs directly attributable to sarcopenia have been estimated at $18.5 billion dollars per year,7 which is more than the estimated ($16.3 billion) cost of osteoporosis.17 Indirect costs are projected at $26.2 billion per year. Yearly health care costs attributed to sarcopenia are estimated at 1.5% of total U.S. health care costs.18 As the American population matures loses related to sarcopenia are expected to increase and place an even larger burden on the U.S. health care system.
Risk Factors
Physiological and behavioral risk factors have been identified with sarcopenia. Key physiological factors include chronic inflammation, mitochondrial dysfunction, oxidative stress, diminished hormones, chronic disease18 depressive mood, cognitive impairment19 and a diminished response to anabolic stimuli.14 Behavioral risk factors include inadequate physical activity, obesity, smoking,8 alcohol abuse18 and poor dietary practices.20
Where as it’s possible to preserve a reasonable amount of muscle, strength and function with aging it can be extremely challenging to regain once significant loss has occurred. Consequently early detection may be a key to mitigating sarcopenia and preventing serious health consequences. Based upon varying reference criteria, including the European Working Group on Sarcopenia in Older People (EWGSOP),1 Asian Working Group for Sarcopenia (AWGS),2 International Working Group on Sarcopenia (IWGS),3 an array of screening methods exist for sarcopenia. I review 5 common methods of screening so chiropractors may make early identification of sarcopenia and take appropriate actions to mitigate it’s damage.
Screening Tests
The purpose of screening tests is to rapidly identify those likely to benefit and those unlikely to benefit from additional diagnostic testing. The “gold standard” for diagnosing sarcopenia is a DXA (Dual energy X-ray absorptiometry) scan. But due to cost, lack of portability and limits on assessing obese individuals there is need for simpler screening tools in practice settings. As opposed to a DXA scan a positive screen for sarcopenia is not meant to definitively diagnose sarcopenia but to trigger additional diagnostic testing to confirm a suspicion of sarcopenia.
Screening tests should be valid, safe, cost effective, easily performed, reproducible, possess acceptable specificity and sensitivity and have well defined cut points.21 A variety of tests are available and those chosen depend on the patient (mobile, disabled), availability of technical resources, setting (community, clinic, hospital, research center) and purpose of the testing.21 Following are five screening tests commonly employed with sarcopenia.
SARC-F Questionnaire
The SARC-F Questionnaire is a brief, uncomplicated tool originally developed by Malmstrom22 to identify individuals who require further diagnostic testing for sarcopenia. In this screen, which takes only minutes to complete, 5 elements of a patient’s life are reported on: strength, ambulation, stair climbing, rising from a chair and history of falls. Scores range from 0-10 with 2 points for each component. A score equal to or greater than 4 is predictive of sarcopenia.
SARC-F, which is an acronym for the 5 domains assessed, has become a popular screening tool for sarcopenia. Its acceptance has been advanced by the European Working Group on Sarcopenia20 which recommends use of SARC-F as the first step in screening for sarcopenia. In clinical trials, SARC-F has consistently demonstrated high specificity, giving this tool an effective ability to reject individuals who do not have sarcopenia. However, in a validation study, Woo23 found SACR-F to possess low sensitivity raising concerns it may be unable to consistently identify those who have sarcopenia.
In a recent study24 comparing 4 screening questionnaires, SARC-F identified the least number of subjects as sarcopenic. Despite it’s less-than-optimal sensitivity SARC-F is viewed as a suitable tool for research, experimental observations, large scale epidemiological investigations and as a community screening tool for sarcopenia.21
SARC-Calf
In response to the less than ideal sensitivity of SARC-F, Barbosa-Silva25 proposed a modified version of SARC-F called SARC-Calf. With this assessment participants complete the SARC-F Questionnaire and have their calf circumference recorded. International organizations such as the World Health Organization recognize calf circumference as a sensitive measure of muscle mass in older individuals.26 Comparisons have found this tool to possess superior sensitivity to SARC-F (66.7% vs. 33.3%), higher AUC (0.736 vs. 0.592) and comparable specificity (82.9% vs. 84.2%). Bahat27 also reported adding calf circumference to SARC-F improved the specificity and diagnostic accuracy of SARC-F but did not improve sensitivity.
In a more recent investigation comparing screening questionnaires for sarcopenia SARC-Calf demonstrated highly variable sensitivity (20.0-75%) and moderate diagnostic accuracy.24 The authors reasoned such discrepancies could be due to confounding factors such as obesity, peripheral edema or peripheral vascular disease, which may mask low muscle mass and diminish the reliability of calf circumference measurements. Consequently SARC-CALF may have utility in screening community dwelling older adults for sarcopenia but have limited usefulness in individuals where obesity and other confounding factors are a possibility.
Body Mass Index
Using appendicular skeletal mass data collected on 22,133 subjects in the National Health and Nutrition Examination Survey (NHANES) Goodman28 proposed a screening method based on age related muscle mass and Body Mass Index (BMI). Sarcopenia has been defined in part as low muscle mass, commonly expressed as a skeletal muscle mass index (SMI) less than two standard deviations (SD) below the mean SMI for young adults. In this study low muscle mass was defined as a SMI of 1.0 SD below the mean SMI of the reference population. Using the thresholds of 1.0, 1.5 and 2.0 SD from the reference population the prevalence of low muscle mass for males was 30.9, 24.2, and 14.2% and for females 6.7, 4.4, 0.8%.
Locquet29 analyzed Goodman’s model against 5 diagnostic definitions of sarcopenia and found AUC to range from 0.600 to 0.853. Generally a AUC of 0.5 suggests no discrimination ability to diagnose individuals with and without the condition; 0.7 to 0.8 is considered acceptable; 0.8-0.9 excellent and greater than 0.9 outstanding. With the exception of 1 comparison above (0.853) and 1 below (0.600) the remaining AUC’s identified with the body mass approach fell within a acceptable range.
Although previous studies have identified sarcopenia based on muscle mass, critics note low muscle mass, by itself, may not insure sarcopenia. But may be attributable to smaller body size or to a debilitating condition such as arthritis or neurological disorder.30 Linge31 showed a decrease in the prevalence of sarcopenia with increased body mass index (underweight 8.5%; normal 4.35; overweight 1.15; obese 0.15) direct correlations between body size, muscle quantity and sarcopenia may be complicated by obesity.
SARC-F EBM
In a unique study of 969 community dwelling men and women, Kurita32 compared the effectiveness of SARC-F and SARC-F EBM (Elderly, Body Mass) for identifying sarcopenia in individuals with musculoskeletal disease. In this study SARC-F was administered in it’s standard format while SARC-F EBM examined seven domains. Five are from the original SARC-F questionnaire plus 2 additional domains representing age (E) and body mass index (BM). The maximum score of SARC-F EBM was 30 points. A score of 12 equaled an increased risk of sarcopenia.
The SARC-F EBM outperformed SARC-F demonstrating superior sensitivity (77.89 to 41.7%), better AUC (0.824 to 0.557) and nearly identical specificity (69.6 % to 68.5%) making the SARC-F EBM a potentially more accurate diagnostic screen for sarcopenia especially in cases of musculoskeletal disease. Musculoskeletal disease covers a host of conditions including osteoarthritis, which is a common aging disorder accounting for approximately 7.5% of the disease burden for people 60 years and older.33 Currently, it’s unknown how many individuals with musculoskeletal disease are also afflicted with sarcopenia but 1 study estimated the prevalence of sarcopenia in patients with osteoarthritis at 9.1%.34
In a separate study by Krzymiska35 with community dwelling individuals, use of SARC-F Questionnaire was compared to the SARC-F EBM. Both SARC-F and SARC-F EBM demonstrated good diagnostic accuracy for identifying sarcopenia but SARC-F EBM had superior sensitivity and AUC. Unlike Kurita’s research however, this study did not assess participants for musculoskeletal involvement. Although more study is needed the concept of adding age and body mass index to the SARC-F Questionnaire appears to improve screening for sarcopenia both with musculoskeletal and non-musculoskeletal subjects.
Three Variable Score Chart
Using EWGSOP1 as the reference criteria, Ishii36 assessed 1,971 functionally independent, community dwelling adults aged 65 and older and found the probability of sarcopenia could be accurately charted based upon 3 variables: age, calf circumference and grip strength. In this model the scores of each variable are summed and charted to reveal the likelihood of sarcopenia. With high specificity values the Ishii Model may be particularly adept at ruling out individuals who don’t have sarcopenia making it a promising tool for minimizing unnecessary testing.
In a recent study by Locquet29 the Ishii tool demonstrated higher sensitivity, comparable specificity and better AUC than 4 other tools, leading researchers to conclude it was better at distinguishing those at risk for sarcopenia. Since sarcopenia, is commonly asymptomatic in it’s initial phase, early detection is an important step towards minimizing it’s damage. With improved sensitivity the Ishii Model may be a upgrade over other screening tests for sarcopenia. However, it leaves room for improvement in providing assurance positive cases are not being missed. The Ishii Model also requires calculations that some may find complex and time consuming.
For a synopsis of the methodology, study population, scoring criteria, strength and weakness of the previously reviewed screening tools see Table 1
Conclusion
Sarcopenia is a condition, growing in prevalence that can have profound impact on aging individuals, putting their health and independence at risk and in some instances even resulting in death. Despite it’s magnitude, sarcopenia is commonly overlooked in primary care practice settings.21 As “portal of entry” health care providers, chiropractors are uniquely positioned to employ screening tools that aid in identifying sarcopenia so negative health outcomes can be mitigated. This paper presented a review of sarcopenia screening procedures with the intent of making chiropractors aware of the effectiveness of such tools and alerting them to options they have at their disposal.