Introduction
Muscular Dystrophy (MD) is not a term used to describe a single muscle-related condition but several conditions that cause loss of muscle mass resulting in weakness and mobility.1
There are many forms of muscular dystrophy and despite their being molecularly characterized for easier diagnosis, progress toward their treatment is slow.2 More than 30 forms of MD can now be accurately identified using either genetic or immunochemical methods.3,4 Each form of muscular dystrophy is caused by mutation or a faulty gene that interferes with the production of proteins that form and maintain healthy muscles. The 30 different forms of MD are awaiting treatments. Scientists and researchers are still left wondering about the possibility of designing gene therapy protocols or if the focus will remain on treating secondary manifestations of muscular dystrophy such as inflammation, membrane instability and necrosis.
The classical gene therapy has been used to supply a muscle that has a defective gene with a normal version of the gene. This approach has been rendered difficult to accomplish in practice since available technologies do not support and allow the efficient distribution of such genes to many groups of muscles. New mutations have evolved following the replacement of genes in the genome.5 Little is known about the mechanisms by which even booster genes exert their effects on dystrophic muscle. This is because it is unknown whether these genes can be reproduced with drug treatments.6
Myostatin, the negative regulator of muscle formation has been found to cause muscle hyperplasia and hypertrophy and even fewer connective tissue and less fat in its mutative form.7 The only current treatment that has shown any benefits in human dystrophin deficiency is prednisone.8 It is not until the mechanisms behind boosters are better understood that drugs can be developed to boost muscles in muscular dystrophy and other degenerative diseases. In summary, there is no cure for muscular dystrophy. Most therapies and medications are administered to help manage some symptoms and to potentially slow down the course of the disease.1
In this paper, we discuss a patient who was diagnosed and treated for muscular dystrophy and who decided to seek chiropractic care at the recommendation of his mother when his condition did not improve.
Neurological investigations and interventions at highly accredited medical centers in the country did not resolve his illness. He dropped out of work and was sent home with no hope for future activities but to be bound to a wheelchair for the rest of his life.
After chiropractic care, he began to improve. He subsequently resumed work and is now living a normal life with no significant evidence of muscular dystrophy.
The purpose of this report is to:
-
To share the improvements seen in a patient diagnosed with muscular dystrophy who received chiropractic care.
-
Open doors for research on the effect of chiropractic on muscular dystrophy.
-
Encourage other chiropractors to document and write case studies on the effect of chiropractic on the conditions they see in their practices.
-
To encourage and point patients with muscular dystrophy to the available possible alternative treatments for the condition.
Case report
History
A 23-year-old man who sought care for complaints of low back pain, immobility of lower limbs and neck pain, and arm and neck numbness. He was a welder by occupation but was out of work because of his condition.
He signed a consent form allowing us to use his information as obtained from case history, examinations, radiographic images and treatment protocols for research purposes. The Institution Review Board at Sherman College of Chiropractic approved the study.
The patient first experienced weakness and difficulty walking, bending and sitting due to pain and stiffness when he was 13-years old. By age 19, he realized the seriousness of what was diagnosed as growing pain when he depended on medication to bend, tie his shoelaces, or engage in physical activity like fishing. A neurologist diagnosed him with muscular dystrophy and fearing for the fast progress of the disease, referred him to Duke medical center in Durham, NC for additional evaluation and treatment. After 9-months of treatment using medication (Naproxin™, Tremadol™ and Zanaflex™) and therapy, he received a report indicating that his condition was still progressing, there was no hope of engaging in physical activity and he would ultimately be wheelchair bound for the rest of his life.
At his first visit, he described his pain as constant and an 8 on a 10-cm visual analog scale for both his back and neck pain. His symptoms interfered with his daily activities, work, sleep, daily routine and recreation.
His pain was exacerbated by standing, impact and being still. It affected his sitting, standing, walking, and bending. Lying down, stretching and “cracking his back and neck” as he reported, were palliative.
He was taking Naproxin™, Tremadol™, Nortriptiline™, and Zanaflex™ medications. He indicated on his entry form that he had a history of nervousness, allergies, stiff neck, painful shoulder and elbow, arm numbness, constipation, low back pain, sciatica, leg and hip pain, numbness in legs, poor circulation and hemorrhoids. He could no longer perform his job since it required lifting, pulling, pushing, twisting and bending. He was unable to exercise because of his condition but he was proactive in eating plenty of vegetables, fruits, drinking water and avoiding foods rich in sugar, carbohydrates and fats.
Examination
The static, motion and muscle palpation chiropractic examination revealed fixation subluxations denoting hypomobility in the spine. Locating fixations of hypomobility and laxities of hypermobility is an essential method used in palpation to determine subluxations.9
The following findings were found after chiropractic examination and evaluation of the lumbar spine.
Range of motion: The patient had decreased lumbar flexion (70/90), decreased lumbar extension (20/30), decreased lumbar Right and Left lateral flexion (bilaterally) (20/30), decreased lumbar Right and Left rotation (bilaterally) (30/40)
Muscle testing: Bilateral muscle weakness was noted in the following muscles. Manual muscle testing has reliable validity for patient evaluation of strength and grip.10–12
Splenius Capitis (3/5), RCP Major (3/5), Levator Scapula (3/5), Rhomboids (3/5), Erector Spinae muscles (3/5), Trapezius (4/5), Piriformis (4/5)
He had weak gluteus muscles and was unable to lift and hold his legs in prone position.
Orthopedic examinations
Positive findings and indications were noted bilaterally as follows. Distraction test (+), Cervical compression test (+), Spurlings (+), Straight leg raiser (+), Bragard’s test (+), Kemps (+), Gaenslen’s test (+), Hibb’s test (+), Yeoman’s test (+), Iliac compression (+), Femoral nerve stretch (+)
Other finding included a high right shoulder, anterior head carriage of 1.2" beyond the external auditory meatus to the shoulder point. The headache disability index was measured at 56% with daily headache pain registering 7/10 on the pain scale with 10 out of 10 being the worst possible pain.
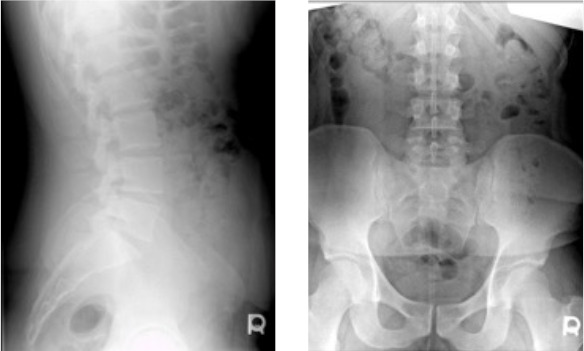
X-Ray findings
There were subluxations in the cervical, thoracic, lumbo-pelvic and sacral spine with evidence of
-
Cervical brachial syndrome—Neck pain typically seen with tingling, numbness and discomfort in the arm, upper back and upper chest. It is usually due to discogenic brachialgia from C5/6 and C6/7 segments.
APOM and Lateral Cervical X-ray views were taken
Facet derangement and imbrication was indicated in the cervical spine at C5-C7, with right tilt and rotation.13
-
Disc degeneration—the wear and tear of intervertebral discs leading to pain, numbness, and tingling along dermatomes of the affected discs.14–16
He had reduced disc height at T12-L1. Degeneration was evident in these areas through thinned out and compressed cortices with osteophyte formation.
-
Lumbo-sacral plexus disorder—Ill functioning of the lumbosacracl plexus resulting in pain in the low back, weakness, pain and loss of sensation in all or some parts of the legs. It may also affect the abdomen, buttocks, thighs, calves, feet and genitals.17,18
Lateral and AP Lumbo-sacral X-rays were taken. The sacrum indicated a right tilt with right rotation malposition.
Intervention
The patient received chiropractic care at a frequency of 3 visits per week for the first 2 weeks, after which visits were reduced for 2 times a week for 4 weeks for the initial plan of care. See table 1 for initial treatment protocols.
Using chiropractic clinic protocols of palpation, examination and X-rays mentioned earlier, subluxations were located at C1, T4, T6, L1 and sacrum.
Correction of subluxations was done via the Diversified method of adjusting19 for the cervical and thoracic spine. Thompson technique,19 using drop table pieces, was used for adjusting the sacrum. The patient was adjusted in supine position for the C1 subluxation and in prone position for thoracic and sacral subluxations. Changes in leg length were observed visually in prone and supine positions. Static, muscle and motions pre-adjustment findings were compared to post-adjustment findings. All orthopedic tests performed on the initial visit were re-assessed at the end of the first plan of care.
A TENS unit was used in the lumbo-sacral area to decrease pain in the acute and chronic stages and increase blood flow in order to facilitate healing of tissues. PNF stretches were also done in office and out of office to activate gluteal antagonistic muscles and stretch Hamstrings—biceps femoris, semitendinosus, semimembranosus, core spine muscles—erector spinae muscles. The patient used a large exercise ball he sat and balanced on for 10 seconds before standing up straight without bending at the waist for 10-15 repetitions. Strengthening exercises—Williams flexion exercises and squats were done too. Superman exercises were included interchangeably. Exercises were done in 3 sets of with 10 repetitions bilaterally.
Outcomes
The aim of chiropractic care for this patient was to correct vertebral subluxations and strengthen paraspinal muscles. After completing the initial plan of care, he did not have any more headaches. His headache disability reduced to 4%. He could also perform other activities he was previously unable to do, including drive, concentrate, lift, sleep and take care of himself.
ROM improved significantly. Cervical extension increased to 50/60, cervical right and left lateral flexion increased to 40/45 bilaterally and right and left cervical rotation increased to 65/80 bilaterally.
Lumbar flexion increased to 80/90 while lumbar extension increased to 30/30. Lumbar left and right lateral flexion increased to 30/30 bilaterally as lumbar right and left rotation regained normal range of 35/40 degrees.
The patient reported a pain decrease to 3 out of 10 in both his neck and back.
Muscles regained strength bilaterally to: Splenius Capitis (5/5), RCP Major (4/5), Levator Scapula (5/5), Rhomboids (5/5), Erector Spinae muscles (5/5), Trapezius (5/5), Piriformis (5/5)
Orthopedic tests were re-evaluated with the following results seen bilaterally.
Distraction test (-), Cervical compression test (-), Spurlings (-), Straight leg raiser (-), Bragard’s test (-), Kemps (-), Gaenslen’s test (-), Hibb’s test (-), Yeoman’s test (-), Iliac compression (-), Femoral nerve stretch (-).
Anterior head carriage showed ½" reduction. There was sigificant change from his initial posture and gait as he was able to stand, walk and perform tests on his own as directed after the treatment.
The patient did not show evidence of vertebral subluxations through the static and motion palpation analysis performed.
After the initial care protocol and the significant improvement seen, the patient’s visits were reduced to one time a week while maintaining the protocols seen in table 2.
At the end of the 2nd treatment plan, the patient reported that he could take care of himself, sleep, read, drive, walk, fish and lift up to 10 pounds of weight without any trouble. He had no more headaches. His Headache Disability Index reduced to 1%. We shifted him to maintenance care, where follow-up treatment visits were schedule once every 2 weeks.
Discussion
How Does Chiropractic Fit In?
Many patients visit chiropractic offices with musculoskeletal ailments. However, muscular dystrophy is not a common ailment seen by chiropractors. This disease, caused by “a mutation or flaw,” results in defective, insufficient, or missing proteins needed for normal muscle functions in the body. The body contains a protein called rapsyn needed to link the communication between the brain and the muscles of the body. This means that certain fully functioning receptors must be in specific places for this communication to occur.20
Chiropractic is a healthcare profession that for some focuses on locating, analyzing and correcting vertebral subluxations. Subluxations are defined by Stephenson as a condition of a vertebra that has lost its proper juxtaposition with the one above or the one below, or both; to an extent less that a luxation; which impinges nerves and interferes with the transmission of mental impulses.21
Misalignments of the spine cause a vertebra to move out of its juxtaposition in relation to the vertebra above or below to the extent that it alters the biomechanical and physiological functions of surrounding structures, leading to impairment or loss of function.
Vertebral subluxations are recognized as a biomechanical lesion of the spine by the World Health Organization.22
Chiropractic has focused on the correction of vertebral misalignments while advocating for the body’s natural ability to heal itself. Chiropractic sees the human body as possessing great ability and potential to restore bodily functions once it is cleared from subluxations that alter neurology and compromise communications between the brain and targeted endpoints in different tissues.
Vertebral subluxations are identified using a combination of pathophysiologic indicators of spinal dysfunction.23
Application to the Case
The patient came with a diagnosis of Muscular Dystrophy from a reputable hospital. He had dropped out of work because of back pain and acute muscle weakness. Muscular dystrophy had been diagnosed through a series of enzyme tests, physical exam and case history findings from the hospital prior to chiropractic care.
He was evaluated for subluxations, which were found in the cervical, thoracic and sacral areas. Orthopedic and diagnostic images were also used to ascertain and confirm chiropractic diagnoses.
The principle aim of chiropractic care for this patient was to correct vertebral subluxations using Thompson and Diversified specific techniques.
Chiropractic adjustments were given, beginning with low force, to the tolerance of the patient knowing he was in pain and his muscles were weak. PNF stretches, passive modalities and rehabilitative exercises were done alongside the chiropractic care.
The combinations of correcting vertebral subluxations with physiotherapeutic procedures like stretches and rehabilitative exercise were successful in reducing the patient’s pain, restoring muscles strength and restoring neurological and physical functions. He resumed work after believing he would never work again. The adjustments significantly improved his range of motion in the cervical, lumbo-pelvic and sacral spine. Therapeutic modalities strengthened muscles and improved their tone.
In this case, observed changes in leg length were noted both in supine and prone positions following the correction of vertebral subluxations. Such changes indicate and suggest the occurrence of a neurological change following chiropractic adjustments.
One limitation in this case study is that follow-up diagnostic images were not taken and neither was the patient re-evaluated at the initial facility where he was diagnosed. He was so happy to start living a normal life and to resume work that he did not wish to undergo further evaluations.
Possible Benefits of This Report
-
Highlight the effects of chiropractic care in conjunction with PNF stretches, passive modalities, and rehabilitative exercises on a condition that does not have a definite treatment.
-
Open doors for research on the possible effects of chiropractic on muscular dystrophy as we walk toward finding a cure for this deadly disease.
-
Encourage other chiropractors to document and write case reports on the effect of chiropractic on the conditions they see in their practices.
-
Show the effect of chiropractic on a patient diagnosed with muscular dystrophy.
-
To encourage and point patients with muscular dystrophy and other illness for which there is no cure to try available alternative treatments.
-
Encourage collaboration between other health care practitioners and chiropractors through referral, co-management and research on conditions such as muscular dystrophy.
-
Promote the scholarly activities of chiropractic institutions.
Conclusion
Our patient, initially visited us with a medical diagnosis of muscular dystrophy. Despite medical intervention, a series of exacerbations led to intense back pain and loss of function and use of his limbs. He had severe neck and back pain and lack of mobility. He received chiropractic adjustments to his cervical, thoraco-lumbar and sacral spine along with physical therapy and therapeutic exercises for 12 weeks. He reported significant improvement of his condition,measured by functional outcome assessments (the neck and back indexes), patient perception outcome assessments (patient satisfaction measures) general health outcome assessment, physiological outcomes (Range of motion, muscle function, reflexes, subluxation syndrome—asymmetry or hypertonic muscle contraction, soft tissue compliance and tenderness, abnormal segmental motion assessed radiographically)
It is important for practitioners to be aware that chiropractic adjustments for muscular dystrophy can be controversial, and there is no literature showing that manipulative treatment is a method of choice for this condition. However, this case shows that muscular dystrophy may show favorable response to a combination of chiropractic, physical therapy, and rehabilitative exercises. One shouldnot infer this would be successful for any other patient with muscular dystrophy as one cannot generalize from a case report.
WE recommend that additional research be conducted in collaboration with other doctors who can do post adjustment clinical evaluations to ascertain the presence or absence of muscular dystrophy.