INTRODUCTION
Harrison presented a systematic method for categorizing postural displacements as translations or rotations of the head, thorax and pelvis.1 For lateral thoracic translation postures, the spine adopts an 'S-shape, where the lower lumbar segments laterally bend toward the lateral shift and the upper lumbar and lower thoracic segments laterally bend opposite the lateral shift, bringing the spine back to a vertical orientation.2 This is the normal spinal coupling pattern expected from a ‘pure’ translation posture and as demonstrated by case report3 and clinical trial4 may be amenable to reduction.
In the scientific literature, spinal asymmetry in the coronal or frontal plane is traditionally known as ‘trunk list.’ The aging spine is also associated with degenerative changes5 including in those with degenerative scoliosis which may occur with coronal offset.6 A lateral translation posture in the aged spine may not be as flexible and may not be able to display the describe ‘S’ shaped spinal coupling and instead be seen as a left or right postural ‘lean’ in the coronal plane.
Coronal balance is well studied in those with scoliosis, where it is known that lateral malalignment with an offset greater than 3cm in the direction of the concavity of the scoliosis is associated with a significantly greater negative clinical impact.7 In another study an average coronal imbalance of 25 mm correlated with poor vitality on the short form-36 Health-Related Quality of Life (HRQOL) questionnaire in adult degenerative scoliosis patients.8
The purpose of the present series is to discuss 5 cases in which reduction of coronal plane spinal subluxation helped improve back pain, disability and HRQOL after corrective treatment in older patients with degenerative disc disease.
CASE REPORT
This is a retrospective case series featuring the reduction of coronal plane, lateral thoracolumbar spine translational offset postures (subluxation) in older patients with degenerative disc disease. The inclusion criteria included: 1) degenerative disc disease; 2) a lateral translational offset of the thoracolumbar spine as measured from either T1 or C2 as compared to S1 or L5; 3) chronic back symptoms (>3 months) to ensure the lateral subluxation was not a temporary acute antalgic posture; 4) greater than 50 years of age; 5) patients who underwent treatment for their coronal misalignment.
All patient anterior-posterior (AP) radiographs were assessed using the modified Risser-Ferguson method of measurement9,10 consisting of estimation of the centroid of each vertebra with a best fit line to approximate the spinal alignment. This method was chosen as these patients did not exclusively have scoliosis warranting the Cobb angle of measurement. Although some had moderate scoliosis, most simply had a ‘lean’ to the left or right not due to muscle spasm (not an antalgic posture). This measurement method has good to very good inter- and intra-rater reliability.9,10
All patients underwent treatment to correct the coronal plane deformity. Chiropractic BioPhysics© (CBP©) methods3,11,12 that incorporated opposite lateral translation exercises, spinal adjustments, and spinal traction were employed in the attempt to reduce the deformities. CBP technique methods are an evidence-based approach to postural disorders that incorporates corrective ‘mirror image©’ postural exercises, spinal adjustments and spine traction in the opposite of the presenting posture misalignment. For this series, an opposite lateral displacement of the spine and torso was the corrective approach for these patients.
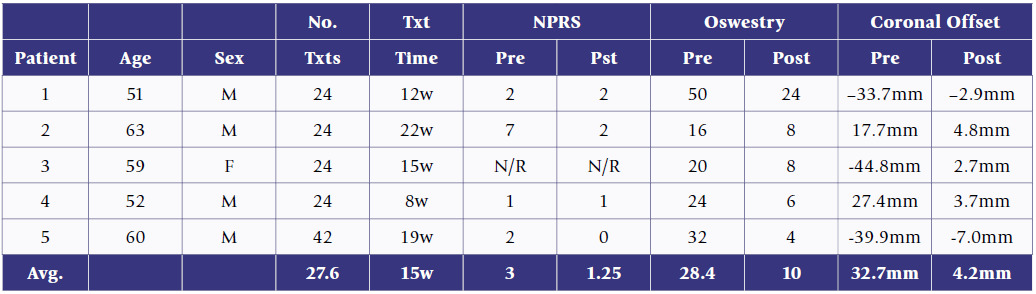
Specifically, all patients performed exercises, adjustments and traction in the office as well as home exercises. The exercises consisted of a right or left thoracic translation on a vibration platform (Powerplate®, Performance Health Systems LLC, Northbrook, IL, USA) for a 2-minute duration (Figure 1).13 Each repetition was held for 5 seconds with a 1-second rest. Prescription of home exercises were also given at a frequency of 100 per day. All patients received manual adjustments which consisted of thoracolumbar spinal manipulation and application of a hand-held instrument (Impulse®, Neuromechanical Innovations, Chandler, AZ, USA) to the paraspinal muscles while positioned in the mirror image posture (i.e. torso positioned left or right relative to the pelvis) while laying prone on an adjusting table. All patients were placed in the Meyer’s wall traction unit (Circular Traction Supply, Inc., Huntington Beach, CA, USA) which stressed the spine to the left or right relative to the pelvis in a standing or seated position (Figures 2 and 3). Each patient worked up to a maximum of 12 minutes in the wall unit. Two patients were seated (Patients 3 and 4) and three were positioned standing in the wall unit (Patients 1, 2 and 5). The patients who were seated could not tolerate standing due to getting either light headed and/or having difficulty with the intensity of standing traction. A summary of the patient data and results are shown in Table 1.
Results
Case 1
A 51-year-old male (185cm, 141kg) presented with a chief complaint of low back pain (LBP) and secondary complaints of numbness in the feet, cold feet, ankle pain, mid-back cramping, heartburn, neck pain and stiffness, as well as allergies.
He had an observable right thoracic upper body translation. Static palpation revealed hypertonicity, tenderness upon palpation, and motion restriction at right T5, right sacrum, left L2, left L5, right T12, right C7 and left C3. The patient also had positive signs for the orthopedic tests of Soto Hall for LBP, Kemp’s test bilaterally and Yeoman’s test on the right. Muscle testing showed a 4/5 for knee flexion on the left and right. Range of motion testing demonstrated lumbar flexion, extension, bilateral lateral flexion and rotation showed restriction and elicited pain throughout the entire lumbar spine region. Reflex testing showed the right patellar and left Achilles’ reflexes were diminished (1+). Dermatome sensory testing showed that areas associated with L4, L5 and S1 showed hypoesthesia on the left.
The AP thoraco-lumbar X-ray showed a right whole spine translation and lean of 33.7mm (Figure 4). There was a mild degenerative left lumbar scoliosis in the lower lumbar spine from L3 to L5 (18.5°) with a compensatory opposite right curve from T12 to L3 (10.3°). The spine cephalic to the curves was straight with a lean to the right.
The patient received 24 treatments over 12-weeks (3/26/20 – 6/24/20). The patient performed left sided exercises (Figure 1) and standing traction with a pulling strap located at T8 and L2 (Figure 2). The post-treatment reassessment showed static palpation hypertonicity, point tenderness, and motion restriction at C2, T4, T10 and L4. Lumbar and sacroiliac joint orthopedic tests were negative. Muscle testing was WNL. Lumbar ROM was WNL. The right patellar (1+) and left achilles (1+) deep tendon reflexes were diminished. The left S1 dermatome showed hypoesthesia.
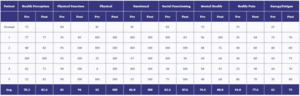
There were notable improvements in physical functioning and bodily pain on the Short-form HRQOL questionnaire (SF36: Table 2), reduction on the Oswestry low back pain disability index (OSW: 24% vs. 50%), the average pain intensity (NPRS: numeric pain rating score) was reported to be at 2/10. The patient reported a 100% improvement in numbness in the feet and heartburn, a 90% improvement in migraines, an 80% improvement in cold feet, a 70% improvement in LBP and ankle pain, a 50% improvement in mid back cramping, and a 40% improvement in neck pain and stiffness. The was no reported improvement in allergies. The post X-ray (Figure 4) showed a dramatic reduction on coronal balance (2.9mm right vs. 33.7mm right) as well as a reduction of the lower lumbar scoliosis (L3-L5: 7.5° vs. 18.4°). The upper lumbar scoliosis curve remained stable (T12-L3: 10.5° vs. 10.3°).
Case 2
A 63-year-old male (178cm, 95kg) had right rib pain, and secondary complaints of neck pain, constipation, pain at the base of the skull and left thumb pain. Static palpation revealed hypertonicity, point tenderness, and motion restriction at C3, T2, T7 and L4. Lumbar ROM showed restriction on all movements without pain. Dermatome testing showed hypoesthesia on the right along the T1-T4 dermatomes, and bilaterally along the L5 and S1 dermatomes.
The AP thoraco-lumbar x-ray showed a T1-S1 translation of 17.7mm to the left (Figure 5). There was visible degeneration at multiple intervertebral levels. The patient received 24 treatments over 22-weeks (2/25/20 – 7/7/20). The patient performed right-sided exercises (Figure 1) and right-sided standing traction (Figure 2) with the pulling strap located at T12.
Upon re-assessment visual posture looked symmetrical in the frontal plane. Static palpation revealed hypertonicity, point tenderness, and motion restriction at C4, T6, and L3. Lumbar ROM was WNL. There was only hypoesthesia present for the S1 dermatome on the right.
Notably, there was a significant improvement in bodily pain on the SF36 (80 vs. 48) (Table 2), improvement in the OSW (8% vs. 16%), and decreased average pain on the NPRS (2/10 vs. 7/10). Overall, the patient noted a 100% improvement in the right rib pain, a 70% improvement in the neck and base of skull pain, and 50% improvement in constipation and left thumb pain. The post-X-ray (Figure 5) showed a reduction of the left translation (4.8mm vs. 17.7mm).
Case 3
A 59-year-old female (160cm, 57kg) reported with a chief complaint of left sacroiliac joint pain and secondary complaints of LBP, numbness into the right 3rd/4th toes, plantar fasciitis, right-sided neck pain and a tingling into both hands. Static palpation revealed hypertonicity, point tenderness, and motion restriction at bilaterally at L2-L4, on the right side of C3-C4, bilaterally at C4 and on the right of T6-T9. Orthopedic tests were positive for Jackson compression localized on the left, maximal compression radiating into left side, cervical distraction relieved pain, Kemp’s tests to the left and right produced bilateral back pain, straight leg raise was positive on the right, and Hibb’s test was positive on the left. Cervical ROM had overall lack of mobility but no pain. Lumbar ROM was severely restricted with pain on flexion, extension and for left lateral flexion. Muscle testing showed weaknesses on cervical flexion (3/5), cervical extension (4/5), cervical lateral bending to the right (4/5), left hip flexion (3/5) and right hip flexion (3/5).
Deep tendon reflexes were diminished for the left and right patellar (1+). Hypoesthesia was noted bilaterally for dermatomes L4, L5, and S1. There were muscle contractures noted for the gluteus medius and hamstrings.
Initial X-ray showed a C2-S1 right shifted coronal imbalance of 44.8mm (Figure 6). The patient also had a right T10-L2 thoracolumbar scoliosis curve of 19.5° with noted degenerative changes at levels L3 to S1.
The patient received 24 treatments over 15-weeks (1/25/19 to 5/17/19). The patient performed left-sided exercises (Figure 1) and seated traction (Figure 3) with the pulling strap located at T12. Re-assessment showed visual coronal symmetry of the posture. Static palpation revealed hypertonicity, point tenderness, and motion restriction bilaterally at L3 and T4 and to the right of C3-C4. The only positive orthopedic test was maximal cervical compression which radiating pain into the left side. Cervical and lumbar ROM was WNL. Muscle testing was WNL. Reflexes were diminished for right and left patellar (1+). Sensory testing was WNL. The OSW showed improvement (8% vs. 20%) and the SF36 indicated notable improvements in the physical, emotional and bodily pain categories (Table 2).
The patient reported a 100% improvement in plantar fasciitis, a 90% improvement in tingling into the hands and numbness into the right toes, a 60% improvement of LBP and a 50% improvement of right-sided neck pain. The post X-ray (Figure 6) showed a reduction in coronal balance (2.7mm left vs. 44.8mm right) and a reduction of the T10-L2 thoracolumbar scoliosis (11° vs. 19.5°).
Case 4
A 52-year-old male (165cm, 68kg) had an acute episode of chronic LBP and secondary issues included cramping in the right inner thigh, pain radiating into the left leg, cold feet and hands, right mid back pain, occasional neck pain, tinnitus and double vision. The patient initially presented in an antalgic posture that was treated until non-antalgic and then corrective care was given to reduce to chronic asymmetric lean.
He had an observable thoracic translation to the left. Static palpation revealed hypertonicity, point tenderness, and motion restriction at C5, T5 and L5 bilaterally. The straight leg raise was positive on the right and left. Lumbar ROM was restricted in all directions with pain. Reflex testing showed the left achilles to be diminished. Sensory testing showed hypoesthesia along the L4 dermatome on the left.
Radiographic assessment showed a thoracic translation of 27.4mm to the left, a left thoracic scoliosis (T1-T12) of 21.8° and a right lumbar scoliosis (L1-L5) of 19.5° (Figure 7). Also, it was noted the patient had a shorter right leg by 16.5mm (Figure 8). Due to the patient presenting with an acute antalgic posture, 6 treatments were given consisting of spinal manipulation, low-back proprioceptive neuro-facilitation stretching, hip ROM and mobility exercises on the PowerPlate. After these treatment sessions the patient reported to feel well and new X-rays were taken with the patient standing on a 12mm heel lift under the right foot (Figure 7, Figure 8). The posture was still deviated 24.5mm to left (at level of T6), the scoliosis curves reduced for the thoracic (14.3° vs. 21.8°) and lumbar (8.1° vs. 19.5°) curves. The patient received a further 24 treatments of corrective care over 8-weeks (8/2/18 to 10/5/18) performing exercises (Figure 1) and seated traction (Figure 3) to the right with the pulling strap located at T12.
Upon re-assessment the patients posture visually looked significantly more symmetric. Static palpation revealed hypertonicity, point tenderness, and motion restriction at C7, T8 and L4. Orthopedic tests, ROM, muscle reflexes and dermatome testing were normal. There was significant improvement on the ODI (6% vs. 24%). Although average pain intensity was reported to remain a 1/10, the ‘worst’ pain rating improved significantly (3/10 vs. 8/10). The patient scored notable improvements in physical wellbeing, social functioning and bodily pain on the SF36 (Table 2). The patient reported a 90% improvement in LBP, left leg sciatica and double vision, an 80% improvement in right inner thigh cramping, right mid back pain and neck pains, a 50% improvement in cold feet and hands, and a 20% improvement in tinnitus. The post X-ray (Figure 7) showed a significant reduction of the coronal deviation (7mm vs. 24.5mm to left at level of T6) and a significant reduction of the thoracic (4.7° vs. 21.8°) and lumbar (2.6° vs. 19.5°) scoliosis curves.
Case 5
A 60-year-old male (167cm, 83kg) had a primary complaint of left sacroiliac joint pain and secondary complaints of neck pain and stiffness, numbness in hands at night, weakness in grip, ringing in ears, allergies, weakened immune system, left rib pain, acid reflux, lower back pain, cramps in legs and feet.
The patient had an obvious right thoracic translation posture. Static palpation revealed hypertonicity, point tenderness, and motion restriction at the left occiput, right C3, T1, and T5, and left T8, T12, L3 and left sacrum. Orthopedic tests demonstrated Jacksons and maximal compression was positive bilaterally, cervical distraction relieved pain, left and right Kemps elicited pain bilaterally, Patrick’s elicited pain to the ipsilateral hip on both the right and left sides and Nachlas was positive on the left for thoracic pain.
Muscle testing showed weakness (4/5) in cervical extension, bilateral rotation, and bilateral lateral bending, as well as left wrist flexion, right and left finger abduction and right and left knee flexion and extension. Cervical ROM was restricted in all directions but without pain. Lumbar ROM was restricted in all directions with pain elicited in all but flexion movement. Hypoesthesia was found bilaterally for the L4, L5 and S1 dermatomes.
The AP thoracolumbar X-ray showed a 40mm right thoracic translation shift (Figure 9) and a severe unleveling of the pelvis (Figure 10). The femur head on the right was measured to be 18.2mm lower than the left, and measured from the line congruent with the sacral base, the pelvis was 23.7mm lower on the right. To address this, a 21mm right heel lift was prescribed and a follow-up X-ray with the lift showed a dramatic reduction in pelvic obliquity (4.8mm lower right pelvis; 0.3mm lower right femur head) (Figure 10). A re-X-ray of the AP thoraco-lumbar spine with the patient standing on the 21mm right heel lift showed a 10mm reduction in the coronal imbalance, though it remained significant at 29.7mm (Figure 9). The patient was prescribed a 12mm lift to be worn inside the right shoe and the patient had their footware built-up 12mm from the bottom of the right sole. The patient received 42 treatments over approximately 19-weeks (3/9/20 to 7/31/20). The patient performed left sided exercises (Figure 1) and standing traction (Figure 2) with the pulling bands located at T7 and T12 levels.
Upon re-assessment the patient’s coronal imbalance was visually much improved. Static palpation revealed hypertonicity, point tenderness, and motion restriction at C2, T8 and L3. All ROM, orthopedic, muscle, reflexes, and dermatome testing were WNL. There was significant improvement in ODI (4% vs. 32%), average pain intensity (0/10 vs. 2/10), and notable improvements in the categories of health perception, emotional wellbeing, social functioning, mental health and energy/fatigue on the SF36 (Table 2). The thoracic translation was significantly reduced (7mm vs. 40mm) (Figure 9).
DISCUSSION
This case series demonstrates that coronal plane lateral translation postures (i.e. global coronal imbalance) can be reduced in older patients with degenerative disc disease. All 5 patients experienced a reduction of symptoms and all tolerated the treatment protocol without any adverse events.
It is important to distinguish that the lateral postural lean in these cases were not typical of a lateral thoracic translation posture as the thoracolumbar spinal coupling was not in the typical ‘S-shape’ pattern that would be expected from a pure lateral translation posture of the thorax.2 Although 3 of the patients also had scoliosis (Cases 1,3,4), the spine had minimal segmental vertebral rotation as expected with mild scoliosis curves. Indeed, the spine coupling in these 5 patients largely involved a coronal lean orientation.
Despite not representing typical lateral thoracic translation,2 opposite sided corrective procedures resulted in an average reduction of 29mm of coronal imbalance towards the midline. In the Harrison trial, 63 consecutive patients with back pain and lateral thoracic translation showed an average of 8 mm correction in coronal imbalance after 36 treatments over 11.5 weeks.4 The average number of treatments in these 5 cases was 28 over 15-weeks and therefore shows a greater average reduction to that reported in the Harrison trial. There may be important reasons for this, such as older patients in this series (average age 57 vs. 39 years in Harrison) having stiffer spines, and stiffer spines may actually be amenable to greater responses to the traction protocols. Other reasons for the greater differences in this series may be due to upright spinal traction versus supine lateral traction as performed in the Harrison trial; it can be argued that upright traction may be more efficacious as it would involve more musculoskeletal reflexes versus in the supine position where the muscles would be relaxed.
As mentioned, coronal symmetry is a requisite for good clinical outcomes, for example in those with concomitant scoliosis.7,8 Asymmetry of the spine may progress, over time, simultaneous with degenerative spine processes. It also may progress due to inactivity in older persons similar to the trend shown to occur in thoracic hyperkyphosis patients.14 Thus, spinal exercises, we suggest should be part of a whole spine rehabilitation program to treat coronal postural disorders in older patients.
Coronal imbalance in surgical circles is considered by some to be a coronal plumbline offset of 40mm15 and by others an offset of 30mm.16,17 As mentioned, an average coronal imbalance of 25 mm was found to be associated with reduced vitality in a group of patients with lumbar degenerative scoliosis.8 As suggested, and discussed recently,18 adult spinal deformity is a biomechanical disease entity that often leads to surgery, but many non-surgical manual therapists assess and treat these patients. Successful methods to reduce adult spinal deformity are required and the procedures illustrated in this patient series show promise in reducing coronal imbalances.
The average coronal offset in our sample was 32.7 mm, ranging from 18-45 mm. It is important to note that thresholds of spinal deformity to surgeons are likely greater than thresholds for treatment from non-surgical manual therapists.18 Indeed, patients resorting to surgical consult and subsequent surgery are patients who have endured excessive suffering as many consider surgery as a ‘last option’18 Thus, spine deformity patients presenting with a coronal offset <30-40mm (e.g. 15-30 mm) who suffer from spinal pain, disability and functional issues should be considered for non-surgical structural rehabilitation, as the closer the spine is to the vertical, the easier it should be to reduce it.19 The logical argument is that treating smaller deformities, if successful, would lead to the prevention of larger deformities.
Limitations to this series include a lack of follow-up for all patients. Strengths include use of pain, disability, and HRQOL questionnaires. Further research is necessary to elucidate effective non-surgical treatments for coronal imbalance postures.
CONCLUSION
The case series illustrates that non-surgical spine rehabilitation programs can be effective at reducing coronal plane spinal imbalance; specifically, in older patients with degenerative disc disease with and without mild scoliosis. More non-surgical methods need to be evaluated to treat adult spinal deformity and the Chiropractic BioPhysics® methods as utilized here may prove reliable for older patients with global coronal imbalance.
ACKNOWLEDGEMENT
We thank all patients who gave verbal and written consent for the publication of their treatment results including X-rays.
Conflict of Interest Statement
Dr. Paul Oakley (PAO) is a paid consultant for CBP NonProfit, Inc.; Dr. Deed Harrison (DEH) teaches chiropractic rehabilitation methods and sells products to physicians for patient care as used in this manuscript.