INTRODUCTION
A paradigm shift has taken place in patient education related to pain. Evidence-based treatment of chronic pain supports patient education in the form of biopsychosocial explanations, such as therapeutic neuroscience education (TNE), over pathoanatomical explanations. Therapeutic Neuroscience Education (TNE), a term coined by the Institute for Chronic Pain, is a method of education that emphasizes the science of nerves related to pain rather than tissue pathology. The method helps improves function, decreases pain, and decreases fear in the chronic pain population.1 Pathoanatomical explanations fail to explain why pain continues to exist in spite of the reversal of damaged tissue2 while the biopsychosocial model recognizes the neurophysiological changes related to chronic pain, which include:
-
Changes in sensory amplification2
-
Changes in sensory and motor representation3–5
-
Changes in body images6,7
-
Changes in motor control8
-
Bilateral findings9–11
-
Persistence and amplification of pain2,12
-
The transition from acute to chronic disorders13,14
The latter effects are learned and reinforce following the initial incident and form a maladaptive memory.15–17 The memory couples the previously pain-free movement or activity with pain, resulting in an aversive reflex that is maintained by plastic neurolimbic changes, perpetuating pain.18,19 Current interventions in rehabilitation typically do not address the underlying neuroplastic changes present in chronic pain patients.20 The following represents a case illustrating use of therapeutic neuroscience education as a rehabilitation intervention. The purpose of this case is to inform clinicians about the negative impact the pathoanatomical model of education had on a chronic pain patient, and report a case illustrating reversal of disability using manual therapy and TNE.
CASE REPORT
Presenting Concerns
A 31-year old ambulatory, male sought care at a hospital-based chiropractic clinic to address 10 years of axial low back pain without radiation, bilateral hip pain, right shoulder pain, and intense non-radiating neck pain. All his pain began during the first of 3 military deployments during which he reported multiple blast exposures, 40 to 50 bouts of loss of consciousness, and the loss of his closest friends. When asked what he felt was causing his pain, he replied:
-
“I have really large bone spurs in my hip joints that are digging into my muscles and cutting the nerves.”
-
“I have large bone spurs digging into my muscles.”
-
“I horrible degenerative changes” and “spurs digging into my spinal nerves.”
-
“My orthopedic surgeon told me that I have horrible degenerative joint disease in my hips. It is the worst that he has ever seen.”
-
“I was walking and felt my piriformis snap and nobody has put it back together.”
-
“In my spine, I have horrible degeneration. They told me that I have spurs digging into my nerves which cause my pain.”
Previous interventions included bilateral hip arthroscopy for right labral repair and bilateral femoral acetabular impingement. He reported benefit post-right shoulder surgery; however, the bilateral hip pain increased following surgery. Previous conservative measures of physical therapy, NSAIDS, and hydrocodone provided little to no benefit. His pain state resulted in a marked decrease in physical activity, activities of daily living, activities he enjoyed, quit his occupation, and instead engaged in a sedentary lifestyle.
Clinical Findings
Clinical examination included a thorough history, physical examination, and self-reported outcome measures. His physical, orthopedic, and neurological evaluation were unremarkable; however, he reported diffuse, inconsistent, non-anatomical areas of pain throughout the examination.
Diagnostic Focus and Assessment
The diagnostic focus of this presentation addressed the patient’s central sensitization. Central sensitization is a condition of the nervous system that is associated a heightened sensitivity to pain and touch leading to the development and maintenance of chronic pain.2 Factors predisposing a patient to central sensitization include stress, anxiety, depression, physical trauma, or psychological trauma. His physical examination was unremarkable; however, his comorbidities included anxiety, depression, physical and psychological trauma which contributed to his diagnosis of central sensitization.
Another factor that can lead to central sensitization is fear avoidance.21 As a part of the assessment of this patient’s pain, he completed an FABQ-PA and scored a 24 which is the highest score and suggested significant fear of pain and consequent avoidance of physical activity.22 The reason for his fear was provided in quotes within the presenting concerns. He had withdrawn from all activities including work because of his fear of further damage. His fear and anxiety related to movement provided another threat to his nervous system contributing to the central sensitization.
Therapeutic Focus and Assessment
Treatment of central sensitization involved cognitive approaches to treatment like TNE. In fact, TNE alone produced 20% improvement in disability when compared to education related to anatomical models.1,23–28 Research illustrates limited efficacy related to the anatomical and biomechanical models of pain education24 with some sources noting elevation in patient fear, anxiety, and stress which negatively effects patient outcomes.29–31 The patient exhibited a great deal of fear and anxiety related to the previous pathoanatomical explanation. Therefore, TNE was implemented with the goal of reducing the patient’s anxiety and fear of movement.
Another therapy employed to address fear avoidance in chronic pain patients is graded exposure. The idea is to expose the patient at a diminished level to the direction they are afraid to move in. Successful application of graded exposure provides the patient with evidence to support the safety of the movement reinforcing the lack of tissue damage. The patient possessed fear of all movements; therefore, use of manual therapy was used to provide a bridge to towards active care. Active therapy was then introduced in a graded, non-threatening order beginning with diaphragmatic breathing and ending with loaded stretching.
Follow-Up and Outcomes
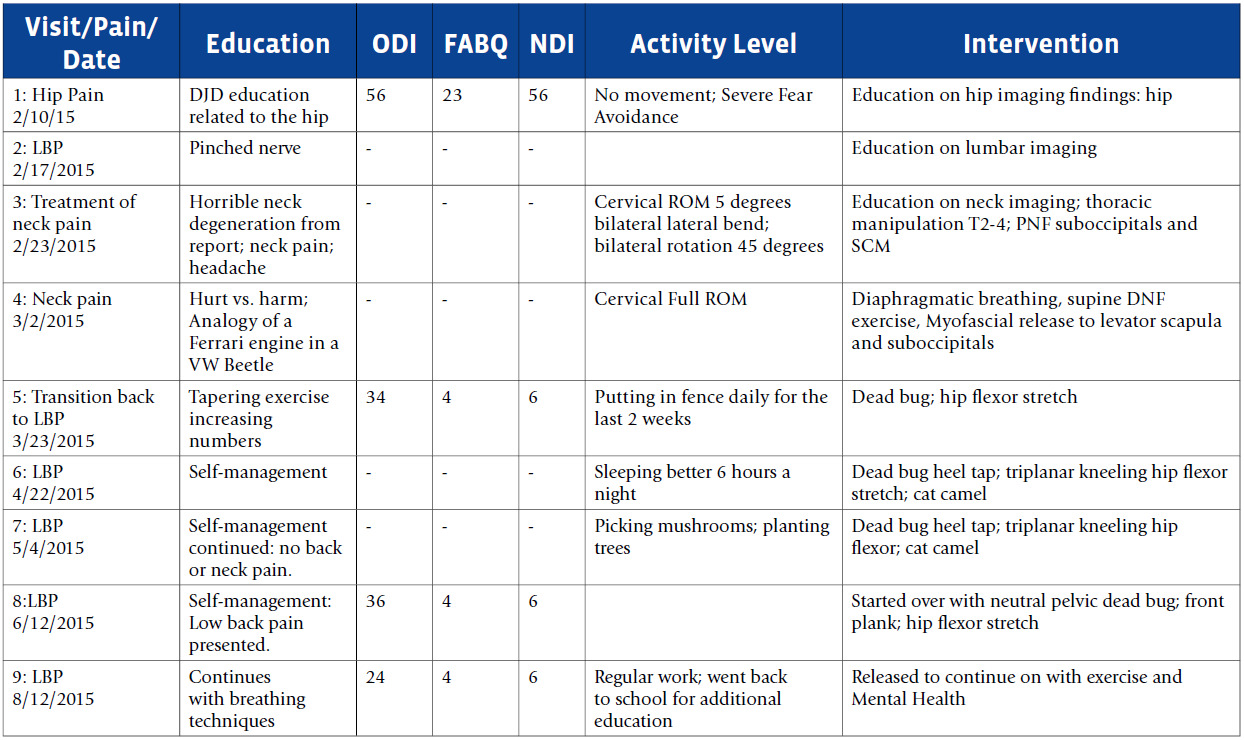
The patient reported once a week for five weeks followed by four additional visits over the next four months. Patient progress was assessed by subjective patient report. Improvements included engagement in fixing a fence, which he previously avoided, sleeping 6 hours a night instead of 3, a return to a favored activity of mushroom hunting, and resumption of college class since he could sit without pain. He was then released from care as he had returned to full pre-injury function per his report. A summary of the provided treatment and outcome measures (Oswestry Disability Index (ODI), Neck Disability Index (NDI), and Fear Avoidance Belief Questionnaire Physical Assessment (FABQ-PA) are presented in Table 1.
The ODI was chosen over the Roland Morris, since the ODI is better at detecting change in seriously disabled patients, whereas the Roland Morris may be more useful in patients with minor disability.32 Clinically significant improvement was deemed to be 10/50 points for the ODI. An improvement of 16 points occurred over the treatment period, indicating significant improvement.33
For his neck pain, the NDI was chosen since it has sufficient support in identifying self-reported disability for neck pain. It is also the most commonly used self-report instruments for evaluating neck pain status in the literature. A 25-point improvement was noted here, again suggesting significant improvement as the minimal distinguishable change is reported to be 5/50 points for uncomplicated cervical pain and 10/50 for cervical radiculopathy, again illustrating significant improvement.34
The FABQ-PA was the third metric that was used to assess improvement. The FABQ-PA assists the clinician in identifying patients with fear related to movement, thus increased risk for prolonged disability. The measure has been correlated with the Tampa Kinesiophobia Scale and Roland Morris Disability Questionnaire. A score of greater than 15 has been determined to be a high risk score. This case illustrated a starting score of 24, which was high risk. During discharge, his score was 6. The treatment provided reduced the patient’s fear of physical activity allowing him to integrate back into the working population.20,22
DISCUSSION
Healthcare providers have many different modalities that they can use for patient care. Therefore, one of the most important aspects of designing a treatment plan is appropriately classifying the patient. Murphy et al illustrate a proposed model for classification that may assist in identifying appropriate modality implementation in the cervical and lumbar spine pain.35 Others have provided additional pain classification systems to assist in evaluating and managing pain.36
In addition to classification, those managing chronic pain need to understand the neuroscience of pain. Educating patients about this has resulted in empowering them to improve and be active.1,31 Treatment plans lacking appropriate education result in tethering of the patient to the healthcare provider and continuing passive care, which may include manual therapy, medications, acupuncture, or other interventional procedures. Verbiage and illustrations that providers use to describe patient pathology impact patient outcomes.23–25 The result of inappropriate education or our patient’s interpretation of the provider’s education related to his presentation resulted in years of unnecessary disability; therefore, it is important that healthcare providers emphasize the neuroscience of chronic pain instead of tissue damage and imaging findings.
CONCLUSION
Our patient her represents a single case; therefore, it is not generalizable. In addition, several modalities including patient education, hip flexor stretching, manipulation, core stability exercises, and breathing instruction were used; therefore, a claim cannot be made related to any one of those modalities. Some view the latter as a limitation; however, the scenario above does provide true representation of a clinic setting; therefore, the above may be more applicable to the clinician than a single intervention study. Also, in the clinical setting the intention is to provide what is needed when it is needed to obtain hasty return to function instead of measuring the result of one intervention.