INTRODUCTION
“Care-at-home” refers to home-based healthcare that provides care to patients at home. The term is often used in the palliative care literature.1 Chiropractic studies have never used this term, and the details of chiropractic care-at-home have rarely been discussed. Instead, the frequently stated term “home-exercise program”2 has a similar meaning. “Care-at-home” in chiropractic can be defined as an extension of chiropractic service in the comfort of patients’ homes. The care-at-home should cover a broader definition that involves patients’ physical, mental, and chemical (nutritional) care. For example, chiropractors can arrange for community assistants to come to patients’ homes and provide care. The chiropractor can provide or arrange hands-on massage or personal rehabilitation programs, advise on pain and symptom control, monitor scoliosis progression, provide emotional and practical support for the patients and their carers at home. They can also involve other specialist professionals in the home care, such as surgical and medication consultation through telemedicine. Although traditional spinal manipulation may not be administered through care-at-home if the chiropractor is not present at patients home, the purpose of care is to provide a range of equipment and services to help patients remain healthy. This could include rehabilitation home adaptations, such as handrails.
The World Economic Forum had described the Covid-19 pandemic and work-from-home had many dangers at home. These dangers are the DEMON – Device addiction, Eye strain, Mental health, Obesity, and Neck3,4 and back pain3,5 – and if left unchecked, can quickly escalate into lifelong challenges. This has altered society’s perceptions of perfect healthcare delivery. During the peak of the pandemic and in the face of widespread social isolation, billions of people worldwide remained confined to their homes. In Australia, a care-at-home program was launched on January 31, 2022, to support those recovering at home with mild COVID-19 symptoms.6 For many, this changed their everyday lives in diverse ways, from how they worked and interacted with others, to their purchasing behavior. One of the most notable consequences of this event was a fresh attitude toward healthcare among many people—one that prioritized patient convenience over everything else.
How “Care-at-Home” is Reshaping Healthcare
“Care-at-home” can reshape the way healthcare is envisioned in patient care. By 2025, an estimated $265 billion worth of care services for Medicare fee-for-service and Medicare Advantage participants might shift from traditional facilities to home-care, accounting for up to 25% of the overall costs of care.7 With favorable demographic and regulatory trends, home care was one of the fastest-growing provider growth areas, even before the pandemic.8 Research suggests that in addition to customer preferences for receiving care-at-home rather than in a facility, care-at-home can provide consumers with higher-quality care at a cheaper cost to health systems.9 Incentives are spreading across healthcare stakeholders to encourage the transformation of more cost-effective and efficient patient care (e.g., site-neutral payments and value-based contracting).10 Recent regulatory reforms by the Centers for Medicare and Medicaid Services are likely to hasten the shift to care-at-home and community-based settings.11 Care-at-home has the potential to change the way chiropractors think about patient care.
How the Pandemic has Catalyzed Care-at-Home
Three pandemic-related factors have catalyzed the rethinking of care-at-home. The invention of new technologies and capabilities, innovation in telehealth and virtual care, and investment in the digital health industry has accelerated the use of care-at-home and altered the architecture of the traditional healthcare system.
Invention of new technologies and capabilities: New technologies are making home care possible for more intensive care. The pandemic has catalyzed the integration of remote patient-monitoring technologies. For instance, the Mayo Clinic used patient monitoring technology for home care in COVID-19 and found that the technology engagement rate was 78.9%, and a multisite remote monitoring program for the management of acute COVID-19 illness was feasible, safe, and associated with a low mortality rate.12 Artificial intelligence (AI) and rule-based systems, such as the New York Medical Group and the University of Hong Kong, have used SpineHRNet+, allowing chiropractors to assess spinal alignment remotely and monitor the progression of scoliosis.13 The system allows the patients at home to take photographs of their back, which creates AI-generated spinal radiographs with calculated angles for chiropractors to monitor the alignment. Chiropractors can prescribe CBP® home-devices to ensure patients’ recovery journey.
Innovation in telehealth and virtual care: A recent study by the U.S. Department of Health and Human Services (HHS) found a 63-fold increase in Medicare Telehealth Utilization during the Pandemic.14 Although there are significant challenges yet to be overcome with these virtual care modalities, growth in this sector has been promising.15 Researchers at the University of Cincinnati (UC) have innovated a way to integrate basic telehealth services into a drone, potentially expanding the bounds of what previous innovators have envisioned with these two technologies individually.16 As chiropractors are primary care physicians, telehealth and virtual care extend the service for patients care-at-home.
Investment in the digital health industry: As larger industry players and insurers are increasingly trying to pivot their existing healthcare offerings into the telehealth space, more communities and patients will have access to remote healthcare services.17
Venture funding for digital health among US-based startups soared to a record $29.1 billion across 729 companies in 2021, nearly doubling the 2020 record of $14.9 million.18 During the pandemic, Lululemon Athletica (NASDAQ: LULU) acquired Mirror, the at-home digital workout platform, for 500 million19 to reach community clients.
Care-at-home May Deliver More Value and Higher-Quality Care
With an annual increase in the aging population,20 stakeholders are looking for new methods to address the persistent COVID-19 dilemma by providing better care. Primary-care visits with telehealth and self-rehabilitative exercises and expert therapist services at home, with remote patient monitoring and support for activities of daily living, could all be part of the solution. These interventions can be delivered to different types and conditions of patients, such as chronic and acute, and throughout the patient journey in diagnosis, treatment plan, and self-care, as either point solutions or as comprehensive offerings.
McKinsey Consulting investigated the existing and future impact of this form of care and generated hypothetical care-at-home journeys for a variety of patient categories.7 By allowing patients to receive care in the comfort of their own homes, care-at-home has the potential to improve the quality of care and patient experience, while potentially reducing preventable adverse health events. Insurance payers, healthcare institutions and chiropractic clinics, care-at-home providers, technology businesses, and investors, among others, might find significant value, although the types of benefits and costs would differ for each stakeholder. Improved quality performance and a more clinically relevant and precise risk classification could potentially add value. However, compensation for care-at-home services and the potential for generated demand through more convenient care may partially counterbalance this benefit. Ultimately, the value of care-at-home will probably be determined by which options are sought and taken.7
DISCUSSION
Chiropractic journeys can begin to define the broader scope of care—one that extends beyond the hospital and other clinical settings into the homes—that they will need to achieve the best quality, outcomes, and experiences for their patients by mapping the various sites and modalities of care that specific patient populations may encounter throughout their care journey.
Before determining how chiropractic care could shift from traditional clinics to home, we shall closely analyze the patient journeys and answer 2 questions. First, where does chiropractic care-at-home fit into a patient’s overall care plan and which would benefit the most—acute condition and pain management, preventative and maintenance care, or specific treatment such as the chiropractic scoliosis protocol?21 Second, which chiropractic patient population does the service assist and would require home care—patients with episodic acute relapse, chronic arthritic conditions, and a history of complicated conditions? The answers can help chiropractors to map out their care-at-home practice needs.
Opportunity for Chiropractic to Unlock the Architecture of Healthcare Model
As the chiropractic profession begins to implement a chiropractic care-at-home strategy, there are several approaches we can find in the healthcare landscape.
Care-at-home subsegments have variable potential for growth and are at various degrees of maturity; chiropractors should identify and prioritize the subsegments and demographics that are their strengths. The pursuit of care-at-home subsegments should correspond with healthcare strategic objectives and growth goals. The choice of patient demographics for home care may have ramifications for value sources. This includes the possibility of reducing healthcare costs through conservative treatment and wellness plans to encourage prevention and avoidance of surgery. For example do the means and capacities required to avoid disease progression or exacerbation differ if the target population is healthy, has stable and treatable chronic degenerative joint diseases; or is fragile and in advanced stages of illness. A risk-based care-at-home model can promote the integration of behavioral healthcare across all stages of the care journey, from preventative to post-acute care, in populations with complicated and multiple chronic conditions. The precise care journeys that health systems select for their care-at-home strategies can also inform their strategic posture toward post-acute and long-term care institutions.
Chiropractic care-at-home strategy should align itself with the mainstream healthcare system with the common goal of patient-centric care, including physical, psychological, and wellness healthcare. Nonclinical determinants of health can be addressed through home and community-based personal care services such as in-home supplement delivery, transportation, and wellness programs. For example, AIA, an AIG-founded Hong Kong multinational insurance and finance corporation, offers an evidence-based wellness program to promote cost management and improve health outcomes. The healthier the choices patients make every day, the more insurance premium discounts and rewards they can enjoy.22 Chiropractic care-at-home may promote health equality and care outcomes since socioeconomic determinants of health are also at the root of health disparities and inequities.
When developing a chiropractic care-at-home plan, chiropractors should understand the role of chiropractic care-at-home in the overall healthcare strategy. They must address the numerous interdependencies with their overall enterprise strategies. While health systems may want to transfer care delivery to the home as quickly as possible to unlock lower-cost, higher-quality, and more effective care, they may require time to set up risk-based agreements and financial incentives that make this transition value-adding. As a result, chiropractors can assess whether to provide in-home treatments in the context of their entire risk-based payment strategy. They might think about a glide path that balances the incentives of the various payment types in which they participate. The characteristics of the health systems’ unique markets and regions, such as demography, payer market dynamics, and the current footprint of brick-and-mortar services, may influence these judgments. Furthermore, because long-term post-acute care will continue to be required to meet patient needs that cannot be met at home, health systems that do not own a hospital, the post-acute footprint will need to decide whether to co-develop their strategy with chiropractors’ partnerships, or to develop chiropractic care-at-home independently of their post-acute strategy.
Chiropractic at home should meet new capability and operating model requirements. Pursuing opportunities will provide new operational hurdles, particularly for chiropractors who have no experience in providing treatments at home. In addition, operating chiropractic care-at-home brings with it unique workforce challenges which differ from those in clinical settings, such as a geographically dispersed, contingent workforce with high turnover management and regional regulations and insurance that limit home care workers. To resolve the challenges faced by workers in the new models, reskilling programs should allow workers to advance into more specialized, higher-paying caring professions or collaborations with tertiary education institutions to teach and educate the future generation of home caregivers. Given these disparities in operating requirements, the chiropractic profession will have to decide whether chiropractic care-at-home should be provided within their present operating service-line paradigm or should be run as a separate division.
Chiropractic care-at-home is affected by an increasingly diversified and fragmented care delivery ecosystem. As these possibilities become more prevalent, there is an unmet need to organize these operations through the creation of new enterprises, acquisition of expertise, or collaboration with other service providers. Many pharmaceutical companies now provide home delivery, recognizing that patients are most likely to choose their preferred pharmacist based on convenience. Diagnostic testing companies are also getting on board with this new ode to convenience.23 Therefore, the project may necessitate a completely new set of capabilities for health systems, such as the ability to collaborate with stakeholders from other sectors of the healthcare industry.
As insurance companies increase their investments in both home-health start-ups and large providers of in-home care and private equity, and venture capital investors fund innovation in care-at-home models and enablers, health systems can gain a competitive advantage by pursuing a programmatic strategy of seeking capital and operating partners to help accelerate their care-at-home agendas.
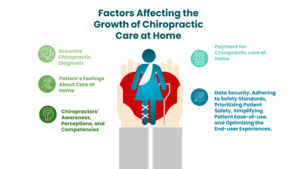
Factors Affecting the Growth of Chiropractic Care-at-Home (Figure 1)
The growth of chiropractic care-at-home services could vary based on several factors. First, an accurate chiropractic diagnosis goes beyond describing symptoms and formulating a diagnosis and treatment plan. Although current telehealth comprises patients discussing their symptoms, demonstrating the problem, and coming up with solutions, there is a limitation of manual treatments for general health, such as scraping therapy.24 As chiropractors often prescribe auxiliary testing or more in-depth analysis on the follow-up appointment, traditional telehealth is yet to determine how to incorporate blood testing, imaging, and the physical exam component into patient encounters, all of which are critical to making an accurate diagnosis. Providers need to evaluate which services can be delivered at home to effectively treat patients’ physical, behavioral, and social needs.
Second, patients’ feelings about care-at-home are critical25 in the adaptation of service. Patients can be informed about the benefits of chiropractic care-at-home and express a preference for it over clinic-based care. Payers can fund particular services to encourage uptake, and clinicians can advocate chiropractic care-at-home to patients when clinically appropriate.
Third, chiropractors’ awareness, perceptions, and competencies may play a role in adaptation. Chiropractors might learn about the potential of chiropractic care-at-home, look into case studies and outcomes of how high-quality care can be delivered at home, and be trained to perform interventions. Payers can play a key role in raising awareness and providing training and instructions.
Fourth, payment for chiropractic care-at-home may influence adoption. As the salary of chiropractors in Hong Kong increased during the pandemic,26 the potential for reduced reimbursement for care-at-home rather than in a higher-cost venue, may be less motivating for chiropractors to pursue chiropractic care-at-home for their patients. Payment parity for telehealth or value-based payment arrangements, for instance, can promote uptake through new reimbursement rules or payment innovations.
Finally, for the new models ensuring data security, adhering to safety standards, prioritizing patient safety, simplifying patient ease-of-use, and optimizing the end-user experiences, are just a few of the potential difficulties to manage. Furthermore, inventors face challenges in scaling the technology in a manner that is both cost-effective and adheres to the highest standards of patient safety and privacy. Technology companies and investors can play an important role in accelerating innovation.
CONCLUSION
The COVID-19 pandemic has been a catalyst in fundamentally reimagining care-at-home to help improve the quality of care and patient experience while also creating potential value for payers, healthcare facilities and physician groups, care-at-home providers, technology companies, and investors. The ultimate value of care-at-home will depend on various factors that are in the hands of stakeholders. However, the opportunity may unlock the current architecture of the healthcare model, providing new roles for chiropractic practitioners to play in providing safe, cost-effective, and well-curated patient journeys.
Funding sources and conflicts of interest
No funding sources or conflicts of interest are reported for this study.