Introduction
Orthopedic testing (i.e., orthopedic exams) is intended to aid in the physical examination of those individuals with potential musculoskeletal impairments to assist in establishing a diagnosis. These tests are typically performed by provocation or alleviation of an individual’s chief complaint symptoms or by influencing the physiologic function associated with the suspected condition. Provocation is often elicited by combining specific maneuvers that are meant to stretch, compress, or resist a potentially tissue. The findings are meant to help guide the clinician toward arriving at an accurate diagnosis. In doing so, a provider is more likely to formulate an appropriate treatment plan, while bettering the probability of attaining maximal patient outcomes.
In most cases, Spurling test compresses neural tissue, thus eliciting patient symptomatology. Named after the prominent neurosurgeon and U.S. Army WWII Veteran, Roy Glen Spurling,1 it was implemented beginning in 1944 for use in the evaluation of “radiculitis,” and originally known as the “neck compression test.” The test has also been referred to as the Foraminal Compression Test, Neck Compression Test, and Quadrant Test. Presently, Spurling test continues to be recognized as a provocative test used in orthopedic examination of the cervical spine.2 Tong and Haig suggest that the original version of the test included the combination of extension and ipsilateral side bending, followed by cervical axial compression.3 The test often involves a combination of cervical motions, with the addition of axial cervical compression. This is meant to intentionally provoke a potentially involved cervical nerve root. These coupled motions are meant to reduce the cross-sectional area of the intervertebral foramen in which a specific cervical nerve root is housed. Tissues and structures that are reported to be pain-generating tissues within the cervical spine pain include facet joints, outer annular fibers of the cervical discs, cervical spine nerve roots, sprained ligaments, bony fractures, and various space occupying lesions within the cervical spinal canal or neuroforamina.4
Throughout formal educational training, prospective healthcare providers are educated on the interpretation of orthopedic test, including tests statistics such as sensitivity and specificity as well as test validity and reliability. Often, the way in which orthopedic examination skills are taught is based upon how they are described within an educational institution’s curriculum textbook. Variations in textbook description leads to variations in test interpretation and performance. In this situation, clarification should be made by the instructor, or a class discussion should ensue, even though this takes time away from the outlined lesson plan. It is the responsibility of health-science institutions to remedy these shortcoming as it pertains to didactic musculoskeletal system examination courses.5
The purpose of this review was to identify variations in a common and valid orthopedic test, the Spurling test, by cross-referencing required textbooks used within chiropractic, physical therapy, allopathic, and osteopathic curriculum. By addressing inconsistencies, we aim to direct future studies towards promoting discipline-wide curriculum uniformity as it pertains to neuromusculoskeletal orthopedic training.
Methods
National Board and Licensing websites for chiropractic, physical therapy, allopathic, and osteopathic medicine were accessed to locate textbooks used in health-profession education. Text concerning the explanation and instruction of Spurling test was then summarized via descriptive statistics, in table format.
The National Physical Therapy Examination (NPTE) samples texts from the PT & PTA Textbook Survey, which aims to maintain a representative group of titles most utilized by accredited programs.6 The National Board of Chiropractic Examiners (NBCE) uses the Special Purposes Examination for Chiropractic (SPEC) Reference Text List.7 Both the National Board of Osteopathic Medical Examiners (NBOME) and the National Board of Medical Examiners (NBME) websites were explored for similar lists of reference texts. For these final 2, since no lists were provided, an ancillary search for textbooks was conducted. Search terms used included “diagnosis,” “physical medicine,” and “orthopedic.”
Following review, each textbook was individually studied for its interpretation of Spurling test. Of those that mention the test, descriptions were evaluated to define the procedure. Trends were categorized and compared for simple analysis.
Results
The mean number of textbooks reported by Physical Therapy programs was 33, and of these, the top 10 reported titles were considered for this study. There were 18 titles reported by NBCE that are used in chiropractic programs across the country. While the search of the considered publishing websites produced numerous e-books and abridged texts, only the 19 full edition desk reference options were considered that were physically available.
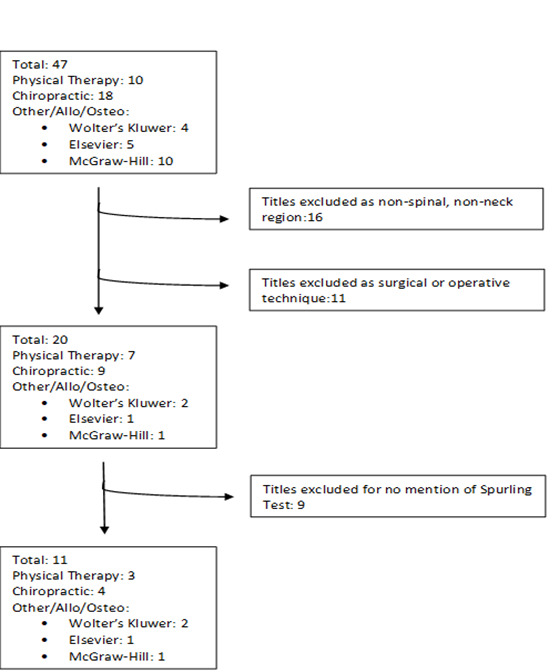
Following initial inquiry, 47 unique textbooks were identified. Here, 20 texts met inclusion for consideration. Textbooks were requested or accessed through university library resources. Textbooks were then examined for their mention of Spurling test. There were nine textbooks with no mention of Spurling test, leaving 11 textbooks for analysis. (Figure 1.)
Text concerning the explanation and instruction of Spurling test was then summarized using descriptive statistics (see Table 1). Table 1 also outlines which healthcare profession the textbook is most commonly assigned. Textbooks were given a designation of “Other/Allopathic/Osteopathic” due to the fact they were not included in either the PT or DC reference lists.
Summary of Spurling Yesty According to Appraised Textbooks
In comparing similarities between the textbooks referenced in Table 1, all include a form of manual axial cervical compression in the attempt to decrease circumferential space of the IVF, which is the essential intension of the test. One textbook goes into greater detail and specifies for how long a practitioner should apply axial compression,10 while another emphasizes the specific amount of force axial compression is to be applied.16 The next most important piece of this test pertains to which standalone biomechanical joint motions were most annotated. Of the 11 texts, 81% included ipsilateral side bending/lateral flexion as part of the examination, while 54% of the sources included extension, and 45% included rotation. Of the 11 texts, only 18% recommend the use of flexion, axial blow, or a neutral starting position. Of note, 1 reference specifically advises against the use of an axial blow.10 As a standalone plane of motion, ipsilateral side bending is most applied, while the most conjoint combination of movements includes the addition of extension and rotation. Of note, the combination of side bending and extension is consistent with the original test version; however, the addition of rotation is not. These results are represented in Table 2.
Discussion
Spurling test was chosen for review due to its robust sensitivity and specificity constructs18,19 promising validity20 and wide use amongst various disciplines within healthcare. One study cites a specificity ranging from 0.89 to 1.00 (95% confidence interval [CI]: 0.59–1.00), with sensitivity varying from 0.38 to 0.97 (95% CI: 0.21–0.99),18 while another concluded Spurling test had a sensitivity of 92% and specificity of 95% with positive predictive value (PPV) of 96.4% and negative predictive value (NPV) of 90.9.19 Validated by operative, magnetic resonance imaging (MRI), and electrodiagnostic findings, Takasaki et al found that functional changes in the foramen cross-sectional area is meaningfully decreased at all segmental levels of the cervical spine when Spurling test was applied. In their version of the test, the cervical spine was placed in the positions of extension (12.79°), rotation (63.36°), and lateral flexion (28.49°), with the addition of a 7kg axial compression force.20 This application most closely parallels Cleland’s “Spurling B,” listed in Table 1.16
Oour findings that ambiguity exists between textbooks included within various health science curricula, as it pertains to their interpretation and instruction of how Spurling test is meant to be performed. This study also makes note as to which textbook a particular health-science program may choose to include in their orthopedic assessment courses. Failure to address the results of these findings may lead to divergences in the way in which prospective healthcare providers apply orthopedic tests where it matters most – clinical practice. In addition, tthis may likely not be an issue unique to only Spurling test, but to other special tests as well. Potential shortcomings, such as these, in healthcare curriculum will lead to less competently trained graduates, inaccurate diagnoses, inappropriate treatment plans, and ultimately poorer patient outcomes. This is however correctable, if recognized. Future studies should ask the question, “what is the best way to apply Spurling test, or any other test for that matter?” It has been suggested in prior research that the combination of extension, ipsilateral lateral bending, and axial compression resulted in the highest visual analog pain scale intensity, the most distally elicited pain, and the highest level of paresthesia.21 Fittingly, this version of the test, is a replication of Dr. Spurling’s original description of what was then called the “neck compression test.” This might suggest that honoring Spurling past, is in fact the best course for the future.2,3 Spurling test is likely just 1 example of many where there is a lack of consistent instruction, teaching, and performance. This provides an opportunity for the continued analysis and critical appraisal of other commonly used orthopedic tests, with the hopes of eventually achieving discipline-wide standardization of neuromusculoskeletal orthopedic assessment training.
Limitations
As no reference list exists for allopathic or osteopathic education, selection bias is likely. Having a reference list, or a study similar to that of the PT and PTA Textbook Survey, would greatly improve method quality. As this is a review of textbooks, no conclusions can be drawn as to the appropriateness of Spurling test in health education or clinical practice.
Conclusion
It is the intention of this study to expose disparities within current recommended textbooks and bring awareness to the fact that these differences will continue to confound clinical education if not sufficiently addressed. Based on this study’s preliminary findings, inconsistencies may exist in the description of Spurling test based upon which reference text is chosen within an institution’s curriculum. Editors and authors alike should take special care to reduce inconsistencies and minimize variability of testing procedures in order to facilitate consistent application that also best represents the current literature. Future studies should aim to parallel what educators are focusing on within their curriculums, with the critical intention of consistently and efficaciously preparing those who will be the future of our healthcare system.