INTRODUCTION
Concussion is now recognized as a mild type of traumatic brain injury (mTBI) causing temporary neurological and neurocognitive alterations.1,2 When a force or impact occurs to the brain, a movement within the brain is initiated. This causes temporary disruption to the cellular membranes and a chaotic release of neurotransmitters within the brain matter.3 Generally, concussions self-resolve within 7 to 14 days.1 High school and collegiate athletes may have an extended recovery time of 21-28 days. Recovery from concussion may be influenced by demographic factors such as gender, age, and previous history of concussion.3 The symptoms reported vary in each individual, making diagnosis and treatment difficult for clinicians. Symptoms may include physical, cognitive, and affective impairments. Physical impairments can include headaches, dizziness, and nausea. Cognition, memory, and attention may also be altered. Affective impairments cause irritability, depression, and anxiety. Symptoms that are least understood are vestibular and oculomotor disturbances. Vestibular disturbances can lead to postural imbalance, altered gaze, visual and spatial orientation defects.4
Concussion is now labeled a public health issue by the Centers of Disease Control and Prevention. Up to 3.8 million sports-related concussions (SRC) are reported every year in the United States. The most recent studies document an increase in SRC incidences in high school and collegiate athletes.2 The most common treatment for concussion is still medication and rest.2 However, the most current research suggests a more active approach to treatment.2 According to the 2015 Pittsburgh TEAM meeting on concussion, the current consensus on approaching concussion is as follows (a) no same day return to play, (b) prescribed physical and cognitive rest until asymptomatic, (c) school/work accommodations as needed, and (d) progressive aerobic exertion-based return to play based on symptoms. Most recent studies have concluded that an active approach to treating concussion is more effective than rest-based approaches.2 Public awareness of concussion has increased in recent years, but clinicians still have many obstacles to face related top diagnosis and treatment.5 The obstacles are due to the complexity and variability of the condition itself.5
This paper describes a chiropractor’s approach to concussion management, using customized, targeted treatment and management following the most recent guidelines indicating that an active approach to concussion is more effective than a rest-based approach. An active and targeted treatment is dependent on the individual’s clinical profile. There are few case reports describing the treatment and management of concussion involving chiropractic care. Concussion is so widely variable and individualized that a one-treatment-fits-all approach may be less effective.
CASE REPORT
This report involves a 17-year-old male high-school football player. On a Friday night (day of injury) at half-time, 1 of the football coaches expressed concerns and asked the team chiropractor to evaluate him. The athlete complained of a headache after he sustained a helmet-to-helmet hit by his opponent during a kickoff return. He reported seeing “green floaters” seconds after impact. The headache was verbally rated 5 on an 10-point scale and was located in the frontal region of the head. The player was visibly distraught and disoriented.
Clinical Findings
Sideline assessment was conducted immediately by the team chiropractor. Reflexes in the upper and lower extremity (Triceps, Biceps, Biceps Brachii, Patellar, Achilles) were 2+. The entire left upper extremity motor strength was 4/5. There was a decrease of light touch sensation in the left upper extremity as well. He had difficulty concentrating when asked to perform finger-to-nose, accommodation, and cardinal fields of gaze. Pupils were responsive and reactive to light. Active cervical range of motion (ROM) was decreased but not painful to perform. The SCAT-5 form from the British Journal of Sports Medicine6 was used for further evaluation. Orientation was 4/5, immediate memory was 10/15, he was unable to recite months in reverse order, and delayed recall was 3/5. After completing the evaluation, he was diagnosed with concussion and was not allowed to return to play. He was advised to follow up with the team chiropractor that coming Monday, 3 days after sustaining the concussion, for further evaluation and management. The athlete, along with his mother, was informed and educated about concussion signs, symptoms, and red flags. A handout was given to he and his mother that presented signs, symptoms, and cognitive and physical limitations. He was informed to rest the remainder of the day and for the entirety of the weekend, with little to no cognitive and physical activity. He was advised to only attend a half day of school that Monday if able.
He followed these recommendations and returned to the chiropractic office on Monday. He reported dizziness when trying to complete homework the previous day, which also caused headache and nausea. He tried to work through the headache and continued to read despite the recommendations to limit activity. He read 3 more sentences and felt an increase in head pain and ran to the bathroom to vomit. His head pain was 6/10 on a verbal rating scale. During his appointment, he stated that he had a dull headache and rated the pain at 3/10. He denied having any neck pain. He noticed that reading, watching TV, and walking aggravated his symptoms. He felt like he had difficulty concentrating, had a slow reaction time, and “didn’t feel right.” He also noticed during gym class that his left arm was noticeably weaker than his right when lifting light weights. He said that he felt 30% of his usual normal.
Examination at this visit demonstrated upper and lower extremity reflexes were 2+. Sensation was intact. Motor strength of the upper extremity was 4/5 for the left arm and 5/5 for the right. Cranial nerves were normal. Cervical ROM was decreased in all ranges with pain during left rotation and right lateral bend. Soto-Hall and cervical compression orthopedic exams caused the headache to increase. Cerebellar exams revealed a loss of balance with eyes closed for both single-leg and tandem stance. Finger-to-nose, Romberg’s test, tandem gait, and diadokinesia testing were normal. The SCAT-5 was repeated and revealed the following deficits: orientation 4/5, immediate memory 10/15, concentration 0/5, 8 out of 30 possible balance errors, delayed recall 1/5. Fascial restrictions were palpated over the cervical paraspinals, Posterior and Middle Scalenes, Upper Trapezius, and Levator Scapulae muscles. There were also thoracic segmental dysfunctions at the T2 and T6 levels.
We ordered a CT scan. Red flags warranting a CT included vomiting while concentrating on homework, increased headache, decreased left upper extremity strength. The CT was negative for pathology or intracranial hemorrhage, fluid collection, mass effect or infarct.
Following examination and review of the CT scan, clinical diagnosis remained concussion. He was experiencing headaches and balance and neurocognitive impairments. We therefore began care.
Therapeutic Intervention
During the first visit, active myofascial release and an instrument-assisted soft-tissue mobilization (IASTM) was applied over the cervical paraspinals, Posterior and Middle Scalene muscles, Upper Trapezius, and Levator Scapulae muscles to address the fascial restrictions that were present. Spinal manipulation involving the Diversified technique was applied to vertebral joint restrictions detected in the thoracic spine initially until the results of the CT scan were reviewed by a radiologist.
Five days following the initial concussion, the patient came for his second office visit. Symptoms included episodes of dizziness and feeling in a “fog.” He had a headache that he verbally rated at a 3/10. Objective examination demonstrated difficulty with balance, especially with his eyes closed. The SCAT-5 assessment was again given for ongoing assessment as well to help monitor deficiencies in cognition and balance. The SCAT-5 revealed the following deficits: orientation 4/5, immediate memory 13/15, concentration 2/5, 7 out of 30 possible balance errors, delayed recall 0/5. At this visit, both cervical and thoracic spinal segmental dysfunctions were identified along with continued myofascial restrictions noted at the initial evaluation. Treatment included myofascial release, IASTM, and an ultrasound-electrical stimulation combination used over the appropriate musculature. Spinal manipulation was performed in the cervical and thoracic spine.
At this time, we felt it was important for the patient to begin a targeted home exercise program (HEP). This was based on his clinical deficiencies in balance and vestibular dysfunction. The targeted program included heel-to-toe walking starting with his eyes looking down at his feet, then looking straight ahead, and finally with eyes closed. He was then to stand with his non-dominant foot behind his other foot in a tandem stance with eyes open and then closed. Vestibular-oculomotor exercises were also used with the patient trying to focus on an object in front of him while trying to bring pens in each hand together to meet together. He was instructed to close 1 eye and focus on an object about 20 feet in front of him and bring his finger out in front of him, right underneath that object. He was then told to “make his finger go into clear focus, then the far away object, and lastly make them both come into focus at the same time.” He was told to perform this routine 3x/day every day.
At his 3rd office visit, now 10 days post-concussion, his symptoms included a mild headache. Mental activity no longer seemed to aggravate the headache. The same treatment was performed during the third appointment: IASTM, myofascial release, ultrasound-electrical stimulation combo, and spinal manipulation in the form of supine Diversified to the cervical spine and prone Diversified to the thoracic spine. His home exercise program was expanded to include more advanced balance and vestibular-oculomotor activities. These included the addition of ballet test, a peripheral vision expansion activity, and infinity walk. During the ballet test, patienta cover one eye with an eye patch. They stand either barefoot or in socks with their eyes directed 20-30 feet in front of them. Holding that target, they slowly raise their left leg in front of them as high and straight as possible, then slowly lower it but without letting the foot touch the ground. They then raise it the same way but to the lateral side, again lowering it without touching the ground. Then, they raise it behind them, slowly returning to the neutral position. This is rpeated with the right leg. After doing that, move the eye patch to the other leg and perform the procedure over. Lastly, they cover both eyes and perform the entire test again. The infinity walk involves walking in a figure-8 pattern while looking at a specific object in the room. As a patient improves, this is progressively refined by adding tasks to improve your skills, such as playing catch while performing the infinity walk.
At his 4th visit, 13 days post-concussion, he had headaches rated only a 2/10 during physical activity that would go away immediately after cessation of that activity. Reading and homework no longer caused headaches or nausea. He no longer had episodes of vertigo nor felt like he was in a fog. Full upper extremity motor strength returned to 5/5 bilaterally. His active cervical ROM had improved but was still slightly reduced. The same treatment was provided as previous visits and his home exercise program remained the same. At this appointment, his first post-injury ImPACT test was administered and compared to his baseline test, which had been administered prior to the start of the football season. This test revealed poor scores in all categories. Since his scores were not close to baseline, he was not allowed to return to full contact for football.
By his 5th office visit (19 days post-injury) he was completely asymptomatic. He no longer had headaches with mental and physical activity and he no longer felt “foggy.” He did not display balance errors with tandem and single-leg stance. Objectively, cervical ROM was restored and non-painful. A second post-injury ImPACT test was administered that demonstrated scores in reaction time and visual memory only slightly below his baseline. No spinal manipulation or soft tissue modalities were performed since he did not display any muscular spasms or segmental dysfunctions warranting chiropractic manipulation or soft-tissue treatment. He was released for full contact game-play. He was instructed to follow-up next week. He was taken through his exercise program before conclusion of that appointment.
At the 6th and final visit (27 days post-injury), he had no symptoms. He was able to participate fully in the previous football game. He was back to attending school full-time without any accommodations. The ImPACT exam was given for the third time and all scores returned to baseline.
It is important to note that school and activity restrictions were employed during the course of care. Initially, we recommended he be held from school for 2 days, which in this case fell over the weekend. He was told to not participate in physical or cognitive activity. That following Monday he was told to return to school for a half day to see if his symptoms were aggravated by cognitive activity and then have his initial office visit immediately after that half day of school. At the initial visit he was informed to continue with half days of school until he could tolerate a full day of school. He was also informed that he could not perform any physical activity until cleared to start the RTP protocol. The school was informed of all recommendations and advised to make academic accommodations for him. He was also taken through 5 graded stages of the return-to-play protocol, with each stage lasting a minimum of 24 hours. Aerobic activity was gradually introduced according to the Consensus Statement on Concussion in Sport – the 5th International Conference on Concussion in Sport, Berlin.6,7 Less restrictions and accommodations were applied as he progressed through each stage. He was also instructed to start participating in memory games at home for ongoing cognitive therapy.
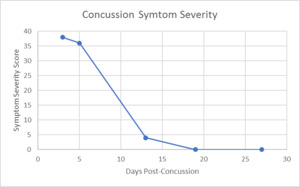
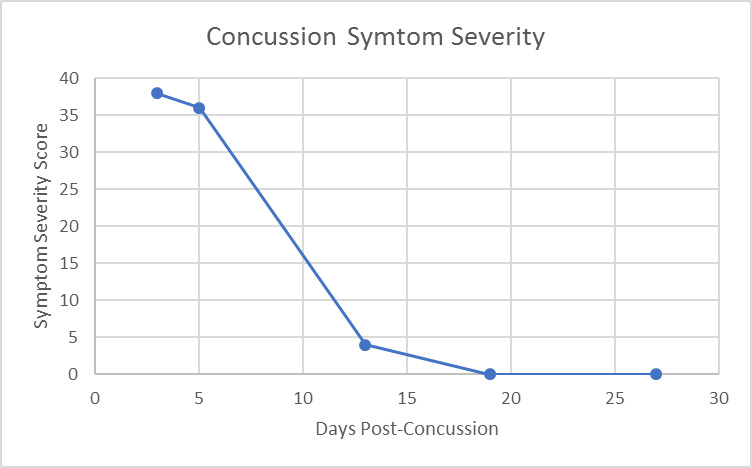
Results of this case study were measured in a variety of ways; however, Figure 1 displays a nice clinical timeline measuring his symptom scores. At his initial office visit, only 3 days post-concussion, he had a symptom score of 38. As time went on with ongoing treatment provided, his symptom score continued to decrease, until finally, 19 days post-concussion the patient’s symptom score was a 0. Furthermore, when taken again at 27 days post-concussion, his symptom score remained a 0/10.
Outcomes
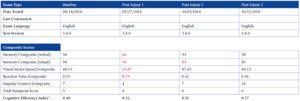
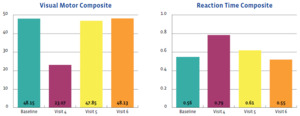
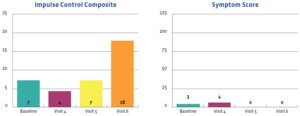
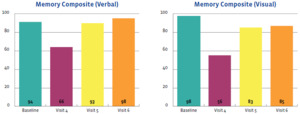
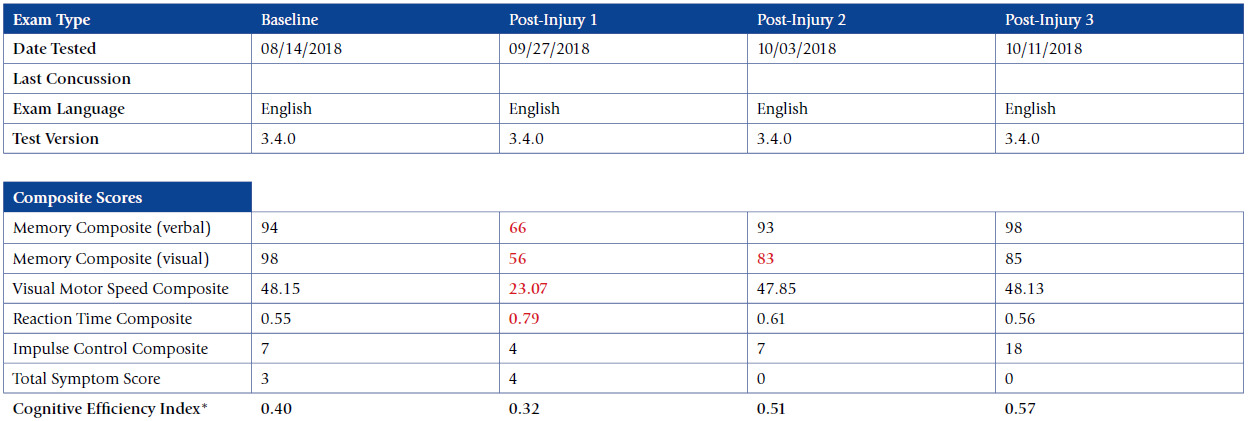
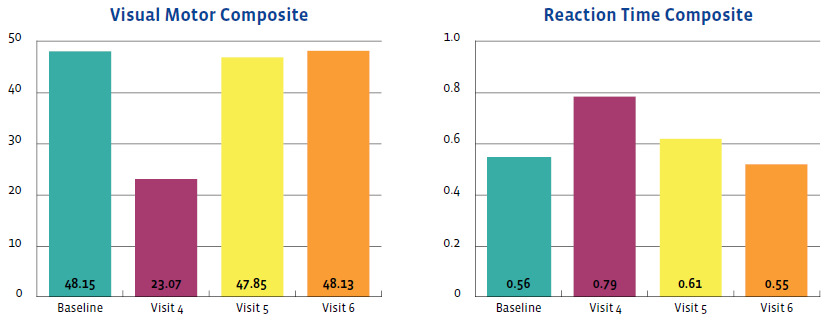
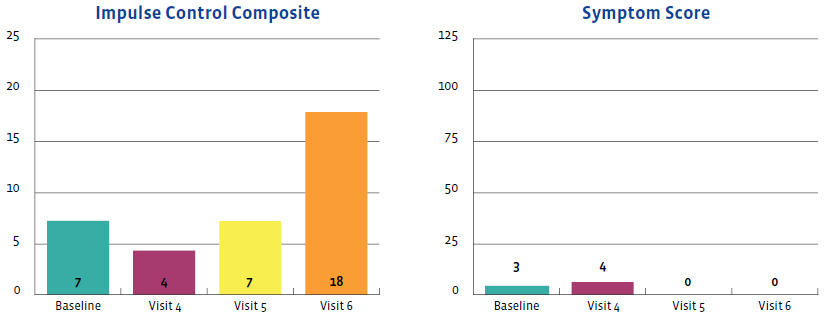
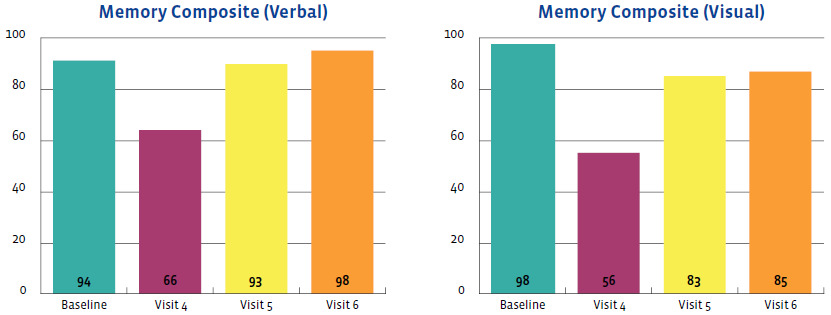
The outcomes of this case study are important to assess and were favorable. They were measured using the symptom severity score, as noted above, as well as with the SCAT-5 scores, the ImPACT scores, and objective examination findings. Figures 2-5 display the results of the ImPACT testing. Note that on Figures 2-5 all his ImPACT scores returned to baseline throughout the course of care.
Objective findings also improved. Initially, his objective findings revealed 4/5 left upper extremity motor strength, reduced cervical ROM, cognitive and balance deficiencies. Upon clearance for full contact game participation, the patient had 5/5 left upper extremity strength, full cervical ROM and no cognitive or balance deficiencies.
During the first week of care, his SCAT-5 scores slightly improved with balance, immediately memory, and concentration. He continued to have headaches, dizziness, and nausea with all activities. His headache was 3 out of 10 for pain level. However, as soon as the patient was able to start taking the ImPACT testing, neurocognitive evaluation turned from doing the SCAT-5 to ImPACT testing
Pertaining to the improvements noted with the ImPACT neurocognitive testing, please refer to Figures 2-5. The patient completed the ImPACT test during the football pre-season to establish a baseline score. He then completed the ImPACT test on the 4th, 5th, and 6th visit with 1 week between each visit. During the 5th visit, the scores were only slightly below baseline, however the player was released to return to full contact as he was symptom free. The patient was then recommended to follow-up one week after starting full contact to test again. As you can see, on the 6th visit, the patient’s scores returned to baseline and he was discharged from care.
DISCUSSION
We feel that arguably the most important step in concussion management is early recognition of symptoms. With early recognition, clinicians and physicians can remove the athlete from play and therefore reduce the risk of second-impact syndrome. One can also consider removal from school or other areas that may further aggravate the symptoms.1 Once removed, clinicians can further evaluate the individual to provide a proper diagnosis and management strategy.1 Additionally, proper diagnosis concerning concussions can be challenging due to variation of symptoms as noted earlier.5 Often, the list of differential diagnoses may be longer than a clinician may like, and therefore more challenging. Differentials may include whiplash syndrome, intracranial hemorrhage, and other TBIs. Due to the red flags displayed here, head CT was justified as it ruled out intracranial hemorrhage and fluid collection within the intracranial structures.
The goal of managing a young athlete with concussion is to hasten recovery by ensuring that the athlete is informed and avoids activities and situations that may slow the recovery process or cause re-aggravation and deterioration. Concussion management should be unique to each individual and take into consideration their subjective and objective findings. In this case, our patient’s symptoms included headache, feeling in a fog, dizziness, nausea, vomiting, and poor balance. He did not have any neck pain nor palpable tenderness within the cervical region initially. There is emerging literature that indicates both active treatment strategies and manual therapy in the early stages for those suffering from SRC, including cervical spine and vestibular rehabilitation for that dysfunction.8–10 The care provided here followed those guidelines. The patient was given an individualized active exercise program and in-clinic treatment was geared at restoring both cervical and vestibular dysfunctions. The cervical dysfunction was addressed with high-velocity low-amplitude (HVLA) manipulation in the cervical and thoracic spine, and therapeutic exercises were prescribed that included various forms of vestibular rehabilitation exercises.
It has become evident that cervical spine manipulation provides functional improvement to a target and adjacent motion segment by improving motion in all planes.11 Improving the motion of the involved spinal segments helps to decrease cervical dysfunction. The patient demonstrated restoration of cervical range of motion during the course of his care, along with resolution of symptomatology. Furthermore, Olson et al published a case study in the Journal of Chiropractic Medicine in which a 14-year-old male hockey player presented with post-concussion syndrome.8 This individual’s treatment also included HVLA manipulation, soft-tissue modalities and therapeutic exercises provided over a 20-day period of care. A neurocognitive computer-based test was also implemented to monitor progression. The patient was being monitored by a medical doctor throughout the entire course of chiropractic care. After 5 treatments, he reported no symptoms and neurocognitive scores had improved to a point where the involved physicians were comfortable enough to clear him for play. These case studies provide initial evidence that chiropractic care may be beneficial to individual’s with sports-related concussion.
The importance of screening for vestibular and oculomotor impairments is cited for those who have sustained a sports-related concussion. Kontos’ literature review evaluates the impairments involving vestibular and oculomotor pathways and offers information about current treatment approaches for the impairments.4 They suggest that strategies should include rehabilitation exercises matched to an individual’s clinical profile. Common vestibular exercises include balance training, gaze stability, and sensory organization training. Possible oculomotor strategies can incorporate visual-attention tasks and near-far-vision focal shifting. This review further supports the home exercise program given in our case because it was a targeted rehabilitation program tailored to the symptoms and impairments screened in the patient. The targeted exercises here included both vestibular and oculomotor strategies that may have helped to expedite recovery.
A second paper provides further evidence of the importance of screening for impairments to aid in clinical decision-making.12 A clinical evaluation of concussion should include gait, balance, and neurocognitive screening tools. These screening tools are often used during objective side-line evaluations and computer-based programs. Assessing these impairments as a single-task or in isolation can be useful; however, this review offers insight on the importance of dual-task screening by combining cognitive and balance tests. In this case, impairments were screened in the football player using single-task assessments such as the SCAT-5 form and ImPACT computer-based test. This review provides recommendations that were beneficial in our case with the combination of gait and cognitive tasks to further identify disturbances caused by concussion.
There are many heterogenous presentations and various clinical profiles of concussion in which a team approach involving multiple health disciplines can provide more effective and collaborative care for an individual.2 Our report provides evidence that a chiropractor can be a coordinating healthcare provider within the many healthcare specialties that an individual may seek care from. Current studies emphasize the importance of targeted and active treatments that are directed at the symptoms and impairments presented by an individual.2 Research is lacking in terms of evidence-based treatments, but multimodal treatments, including cervical spine manual therapy, vestibular rehabilitation, vision therapy, and exertion training, may be beneficial.2,8,9,13 Chiropractic care is a cost-effective approach that provides multimodal care to an individual with concussion.
Limitations
This is a case study describing the treatment and management of a single patient and therefore may not be applicable to every patient with sports-related concussion. Most athletes will recover from sports-related concussion within 21-28 days.1–3 Therefore, we cannot assume the patient improved due to chiropractic care vs. the natural progression of concussion.
Future research, including additional case reports and more rigorous randomized controlled trials, should examine the use of spinal manipulation and targeted active treatments in the conservative management of sport-related concussions.
Conclusion
A 17-year-old male football player sought chiropractic care for treatment and management of concussion-like symptoms. Throughout the course of care, his symptoms and objective findings improved and his neurocognitive computer-based testing scores returned to baseline 27 days post-injury. Given the subjective and objective improvements, he was eventually cleared to return to full contact football.