INTRODUCTION
Low back and neck pain are a significant public health problem affecting increasing numbers of people.1,2 In 2015, low back and neck pain were the 4th leading cause of disability-adjusted life years after ischemic heart disease, cerebrovascular disease, and lower respiratory infection.3 The prevalence of these disabilities costs governments around the world billions of dollars in treatment and workers’ compensation costs each year.1
Mental illness is also a growing public health concern.4 In 2015 the Global Burden of Diseases, Injuries, and Risk Factors Study found that mental disorders were among the highest-ranking causes of nonfatal burden worldwide.5 Anxiety disorders were the 9th leading cause of nonfatal burden as measured by years lived with disability.6 Anxiety is defined as the presence of “fear or nervousness about what might happen”.7 Anxiety is known to impact the quality of life (QoL) of those affected and its effects are numerous from individual performance, familial, social and economic.8–10 Worldwide, recommendations are that governments provide adequate prevention and treatment services for mental health disorders including anxiety.4
While the benefits of chiropractic for people presenting with chronic spinal musculoskeletal complaints are well documented,11,12 the literature describing the chiropractic management of patients presenting with anxiety and related symptoms is more limited, with 2 clinical trials showing conflicting results.13,14 The purpose of this paper is to chronicle the resolution of musculoskeletal discomfort, improvement in mental health and physical functioning in a 38-year-old female receiving Torque Release Technique (TRT) for the assessment and correction of vertebral subluxation.
CASE REPORT
History
A 38-year-old female with a 2-year history of low back discomfort, 6-month history of neck pain and a 3-month history of anxiety and panic attacks presented for chiropractic care. The low back pain was identified as being in the lower thoracic spine on closer examination. She reported this pain to be generally constant for the past 2 years and increased in intensity when experiencing higher levels of stress.
Her neck pain was reported as being persistent for 6-months and rated as 6 out of 10 on a Visual Analogue Scale. The neck pain was particularly noticeable when sitting at a desk or leaning forward. It improved when moving. In addition, she reported a constant sense of tension in the back of her neck. She reported sleep interruption due to the lower thoracic discomfort and neck pain.
Anxiety and panic attacks had been present for 3 months. A general physician diagnosed her with mild anxiety, though did not prescribe medication or make a referral to a psychotherapist or counsellor. The physician referred her for a cardiovascular evaluation, though no pathologies were revealed during her cardiovascular evaluation.
Depression and anxiety were screened for by the chiropractor using the PHQ-4 instrument. The PHQ-4 instrument is a commonly used short-form subjective assessment that accurately measures depression and anxiety. Data from the PHQ-4 has been shown to be reliable and valid in previous studies.15 The self-reported assessment scores revealed a combined 5 out of 12; a combined score range of 3 to 5 is considered to be positive screening for “mild depression and anxiety”. Individually, she scored 3 out of 6 for anxiety and 2 out of 6 for depression. A score of greater than or equal to 3 in either anxiety or depression suggests the person is positive for that domain, here suggesting a positive screening for anxiety.
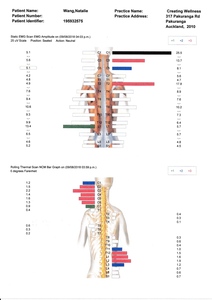
Additionally, she was assessed using the self-reported Health, Wellness and Quality of Life (HWQL) instrument, which measures 5 domains.16,17 The self-reported assessment scores were physical functioning (48%), mental and emotional state (50%), stress evaluation (48%), life enjoyment (43%), overall QoL (71%), and wellness (47%). (Figure 1) An optimal score in each of the HWQL domains is 100%.
Examination
Posture examination, performed by observation, revealed a moderately higher left occiput and shoulder and right hip, and minor forward head carriage of approximately 2cm. Cervical and lumbo-thoracic spine ranges of motion (ROM) was assessed using bubble inclinometry.18,19 Cervical spine ROM revealed flexion of 50°, extension of 60°, left lateral flexion of 45° and right lateral flexion of 40°. Lumbo-thoracic ROM revealed flexion of 60°, extension of 30°, left lateral flexion of 20° and right lateral flexion of 25°. Lumbo-thoracic flexion resulted in patient-perceived pain at 20°. Rotation was not measured in either the cervical or lumbo-thoracic ROM.
An initial chiropractic examination for vertebral subluxation was completed using a battery of commonly-used direct clinical indicators.19–22 The examination revealed a right leg-length inequality, negative right Derifield (further shortening of the right leg in a 90° flexed knee position), right sacral restriction (restriction of the right leg to be extended from the hip compared to the left), and right fast cervical syndrome (balancing of short leg on right head rotation). Static palpation revealed hypertonicity of bilateral Levator Scapulae, right Superior Oblique, bilateral Scalenus Medius, bilateral Quadratus Lumborum and paraspinal muscles at C5-6, T2-3, T6, T10, T12, and L3. Periarticular edema was indicated along the right sacroiliac joint in addition to hypertonicity of the right sacrotuberous ligament. Spinal palpation revealed reduced joint play (end-feel) at C1-2, C5-6, T2-7, T10-12, L3, and the right sacroiliac joint, and inter-segmental motion restriction of C1, C6, T2, T10 and L3 on the left, C2, C6, T3, T6 and T12 on the right. All assessments were performed in the prone position except for cervical spine static palpation and full spine intersegmental motion palpation, which was performed seated.
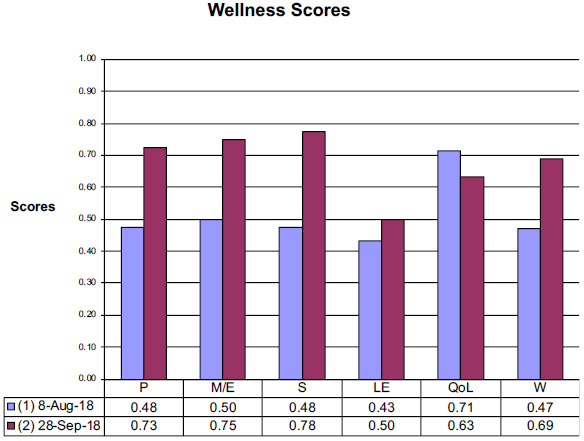
Surface EMG (sEMG) and paraspinal thermography studies were performed using the Insight Millennium. Surface EMG is used within chiropractic practice to measure paraspinal muscle dysfunction, a manifestation of vertebral subluxation, and a neuromuscular response to chiropractic care.23–25 Surface EMG revealed areas of hyperactivity at C1, C3, C5, T2 and L1. Paraspinal thermography is used within chiropractic practice as an indirect measure of autonomic nervous system function (dysautonomia) to assess the impact of vertebral subluxation on the autonomic nervous system.26–28 Thermography revealed varying degrees of autonomic abnormality at C1-C7 and T11-L3. (Figure 2)
Intervention and outcomes
Chiropractic care was initially administered for 12-visits over a period of 7-weeks using TRT protocol. TRT protocol applies functional leg checking and confirmatory spinal pressure testing procedures for the assessment of levels and directions of vertebral subluxation. Vertebral subluxations are primarily identified at locations of dural attachment, notably the occiput, upper and lower cervical spine (C1, C2, C5), sacrum, coccyx and the pelvis. The application of the chiropractic adjustment is via the hand-held Integrator instrument.29,30 No other treatments or modalities were used by the patient during the 7-week period.
During the course of chiropractic care, she reported a resolution in the reported musculoskeletal discomfort. By the 6th visit she reported that her neck pain was only occasionally rated 1 to 2 out of 10 (previously 6 out of 10), and the low back pain was “less obvious” with movement. At the time of the progress examination she reported that she now “rarely noticed back and neck pain,” though the low back pain had been only sporadic in the past.
Improvements were recorded in both depression and anxiety (individual and combined) using the PHQ-4 screening instrument. Depression was rated as 0 out of 6 and anxiety 0.5 out of 6 at this follow-up screening. Improvements were recorded in all domains of the self-reported HWQL assessment, except QoL. The greatest improvements were reported in her ability to manage stress, which improved from 48% to 78%, and in her physical functioning and mental and emotional evaluations, which increased from 48% to 73% and 50% to 75% respectively. For a complete comparison of HWQL results see figure 1.
Posture examination revealed that the left shoulder was still higher, however, revealed that the pelvis and occiput was level and head carriage had normalized. Cervical spine ROM revealed flexion of 50°, extension of 60°, and bilateral lateral flexion of 45° (now even). Lumbo-thoracic ROM revealed flexion of 80° (an increase of 20°), extension of 35° (an increase of 5° and without pain), and bilateral lateral flexion of 25° (now even).
Chiropractic examination revealed a balanced leg length with no Derifield or cervical syndrome apparent. Static palpation revealed hypertonicity of the left scalenus medius and periarticular edema at C1/2 on the left. Restriction in joint play was noted at T4, L5 and the left SI. Inter-segmental motion restriction was indicated at C2 on left lateral flexion and posterior rotation, and T4 and L5 on extension. These findings represent a reduction in direct indicators of vertebral subluxation when compared to the initial examination. The most commonly adjusted levels were C0 and C2. For a complete summary of chiropractic adjustments administered see table 1.
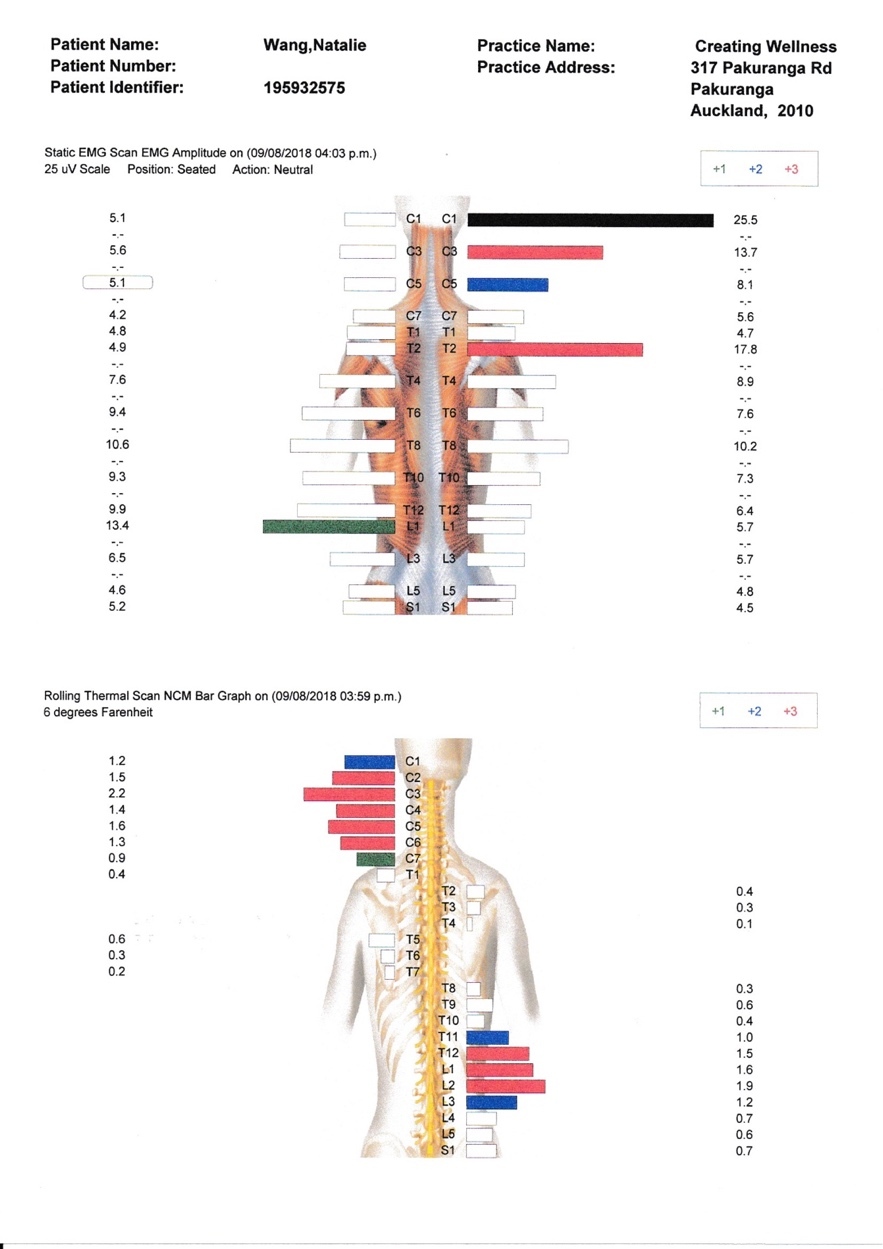
Surface EMG revealed areas of hyperactivity at C3 and hypoactivity at T12 and L1. Thermography revealed varying degrees of autonomic abnormality at C1 and L3-S1. (Figure 3) These results represent an overall improvement in paraspinal neuromuscular function and reduction in dysautonomia.23–28
DISCUSSION
This case chronicles a course of chiropractic care associated with resolution of musculoskeletal discomfort, improvement for mental health and physical functioning in a 38-year-old female receiving TRT for the assessment and correction of vertebral subluxation. Additionally, improvement in the patient’s perceived low back and neck pain, posture, spinal ROM, and reduction in vertebral subluxation were reported.
The most commonly employed treatment methods for anxiety, panic attacks and depression include psychotherapy, psychological approaches and pharmacological interventions.31 As anxiety symptoms are also common in depression, and often times present together in a patient, benzodiazepines and anti-depressant medications are most commonly prescribed.31
Complementary and alternative medicine (CAM) approaches, in which chiropractic care is often included, are also growing in use rates for mental health management.32–35 Approximately 17-20% of people suffering from anxiety have used CAM approaches in an effort to manage their presentation.32,35 The most commonly used CAM approaches include relaxation techniques, meditation, massage, and spiritual healing.35,36 Chiropractic care is rarely indicated as a CAM choice for people with anxiety.35,36 While anxiety is seldom a reason for people choosing chiropractic care, people presenting for chiropractic care may have mental health concerns, including anxiety and depression.37
Limited scientific evidence supports the chiropractic management of people with anxiety. A recent review article describes the neurobiological mechanisms by which the effect of vertebral subluxation on nervous system function could lead to altered mental health.38 A review of the available literature found 2 clinical trials,13,14 1 case series,39 as described below, and 6 case reports40–45 as referred to in table 2.
The 2 clinical trials employed the patient-reported outcome measure Spielberger STAI instrument to assess for effects of anxiety. Yates et al13 found a significant improvement in anxiety scores following a course of chiropractic care. However, Brockman14 found no significant improvement between the chiropractic and control groups. In both studies, an Activator instrument was used to provide chiropractic adjustment to the areas of the spine deemed subluxated. The main difference between these 2 studies is the Yates et al study used subjects with a medical history of hypertension, where the Brockman study used subjects that were healthy.
A case series by Roth et al39 reported on 5 adults receiving upper cervical chiropractic care over a 6-week period. Each patient was assessed with the Generalized Anxiety Disorder – 7 (GAD-7) and Patient Health Questionnaire – 9 (PHQ-9) scales to assess for anxiety and depression. Each participant scored at least a mild positive finding. A significant decrease in anxiety symptoms was reported in all 5 cases. Although a variety of chiropractic techniques were employed in the above cases, all 9 studies (clinical trials, case series and reports) specifically discuss the assessment and correction of vertebral subluxation as the chiropractic intervention.13,14,39–45 One case employed additional non-chiropractic modalities.42
One approach to chiropractic care aims to optimize health and wellbeing through enhancing nervous system function by correction or reduction of vertebral subluxation, typically by manual adjustments.46–49 The assessment and correction or reduction of vertebral subluxation has been reported as being a core objective of chiropractic clinical practice.50 The Australian Spinal Research Foundation have conceptually defined vertebral subluxation as “a diminished state of being, comprising of a state of reduced coherence, altered biomechanical function, altered neurological function and altered adaptability.”51 According to Lantz, ‘common to all concepts of vertebral subluxation are some form of kinesiologic dysfunction and some form of neurologic involvement,’52 while Kent proposes an operational model of vertebral subluxation that includes dysafferentation, dyskinesia, dysponesis, and dysautonomia.53 Haavik and Murphy proposed a neuroplasticity model which suggests that vertebral subluxation cause aberrant proprioceptive afferent input to the central nervous system, which in turn influences sensorimotor integration influencing health outcomes.46
Overall positive results were seen in the patient’s musculoskeletal discomfort, perceived anxiety, mental health and physical functioning. The outcome here is congruent with previously published studies reporting the effects of chiropractic care in similar cases.13,39,41,43–45 There is still limited research investigating the effects of regular chiropractic care on patients with mental health concerns, in particular anxiety and depression. More research is needed to investigate the role chiropractors may play in helping similar patients so as to inform clinical practice and future higher-level research designs.
Limitations
While this case study reports on improvements in this patient, there are several limitations that need to be acknowledged. While the patient had been diagnosed with anxiety by her general physician, she had not been formally diagnosed with anxiety by a psychotherapist. The HWQL instrument has had some psychometric evaluation pertaining to validity, reliability, and responsiveness; however, more psychometric properties could be analyzed.16 The HWQL instrument has been used to assess individual domains of QoL and the results reported in the chiropractic literature.16,17,54–65
Posture assessment was visually observed by the chiropractor pre and post chiropractic care. No formal objective measure was used to assess posture. Thermography and sEMG have been shown to be unfavourable in determining the site of chiropractic intervention.19 The use of thermography and sEMG in the current study was not to determine the site of vertebral subluxation. Thermography and sEMG were used to objectively measure dysautonomia and paraspinal neuromuscular dysfunction that may be a manifestation of vertebral subluxation and changes as a result of chiropractic care.23–28
Due to the inherent limitations of a single case study, being an isolated case not controlled for external factors and natural progression, the findings cannot be generalized or correction of vertebral subluxation implied. To further gauge the effectiveness of care, further higher-level studies are required.
CONCLUSION
A course of chiropractic care, using TRT for the assessment and correction of vertebral subluxation, was associated with resolution of musculoskeletal discomfort, and improvement in anxiety screened with the PHQ-4 instrument, and physical function in a 38-year-old female. Because of the high burden of mental health concerns such as depression and anxiety worldwide, there is a need for examination of effective health care options to support improved mental health. Considerably more research is necessary to adequately bridge the gaps in the fields of chiropractic and mental health.