INTRODUCTION
Trigeminal Neuralgia is classically defined as a sudden and severe, recurrent stabbing pain that primarily affects the distribution of 1 or more of the 3 branches in the Trigeminal Nerve.1 Trigeminal neuralgia is a non-triggerable condition that exhibits unremitting sensory loss and atypical pains.2
Clinically, trigeminal neuralgia has been reported as having a higher occurrence in the female population, with an age-adjusted ratio of 1.74:1.3 The prevalence of trigeminal neuralgia has been reported to be 4-5 per 100,000 in the general adult population, with the incidence rising to 20 per 100,000 after the age of 60.4,5 The peak incidence of trigeminal neuralgia has been recorded in those that are between 60 to 70 years of age.3 Conventional treatment for trigeminal neuralgia involves pharmaceutical management.6,7
Studies have shown that individuals diagnosed with, or experience symptoms of, trigeminal neuralgia also suffer from a diminished quality of life (QoL).8–10 Along with a diminished QoL, individuals with trigeminal neuralgia also experienced a reduction in activities of daily living and an impaired emotional state.8,11 Individuals with trigeminal neuralgia reported increases in anxiety (50%) and depression (37.5%).8
Chiropractic care is commonly used in the management of pain syndromes, though there is limited, lower level clinical evidence describing the chiropractic management of patients with trigeminal neuralgia.12–22 A clinical objective central to chiropractic care is to optimize health and wellbeing through the improvement of nervous system function by removing or reducing nerve interference thought to be caused by vertebral subluxation .23–25 A vertebral subluxation has been recognized as a complex of functional and/or structural changes in the articulations of the spine and pelvis that compromise neural integrity and may influence organ system function and general health.26 Common to all models of vertebral subluxation are both biomechanical and neurological attributes.27–30 Vertebral subluxation correction is achieved through chiropractic adjustments that are a typically manually performed.26,31,32
The purpose of this case report is to chronicle the improvement in symptoms associated with trigeminal neuralgia in a 65-year-old female following a course of chiropractic care using Activator Methods Chiropractic Technique (AMCT).
CASE REPORT
History
A 65-year-old female had symptoms associated with trigeminal neuralgia. Her symptoms had been medically diagnosed 6-years prior. She had been prescribed Tegretol (carbamazepine), an anticonvulsant pharmaceutical used to manage pain associated with trigeminal neuraligia, at a dose of 4.5 tablets (200mg per tablet) per day. She had undergone surgery to treat the symptoms 1 year after the diagnosis. Due to failed response to surgery she sought chiropractic care to help alleviate her symptoms. She reported that while she received chiropractic care she experienced remission of symptoms and decreased Tegretol use, which had reduced from 4.5 tablets per day to 0 to 1 a day, after an approximately 9-month period. She received ongoing chiropractic care for a 3-year period, though ceased chiropractic care when her chiropractor moved away.
The symptoms associated with trigeminal neuralgia returned and the intake of Tegretol had increased back to 4.5 tablets (2 in the morning and 2.5 in the evening). Due to an exacerbation in symptoms, she sought chiropractic care again due to previous positive results. Previous chiropractic care was also AMCT. Her current symptoms were similar to her past history and described as widespread sharp, intermittent left scalp and facial pain that she rated 8- 9 out of 10, on a Visual Analogue Scale, exacerbated by touch, talking and eating. Additionally, she reported experiencing excessive fatigue, changes in mental health (including anxiety, poor concentration, and memory loss), and constipation as a result of the high doses of Tegretol.
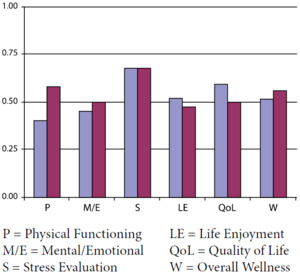
She subjectively rated her physical health as 5 out of 10 and mental health as 6 out of 10 at her initial presentation on a 10-point numeric rating scale where 1 is worst and 10 is best. Additionally, she was assessed using the self-reported Health Wellness and Quality of Life (HWQL) instrument, which measures 5 domains, and generates an overall wellness score.33,34 Scoring is from 0 to 100%, with higher percentages being more favorable. The HWQL instrument has been used and the results reported on extensively in the chiropractic literature.33–42 Her self-reported assessment scores were physical functioning (40%), mental/emotional wellbeing (45%), stress evaluation (68%), life enjoyment (52%), and overall QoL (59%). (Figure 1)
Examination
Cranial nerves V (Trigeminal) and VII (Facial) were found to have positive tests. Cranial nerve V (Trigeminal) testing confirmed widespread severe facial (forehead, maxilla and mandible), scalp pain to light touch on the left, and clenching the jaw. Cranial nerve VII (Facial) testing revealed pain on attempting facial expressions such as smiling and grimacing. These findings are consistent with the symptomatic presentation of the previously diagnosed trigeminal neuralgia. No other cranial nerve or vital sign assessments were positive.
Posture examination, performed by observation, revealed a markedly higher right shoulder and occiput, and forward head carriage. Cervical spine ranges of motion (ROM), using bubble inclinometry,43 revealed flexion of 50°, extension of 40°, left lateral flexion of 20° and right lateral flexion of 30°.
Chiropractic examination was performed using a battery of commonly-used direct indicators of vertebral subluxation, including intersegmental motion palpation, specific soft tissue palpation, joint play/end feel, and leg-length analysis.44 The examination of intersegmental spinal motion and static palpation of the cervical muscles was performed in the seated position; all other examinations were performed with the patient prone. The examination revealed a right leg-length inequality (the right leg appearing shorter than the left in the flexed knee position), negative right Derifield (the right leg appearing shorted when both legs are flexed to 90°), and right sacral restriction. Static palpation revealed hypertonicity of the right Levator Scapula, Superior Oblique and Sub Occipital muscles bilaterally, left Scaleneus Medius, Gluteus Medius on the right, and paraspinal muscles from C1 to C7 bilaterally, T1 to T4 on the right, T8 to T12 on the left and L2 to L5 on the right. Spinal palpation revealed reduced joint play (end-feel) at C1-2, C5-T1, T4-7, T12-L5, and the right sacroiliac joint, and inter-segmental motion restriction of C1 on right lateral flexion, C2, T4, L4 and L5 on the left rotation and extension, C5 on extension, C7 and T6 on right rotation and extension.
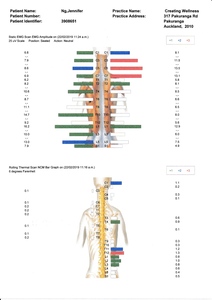
Surface Electromyography (surface EMG) and thermography studies were performed using the Insight Millennium instrument. Surface EMG is used to measure paraspinal muscle dysfunction, a manifestation of vertebral subluxation, and a neuromuscular response to chiropractic care.45–47 Surface EMG revealed areas of hyperactivity from C1 to T1 and S1, with hypoactivity recorded from T8 to L1. Thermography is used as an indirect measure of autonomic nervous system function (dysautonomia) to assess the impact of vertebral subluxation or joint dysfunction on the nervous system.48–50 Thermography revealed varying degrees of autonomic abnormality from C1 to T7 and T9. (Figure 2)
Intervention and outcomes
An initial program of chiropractic care was provided twice weekly over a 6-week period using AMCT protocol. An Activator II instrument was used in the management of the patient. AMCT protocol uses a functional leg-length analysis combined with provocative maneuvers (isolation, pressure and stress tests) to determine involved spinal levels, and a hand-held instrument to deliver a specific, high-velocity, low-amplitude thrust for the correction of vertebral subluxation.51 When cranial adjusting was introduced on the 6th visit, pressure testing was used exclusively to determine site and direction of subluxation, and the activator II instrument used as a force application.
From the 2nd visit during the course of chiropractic care the patient reported awareness of reduction in mouth and jaw pain, and had improved sleep. At the 3rd visit her pain had reduced to 2 out of 10 from 8-9 out of 10, and she was able to eat hard foods comfortably. At the 4th visit her mouth and jaw pain had resolved. On the 7th visit she reported that her face and scalp pain had further reduced, though she was still taking her initial daily dose of Tegretol. At the time of the 10th visit she reported that her facial pain was isolated to a small point on the left side of her forehead, and she had reduced her Tegretol intake by 100mg. She reduced her Tegretol intake by a further 100mg by the 12th visit, and her symptom pattern remained isolated to the small area on her left forehead. For a compete summary of patient subjective reports see table 1.
A progress examination was performed on the 12th visit which included patient self-reported physical and mental health, and HWQL assessment, and Cranial Nerve VII, posture, cervical spine ROM, vertebral subluxation, sEMG and thermography examinations. Her perceived physical health rating improved from 5 to 6 out of 10, mental health from 6 to 7 out of 10. Improvements were recorded in both the physical health and mental/emotional wellbeing domains of the self-reported HWQL assessment. A slight reduction in QoL score from 59% to 50% was thought to be from loss of independence resulting from the effects of the Tegretol leaving her unable to safely drive. For a complete comparison of HWQL results, see figure 1.
Cranial Nerve V (Trigeminal) testing revealed pain to light touch isolated to a 1cm sized area to the left of center of her forehead with no positive findings present over the maxilla or mandible. Cranial Nerve VII (Facial) testing revealed no pain on jaw clenching and attempting to smile and speak. Posture examination revealed generally level shoulders and occiput, with minimal forward head carriage. Cervical spine ROM remained the same, except left lateral flexion of 30° (increase of 10°), making lateral flexion even bilaterally.
Chiropractic examination revealed a right leg-length inequality and negative right Derifield. Static palpation revealed hypertonicity of the right Levator Scapula, left Superior Oblique, right Sub Occipital muscles, left Scaleneus Medius, T5 to T8 on the left, and L1 to L4 on the right. Spinal palpation revealed reduced joint play (end-feel) at C1-2, T4, T6, T11-L2, and inter-segmental motion restriction of C1 on right lateral flexion, C2 and C3 on the left rotation and extension, and T12 to L1 on extension. The most commonly adjusted level was the left occiput, being adjusted 8 times over the 12 visits. For a compete summary of chiropractic care see table 1.
Surface EMG revealed widespread areas of hyperactivity recorded throughout the spine, and elimination of areas of hypoactivity. Thermography revealed far fewer areas of autonomic abnormality, now only at C1, T4, T11 to L3. These results represent a generally more balanced paraspinal neuromuscular function, and an overall reduction in dysautonomia following chiropractic care. (Figure 3) The use of thermography and sEMG in this study was not to determine the site of vertebral subluxation, but was used to objectively measure dysautonomia and paraspinal neuromuscular function that is thought to be a manifestation of vertebral subluxation.46–48,50
Following the initial program of chiropractic care the patient continued regular visits. Over a further 10 visits (7 weeks) the patient experienced a sustained reduction in facial pain, and a further 200mg self-reduction of Tegretol, reducing 100mg on the 15th and 20th visits. Her Tegretol intake now reduced to 500mg from 900mg daily. The patient reported feeling more energy and not needing an afternoon sleep at the 16th visit, and feeling so much more alert on the 18th visit.
DISCUSSION
This case report describes the reduction of symptoms associated with trigeminal neuralgia, both from subjective reports and through CN V and VII testing, in a female receiving chiropractic care. Additionally, the patient reported improvement in physical functioning and mental/emotional wellbeing, posture, cervical ROM, and reduction in vertebral subluxation.
The primary and most common form of treatment for Trigeminal Neuralgia includes taking prophylactic medication to help aid in the prevention of reoccurring attacks.6,7 The most common pharmaceutical used in the treatment of trigeminal neuralgia is Carbamazepine.52,53 The dosage of Carbamazepine is typically slowly escalated throughout treatment to help aid in the management of symptoms.52 While the effects of Carbamazepine have been shown to suppress the paroxysmal pain of trigeminal neuralgia, the benefits elicited in postherpetic and atypical facial neuralgia have been minimal.54 Failure of typical pharmaceutical treatment can lead to the more invasive measure of neurosurgical intervention.7 The typical and most popular neurosurgical intervention used in the majority of trigeminal neuralgia cases would be microvascular decompression (MVD).52,55,56 MVD as a surgical approach decompresses the affected root entry zone of the fifth cranial nerve.56 In turn, it is highly associated with relieving the pain symptoms in trigeminal neuralgia and shows a low morbidity rate.56
There are a number of complementary and alternative medicine (CAM) approaches, which include chiropractic, that have been reported to show success in the treatment and management of trigeminal neuralgia.22,57–59 These include acupuncture and biofeedback.22,57–59 However, in both treatments of acupuncture and biofeedback, mixed outcomes of relief were recorded when addressing the pain management of trigeminal neuralgia.59,60
There is limited scientific evidence supporting the chiropractic management of people with trigeminal neuralgia. A review of the available literature found only lower-level evidence. The 11 case reports found in the review of literature are summarized in table 2.12–22
Reduction or elimination of medication for the management of trigeminal neuralgia was reported in 3 studies, which is consistent with our current report .16,20,21 A variety of chiropractic techniques were employed in the case reports; upper cervical techniques were most often used.12–15,21,22 Nine case reports specifically describe the assessment and correction of vertebral subluxation as the sole intervention.15–18,20,21 The current study is only 1 of 2 to demonstrate a reduction in direct indicators of vertebral subluxation following a course of chiropractic care,14 though 1 other did report changes in spinal biomechanics on radiographic studies.18 Non-chiropractic intervention was additionally used in 2 cases.19,22
While there is limited current research investigating the effects of chiropractic care on trigeminal neuralgia, the outcomes reported in this case are congruent with previously published studies reporting chiropractic care for patients with trigeminal neuralgia.12–22 To our knowledge, this is the first study that demonstrates a positive response to management using AMCT, including formal assessment of mental and emotional wellbeing, in a case of trigeminal neuralgia. More research is needed to investigate the role chiropractic care may play in helping similar patients, to better inform clinical practice and future higher-level research designs.
Limitations
While there are positive improvements reported in the patient’s symptoms, there are several inherent limitations that must be acknowledged. This study is a single case report which cannot be controlled for external factions, no definitive relationship can be concluded between the correction of vertebral subluxation and the improvement of the patient’s symptoms. Spontaneous remission and natural progression cannot be ruled out, and the findings cannot be generalized to the general population.
CONCLUSION
A course of chiropractic care, using AMCT for the assessment and correction of vertebral subluxation, was associated with reduction of symptoms associated with trigeminal neuralgia in a 65-year-old female patient. Pharmaceutical management was reduced while receiving chiropractic care.