INTRODUCTION
A mild traumatic brain injury (MTBI) or concussion is defined as a complex pathophysiologic process affecting the brain, induced by traumatic biomechanical forces secondary to direct or indirect forces to the head.1 Duration of symptoms is highly variable and may last from several minutes to days, weeks, months, or even longer in some cases.1,2 Approximately 1.6 – 3.8 million sports and recreation-related traumatic brain injuries occur in the United States each year.3 Most of these are MTBIs that are not treated in a hospital or emergency department.4 Symptoms of MTBI include functional changes in physical, cognitive, emotional and sleep parameters, as seen in Table 1.
Post-concussion syndrome has been described by the World Health Organization as
"A syndrome that occurs following head trauma (usually sufficiently severe to result in loss of consciousness) and includes a number of disparate symptoms such as headache, dizziness, fatigue, irritability, difficulty in concentration and performing mental tasks, impairment of memory, insomnia, and reduced tolerance to stress, emotional excitement, or alcohol."5
When looking at the prevalence of post-concussion syndrome following an MTBI, a study found that 27.8% of people went on to suffer from post-concussion syndrome.6 Traditionally in chiropractic practice, many of the symptoms of post-concussion syndrome have been helped when correcting function of the craniocervical junction.7–10 This leads to the question, how much of an influence does the craniocervical junction have on post-concussion syndrome? The craniocervical junction is defined as “the junction of the base of the skull and the cervical spine including the occipital bone, surrounding the foramen magnum (occiput), C1 (Atlas), C2 (Axis), and the intervening tendons and ligaments.”11
There is also a striking similarity between post-concussion symptoms and the symptoms of Whiplash-Associated Disorders (WAD). Injury or dysfunction of the cervical spine with a whiplash incident has been shown to cause headaches, dizziness and loss of balance, nausea, visual and auditory disturbances, reduced cognitive function, and many other signs and symptoms considered synonymous with concussion.12 These similarities make it very important to evaluate craniocervical function with post-concussion patients.
It is likely that the forces required to cause an MTBI will also injure the soft tissue of the cervical spine and disrupt proper joint mechanics and alignment, causing vertebral subluxation. The chiropractic vertebral subluxation is described by the World Health Organization as:
“A lesion or dysfunction in a joint or motion segment in which alignment, movement integrity, and/or physiological function are altered, although contact between joint surfaces remains intact. It is essentially a functional entity, which may influence biomechanical and neural integrity.”13
In 1 study involving football players, the range of linear impact accelerations causing concussion injury was between 60-160 G.14 Whiplash injuries can occur at accelerations of 4.5 G.15 Thus it seems probable that the forces required to produce a mild traumatic brain injury will also cause an injury to the soft tissues of the cervical spine.12 In another study, researchers measured aspects of cervical musculoskeletal function in a group of 12 patients with post-concussion headache and in a normal control group. The post-concussion headache group was distinguished from the control group by the presence of painful upper cervical segmental joint dysfunction, less endurance in the neck flexor muscles and a higher incidence of moderately tight neck musculature. The authors concluded:
"As upper cervical joint dysfunction is a feature of cervicogenic causes of headache, the results of this study support the inclusion of a precise physical examination of the cervical region in differential diagnosis of patients suffering persistent headache following concussion."16
Here, treatment of 6 patients allowed us to report the clinical outcome of applying NUCCA chiropractic care for the correction and maintenance of cranio-cervical joint alignment on 6 consecutive patients with post-concussion syndrome.
CASE REPORTS
We treated 6 consecutive volunteer patients who were referred to us from other active patients. There was 1 patient who didn’t complete care due to personal reasons and inability to come in regularly. Two patients had traumatic brain injuries with internal bleeding and were therefore not considered an MTBI leading to post-concussion syndrome. We therefore treated the 6 patients alone. The initial procedure in the study was a history to confirm that each patient had a cranio-cervical trauma and concussion and was suffering from post-concussion symptoms for at least 6 weeks. An examination was then done to determine if there was evidence of an upper cervical subluxation. The examination procedures were consistent with the published standards of care of NUCCA as follows:
-
Postural assessment looking for evidence of head tilt, shoulder un-levelling, pelvic un-levelling.17 (Figure 1a,b)
-
Supine leg check looking for evidence of a short leg.17,18 (Figure 1c)
-
Bilateral weight scales looking for evidence of a significant shift of weight to 1 side. (Figure 1d)
-
Spinal palpation assessing spinal range of motion, spinal fixations, changes in muscle tone, changes in tissue tone.
-
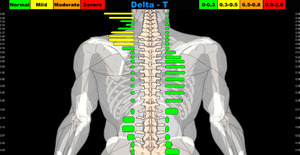
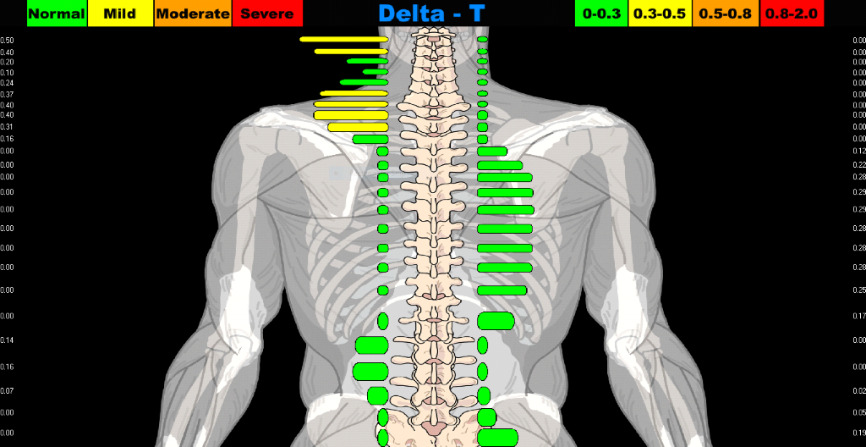
Infra-red para spinal thermography, assessing for significant thermal asymmetries, using the Titronics Tytron C-3000 infra-red thermography instrument.19,20 (Figure 1e,f)
-
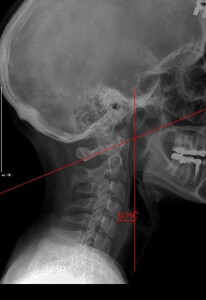
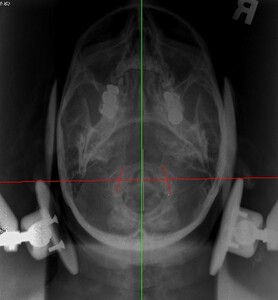
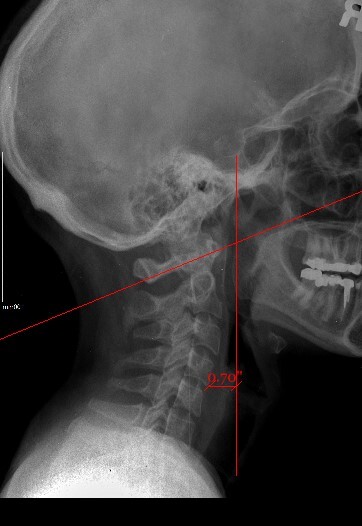
Upper cervical orthogonal based x-rays to measure for significant upper cervical misalignment.17,21,22 (Figure 2 a,b,c)
Figure 1a–1e. NUCCA procedures
These films are used to determine atlas misalignment, develop a correction strategy and confirm an appropriate correction has been made.
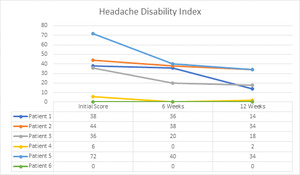
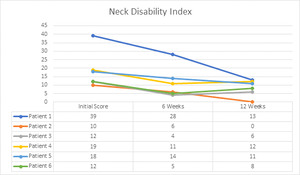
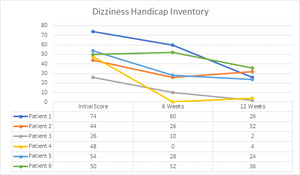
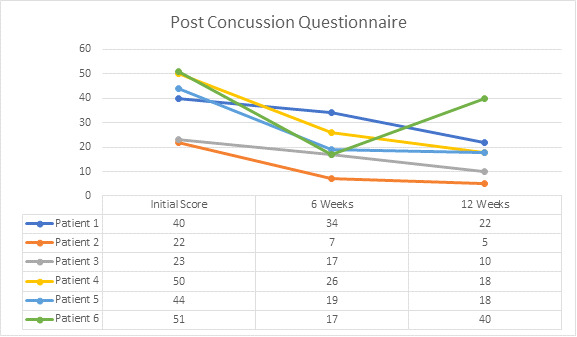
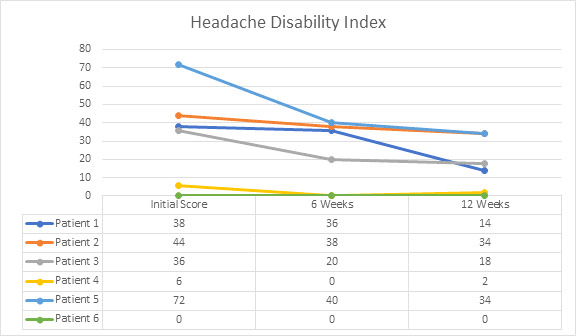
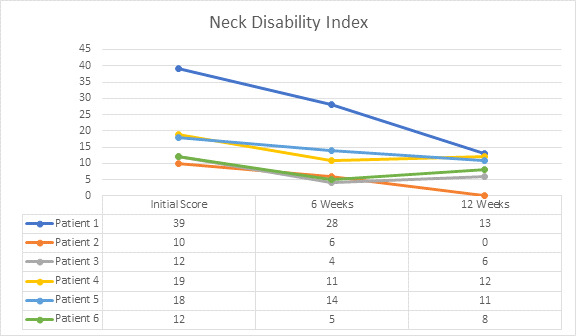
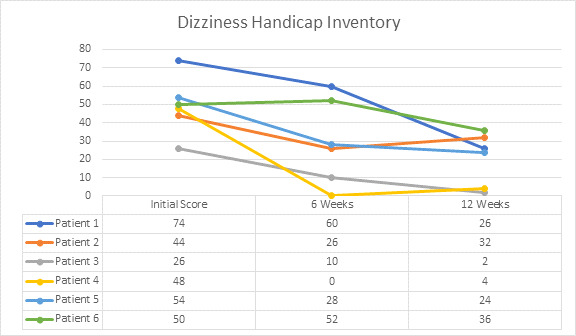
When it was determined that an upper cervical subluxation was present, patients completed the post-concussion intake questionnaires. The questionnaires were as follows: The Rivermead Post Concussion Questionnaire,23 the Neck Disability Index,24 the Headache Disability Index25 and the Dizziness Handicap Inventory.26 For the 4 questionnaires listed above, a smaller number indicates less of a disability. Following this, specific upper cervical chiropractic care began and a NUCCA (National Upper Cervical Chiropractic Association) chiropractic adjustment was performed to restore proper alignment and function to the upper cervical spine, including improved neurological function as measured by posture and thermography changes.27 Following the first adjustment to the Atlas vertebrae, post x-rays were done to confirm that improvement in alignment had occurred. They completed the same forms at week 6 and week 12 to compare the findings.
The patients were monitored over the next 12 weeks to determine if they were holding their alignment or whether another adjustment had to be performed. This was done using the first 5 procedures, as listed above, at each visit.
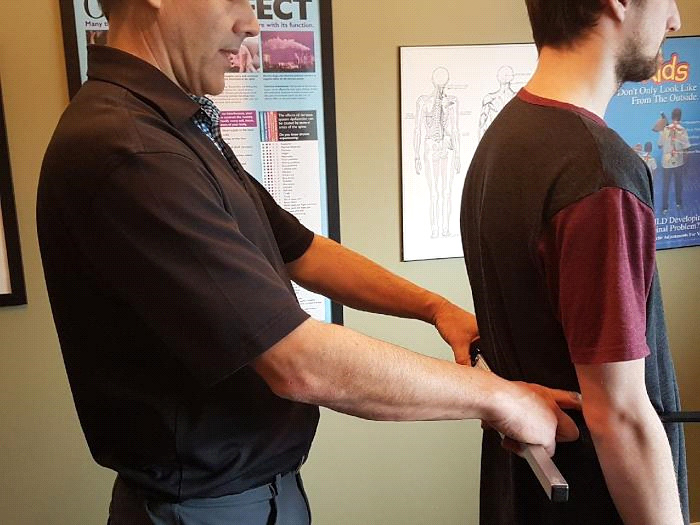
The NUCCA adjustment consists of placing the patient in side posture on the NUCCA adjusting table with the head specifically braced using a mastoid support system, and a specific force was directed into the transverse process of the Atlas. Advanced image-guided care is used to calculate a predetermined specific adjustment vector. “Application of the predetermined controlled force vector for the correction realigns the skull to the atlas and neck to the vertical axis or center of gravity of the spine. (Figure 3) These corrective forces are controlled in depth, direction, velocity, and amplitude, producing an accurate and precise reduction of the ASC. (Atlas subluxation complex)”28 Once the adjustment was accomplished patients rested for a minimum of 10 minutes in the supine position to allow the body to process the adjustment. They were then re-checked using the 5 parameters above to see that a correction had been made. Further details of the method are available elsewhere.28
The frequency of visits ranged from weekly to 3 visits per week for a period of 12 weeks, depending on how well the patient held their alignment.
Six patients (4 female, 2 male) were treated, ranging in age from 39 to 82 years old. The duration of post-concussion symptoms, prior to care at our office, ranged from 6 weeks to 14 months duration. There were no changes in medication and no other therapies were used or started through the duration of the study.
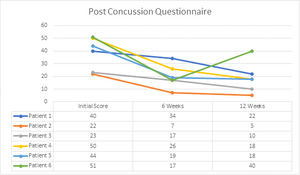
The Rivermead Post-Concussion Questionnaire showed an improvement in scores in all 6 patients, most noticeably after 6 weeks of care. (Figure 4a)
The x ray measurements have been charted to show changes in Atlas laterality, Atlas rotation and degrees of change in angular rotation (measurement in degrees that the cervical spine is off the vertical axis). (Table 3).
Individual Patient Histories and Results
Patient 1: A 59-year-old female suffered a concussion 6 weeks earlier from running into the edge of a door. Her symptoms included constant headaches, photophobia, increased sound sensitivity, anxiety, nausea and tinnitus. Prior history included a severe whiplash 30 years earlier with a history of headaches. She received 14 NUCCA adjustments in 22 visits over the 12 weeks of care. After the 12 weeks she could go without sunglasses inside, could tolerate sound, was much more relaxed, better moods, could think clearer, less headaches, improved blood pressure, less neck pain and better balance.
Patient 2: A 53-year-old male suffered a concussion 12 weeks earlier from falling backward and banging his head on the ice while playing hockey. His symptoms included photophobia, mental fogginess, low energy, poor sleep, poor balance, pressure in head, neck/shoulder pain, and difficulty concentrating. He received 9 NUCCA adjustments in 18 visits over the 12 weeks of care. After the 12 weeks he was able to work full time again, had less neck/shoulder pain, more energy and improved sleep. He had decreased head pressure but it would come and go and he still had poor balance.
Patient 3: A 43-year-old female experienced a concussion from 3 separate accidents over a 5-week period, 10 months prior to coming in. She was initially rear-ended in a car accident, then fell down the stairs one week later and then fell on the back of her head a month later skiing. Her symptoms included constant neck pain, frequent headaches, difficulty concentrating, frequent dizziness, sinus congestion, low energy, eye pain and difficulty focusing, and difficulty exerting while exercising. She received 13 NUCCA adjustments in 22 visits over the 12 weeks of care. After the 12 weeks she reported significantly less neck pain and headaches, less dizziness, clearer sinuses, clearer vision and less eye pain, better concentration and energy, able to write reports at work again and exert with exercising.
Patient 4: An 82-year-old female had a concussion 3 months earlier when she fell and banged her head behind the left ear on a door jamb. Her symptoms included shooting pains in her head, neck pain, dizziness, low energy, frequent nausea, headaches and poor sleep. She received 12 NUCCA adjustments in 18 visits over the 12 weeks of care. After the 12 weeks she reported less neck pain, no dizziness, better sleep and feeling more restful.
Patient 5: A 39-year-old male had a concussion 11 months earlier after being hit in the side of the head during a Muy Thai match (martial arts). His symptoms included constant headaches and neck pain, mental fogginess, sinus pain and head pressure, ear sensitivity, heart rhythm irregularity, inability to exert with exercise, poor sleep, tinnitus. He received 8 NUCCA adjustments in 18 visits over the 12 weeks of care. After the 12 weeks he reported a decrease in headaches, dizziness and neck pain.
Patient 6: A 59-year-old female had a concussion 14 months earlier after a hard fall, in which she was unconscious for 20 minutes. Her symptoms included poor concentration, brain fogginess, fatigue, marked dizziness, blurry vision, sinus congestion, poor sleep and decreased coordination. She received 11 NUCCA adjustments in 23 visits over the 12 weeks of care. After the 12 weeks she reported having more energy, better moods, better sleep, a much clearer mind, clearer sinuses, clearer vision, far less dizziness, and better coordination.
DISCUSSION
In this case series of 6 post-concussion patients there were improvements in many of the measures assessed after the NUCCA intervention. This is suggesting that trauma significant enough to cause post-concussion syndrome can also influence cervical spine function.
The Neck Disability Index showed improvement, with a decrease in numbers, following the 12 weeks of NUCCA chiropractic care. The correlation between restoring cervical spine function and improvements in post-concussion symptoms can be seen in other studies as well and points to the importance of therapy in this area.29
Headaches are a common symptom of post-concussion syndrome.30 In 1 study on 452 patients with traumatic brain injuries, over 41% of patients continued to have headaches at the 3,6 and 9 month intervals following the trauma.30 In another study on 212 patients with mild traumatic brain injury there was a headache rate of over 58% at the 3,6 and 9 month interval following trauma.31 The correlation between headaches and the upper cervical spine has been found in many studies.32–35 This correlation suggests that a proportion of post-concussion headaches could relate to upper cervical spine dysfunction.
Dizziness is another common post-concussion symptom. Studies have reported that 43-81% of patients with sports related concussions develop dizziness.36,37 Restoring cervical spine function with manual therapy and/or chiropractic adjustments can significantly help with dizziness.7,38,39 All 6 patients in this study were experiencing dizziness to some degree and the improvements were substantial following NUCCA chiropractic care.
One study found that cervicogenic vertigo involves both monosynaptic and polysynaptic reflex pathways from the upper cervical spine afferents (associated with a rich innervation from joint and muscle proprioceptors in the cervical spine) to the brainstem structures associated with balance.12 Another study reports:
"In cervicogenic dizziness, pathology in the cervical spine creates abnormal muscle activity in the deep layers of the upper cervical spine, responsible for providing proprioceptive input to the CNS. Dizziness is thought to occur due to the mismatch between aberrant cervical proprioceptive information in relation to vestibular and visual inputs. Because this cervical afferent information also participates in reflex activity for postural control and eye movements, imbalance and impaired eye movements may occur in addition to dizziness. Management of cervicogenic dizziness is directed toward therapies that treat the underlying cervical spine injury to normalize proprioceptive input with visual and vestibular information; along with treatment of any additional balance or oculomotor impairment through targeted exercises."40
Pertaining to the radiological measurements of the upper cervical spine, NUCCA chiropractic theorizes that reducing the misalignment factors in laterality, rotation and angular rotation of the upper cervical spine will remove irritation from the nerve system and improve function. One of the theories on this is the Dentate Ligament-Cord Distortion Hypothesis:
“The Dentate Ligament-Cord Distortion Hypothesis utilizes the unique anatomy of the cervical spine to provide a model which explains how a misalignment of C-1 or C-2 can produce neurological insult directly via mechanical irritation of the spinal cord, and indirectly via vascular compromise of the spinal cord. This hypothesis states that misalignments of the upper cervical vertebrae, because of their unique attachment to the spinal cord by means of the dentate ligaments, can directly stress and deform the spinal cord. Subsequently, this stress on the cord, in addition to direct mechanical irritation, may produce venous occlusion with stasis of blood and resulting anoxia in particular areas of the upper cervical cord.”41,42
Stress on the spinal cord, as stated above, may influence the spinocerebellar tracts of the cord, which would cause postural imbalance through the skeletal structure presenting as shoulder and pelvic unlevelling and a contracted or short leg upon doing a supine leg length test.41,42
Another theory that could explain the influence of upper cervical dysfunction is the dysafferentation model. Seaman formulated a neurological mechanism that implies joint complex dysfunction creates symptoms through joint mechanical receptor dysafferentation.43 Upper cervical misalignment correction may have the greatest potential in modulating afferent input into the central nervous system via this mechanism, which is measured as a decrease in symptoms.43
Limitations
Here, 1 doctor treated 6 patients. Clearly, a larger, multi-doctor study should be a future suggestion. There could be systematic bias related to the measuring of the x-rays. However, studies looking into inter and intra-examiner reliability with orthogonal based x-ray systems have been found to be sufficient, but not conclusive .17,21,22 There is also the natural recovery time of post-concussion patients. There is no clear answer on recovery time with post-concussion although there have been some predictors that correlate to delayed recovery.
“The most consistent predictor of slower recovery from concussion is the severity of a person’s acute and subacute symptoms. The development of subacute problems with headaches or depression is likely a risk factor for persistent symptoms lasting greater than a month. Those with a preinjury history of mental health problems appear to be at greater risk for having persistent symptoms.”44
These predictors were not taken into consideration here but should be considered in future studies with larger sample sizes.
CONCLUSION
Although this was a small case series involving 6 patients, it highlights the importance of upper cervical spine function in relation to post-concussion syndrome for these patients. Many of the symptoms of post-concussion syndrome may have its origins in the cervical spine and evaluating the cervical spine for evidence of an Atlas subluxation following concussion should be considered. Further studies such as randomized clinical trials, to establish upper cervical involvement in post-concussion syndrome are recommended.
ACKNOWLEDGEMENT
The author would like to thank Dr. John Hart for his help with the analysis of the data.