INTRODUCTION
Poor posture in pediatrics is common.1–3 In a study of 562 childrens’ aged 7-12 postures assessed via photogrammetry, only 18% had a balanced posture type.2 In 236 children aged 12-13 years, the occurrence of ‘faulty posture’ was found to be over 50%.3 Lee et al.1 determined that the incidence of cervical hypolordosis was 60% in a group of 181 children.
Back pain is surprisingly common in children. Between one-third to 50% of children may report back/neck pains4 and estimates of children suffering from recurring back pains are as high as 74%.5 Since childhood back pain often leads to adulthood back pain6–8 and back pain is the leading cause of years lived with disability,9 the reduction of childhood back pain is critical for the health of society.
This case presents the alleviation of chronic spine pain, nocturnal enuresis, abdominal pains and sinusitis in a 7 year-old boy who received CBP spine and posture rehabilitation methods to increase cervical hypolordosis, decrease lumbar hyperlordosis, and reduce a mild pseudo-scoliosis (lateral thoracic translation posture).
CASE REPORT
A 7-year-old male was brought in for assessment by his parents. He was experiencing chronic lower cervical-upper thoracic pain, lower back pain, nocturnal enuresis, abdominal pains, and sinusitis and had complained of sore knees since the age of 2.
The child wet his bed nightly, which had been occurring for the last year. His BMI was high. He had been screened for diabetes mellitus ,which was negative, and urine samples were also unremarkable according to the patient’s medical doctor. The only previous treatment was for the nocturnal enuresis and consisted of instructions to not drink past 6pm and urinate just prior to bedtime.
The patient was 117cm in height and weighed 41 kg. Visual observation indicated he had obvious poor, slouchy posture including forward head posture and forward rounded shoulders. He had recently received 6 months of therapy from an occupational therapist for back pain and poor posture without resolution of ailments.
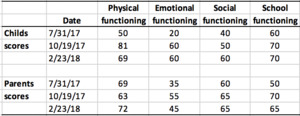
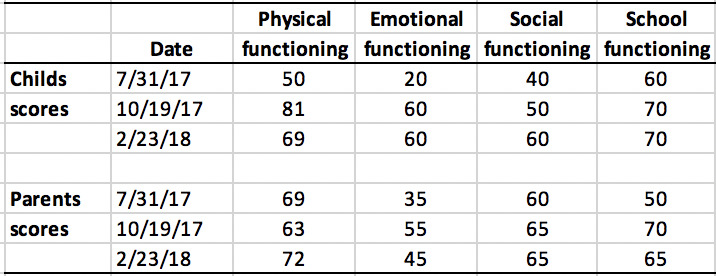
The patient and parents completed the Pediatric Quality of Life Inventory version 4.0 generic core scales (PQLI)10 (Table 1). This is a reliable measure of the child’s health-related quality of life as rated by the parent as well as the child.10
Radiographic assessment was conducted and the images were digitized and analyzed using PostureRay® (Posture Co. Inc., Trinity, FL). This program uses the Harrison posterior tangent method to assess sagittal spine alignment11–14 and the modified Risser-Ferguson method to measure anteroposterior alignment.14 These methods are repeatable and reliable, as is standing posture.11–15
Radiographic assessment indicated the child had forward head translation (11.7mm) and a ‘military’ neck (C2-C7 ARA=0.9°) (Figure 1), lumbar hyperlordosis (L1-L5 ARA=54°) (Figure 2), and a right lateral thoracic translation posture (6.6mm), aka ‘pseudo-scoliosis16 (Figure 3).’
Figure 3. Anteroposterior lumbar radiographs. Left: Pre shows a pseudo-scoliosis/right lateral thoracic translation of 6.6mm. Right: Post shows reduction to 0mm. Note: Red line indicates patient; green line indicates vertical (CBP Seminars, Inc.).
The child was treated with CBP technique rehabilitation protocols to improve posture.17–20 CBP incorporates ‘mirror image®’ exercises, manual adjusting, and traction methods to reverse the spine and posture towards normality. It has been studied in the adult population.21–26 Typical adult programs include treatments at a frequency of 3 times per week for 12 weeks or 4 times a week for 9 weeks before re-assessment.18–20
The manual treatments included paraspinal muscle stimulation with a hand-held instrument (Neuromechanical Innovations, Chandler, AZ, USA) as the child lay on a treatment table. Corrective exercises included prone neck extensions held for 4-seconds, repeated for 8-minutes with 10-second rest breaks in between repetitions.
Spinal traction (Figure 4) focused on increasing the cervical lordotic alignment and reducing the hyperlordosis in the lumbar spine on a Denneroll traction table (Denneroll Spinal Orthotics, Wheeler Heights, NSW, Australia). Traction was started at 3-minutes and increased 2-minutes per session until 12-minutes was reached, thereafter, it remained 12-minutes each session. The patient was treated three times a week for 7 weeks before re-assessment.
Results
Upon re-assessment, the patient and parents reported that all previous complaints had been resolved. The PQLI scores improved in virtually all categories as scored by the parents and child. Radiographic assessment revealed the patient had a gross improvement in posture, reducing the forward head translation (6mm vs. 11.7mm), increasing the cervical lordosis to near normal27,28 (-21.1° vs. +0.9°), reducing the lumbar hyperlordosis (-46.1° vs. -54°) and reducing the right lateral thoracic translation pseudo-scoliosis posture to vertical (0.2mm vs. 6.6mm). The patient continued on a 2x per month basis and remains well. At the 4-month follow-up, the patient and parents scored improvements in all categories on the PQLI (Table 1).
DISCUSSION
This case demonstrates the improvement in cervical lordosis, reduction in lumbar hyperlordosis, and reduction of pseudo-scoliosis in a 7-year old. The improvement in posture resulted in the resolution of multiple spinal pain and health issues and these results were maintained at the 4-month follow-up.
The documentation of correction in pediatric postural deformities with simultaneous spine and health improvements is sparse. Oakley and Harrison performed a review of the correction of pediatric cervical lordosis and found that it is possible when implementing methods that directly hyperextend the neck, as in extension-traction methods as used in CBP technique.27 A case by Basteki et al.29 reported a 20° improvement in cervical lordosis in a 5-year old, which reduced symptoms related to ADHD after 35 treatments over 8-weeks. The improvement in cervical lordosis in this case was 20° after 21 treatments over a 7-weeks period; almost a degree change per treatment, more than the average of 10-18° lordosis improvements demonstrated in several trials on CBP methods treating adults with various extension-traction methods over 30-38 treatments.21–23,30,31 This is likely because the younger pediatric spine is less stiff as well as a smaller spine being weaker and more amenable to change from external forces.
Other postural improvements in this case was an 8° reduction in lumbar hyperlordotic curve. There was only 1 other case in the literature where CBP methods reduced lumbar curve (by 6°), and this was in a 33-year old male.32 This case also showed a complete correction of a mild peudoscoliosis (lateral thoracic translation posture); although this amount of change was consistent with the results in the trial by Harrison et al.33 who found an average 8mm improvement in lateral displacement; it occurred with no traction, as opposed to an average of 36 treatments over 11.5 weeks in the trial. Again, greater improvement in a child may be due to a pediatrics more subtle spine and the fact that the initial shift was only mild (7mm).
Why do children develop poor posture? This question remains to be clarified; however, the use of daily school backpacks may contribute. This is because excessive backpack load carrying causes back pain and spinal deformities in children.34–36 This trend has been termed ‘backpack syndrome’.37 Further, the use of tablet devices may result in considerable postural strain.38,39 Much research into the etiology of the development of poor posture remains.
Limitations pertaining to this case includes that it is only a single case, and that there was only a 4-month follow-up. Another limitation is that although the PQLI was used, no formal documentation was used to quantify the symptom specific improvements that were reported to occur during the treatment of the child. A take home message as seen in this case is that pediatric patients seem to correct faster than adults and with less treatments in the application of CBP methods. Research into the non-surgical spinal rehabilitation of the pediatric patient is lacking and sorely needed.
CONCLUSION
This case demonstrates that the CBP multimodal approach to posture correction achieved postural improvements in multiple areas in this pediatric patient and resulted in dramatic improvements in quality of life and total alleviation of pains. This case illustrates how postural changes in a young patient are possible, and compared to the many clinical trials on adults, happen quicker and have important health impacts. Further research into the non-surgical spinal rehabilitation of the pediatric patient remains to be done and is highly encouraged, particularly as spinal pain in children often translates into spinal pain in adulthood.
Conflict of Interest
PAO is paid by CBP NonProfit Inc., for writing the manuscript; DEH teaches chiropractic rehabilitation methods and sells products for patient care as used in this manuscript.