INTRODUCTION
Carpal Tunnel Syndrome (CTS) is a clinical condition that appears to be increasingly common over the past few decades of today’s technological society.1 The carpal tunnel is a primary source for potential compromise of the median nerve.2,3
Additional areas of median nerve compression include more proximal areas such as the peripheral nerve (at the pronator teres or brachial plexus) and nerve root (at the intervertebral foramen). Such proximal spinal lesions can be present concurrently or even imitate the symptoms of CTS.4 Proximal spinal conditions may exacerbate the CTS or preclude the efficacy of treatment when treatment targets only the carpal tunnel.5,6 Differentiating the distal from the proximal lesions has often been by means of the concurrent presence of neck pain in cervical conditions or a high frequency of nocturnal paresthesia and hand pain in CTS.4 Differential diagnosis of the inciting factor by the clinical presence of hand weakness as a sole-criteria is reported as unreliable. Current accuracy of diagnosis is improved when weakness of abductor pollicis brevis is measured by electrodiagnosis and is coordinated with clinical findings of median nerve distribution hand paresthesia, without neck pain.4,7–10 The Carpal Tunnel Symptom Questionnaire (CTSQ) is commonly used as an additional aid for diagnosis and outcome as it measures the symptoms and functional status, including pain, paresthesia, numbness, weakness, nocturnal symptoms and overall functional status.11 This has been recommended for a primary outcome measure over measures of neuromuscular disability,11 as it measures a different outcome than the NCV studies. Treatment of a spinal component to the CTS may optimize outcomes5 especially for central nociceptive mechanisms that may exacerbate the symptoms associated with CTS.12
Although the Chiropractic Job Analysis reports that manipulation of the extremities is the second most frequent manipulative procedure performed by chiropractors (76% of chiropractors),13 there is little in the area of randomized controlled studies (RCT) for manipulation of non-spinal conditions, or the benefits of a combination of spinal and extremity manipulation14,15 The limited research has recommended post-surgical mobilization16 as being more beneficial than splinting, and spinal and upper extremity treatment was shown to be as beneficial as ibuprofen administration.17 One study for hand and wrist disorders (including CTS), has demonstrated improvement in functional status and pain with manipulation of both the cervical spine and the wrist.18 But there remains a need for further study investigation of the combination of spine and wrist manipulation.
Management of CTS reveals several conservative and invasive CTS treatments are available. In addition to spinal manipulation and extremity wrist manipulation, treatment may include administration of a wrist brace or support, physiotherapy, exercise therapy and surgical intervention. The published studies of most of these treatments are scarce and deficient. Common clinician management of CTS can involve any of these. The literature provides the clinician little direction toward the most effective conservative treatment.19
This gap in the literature for the effectiveness of any particular treatment contradicts current reports of practice, is not based on rigorous clinical trials, and demonstrates the need for clinical evidence of outcomes.14 This case series of patients from a private chiropractic practice is conducted to describe the clinical outcomes of conservative multimodal therapy for CTS, especially with the combination of cervical and wrist manipulation, and to promote further investigation into the modes of conservative care described.
CASE REPORT
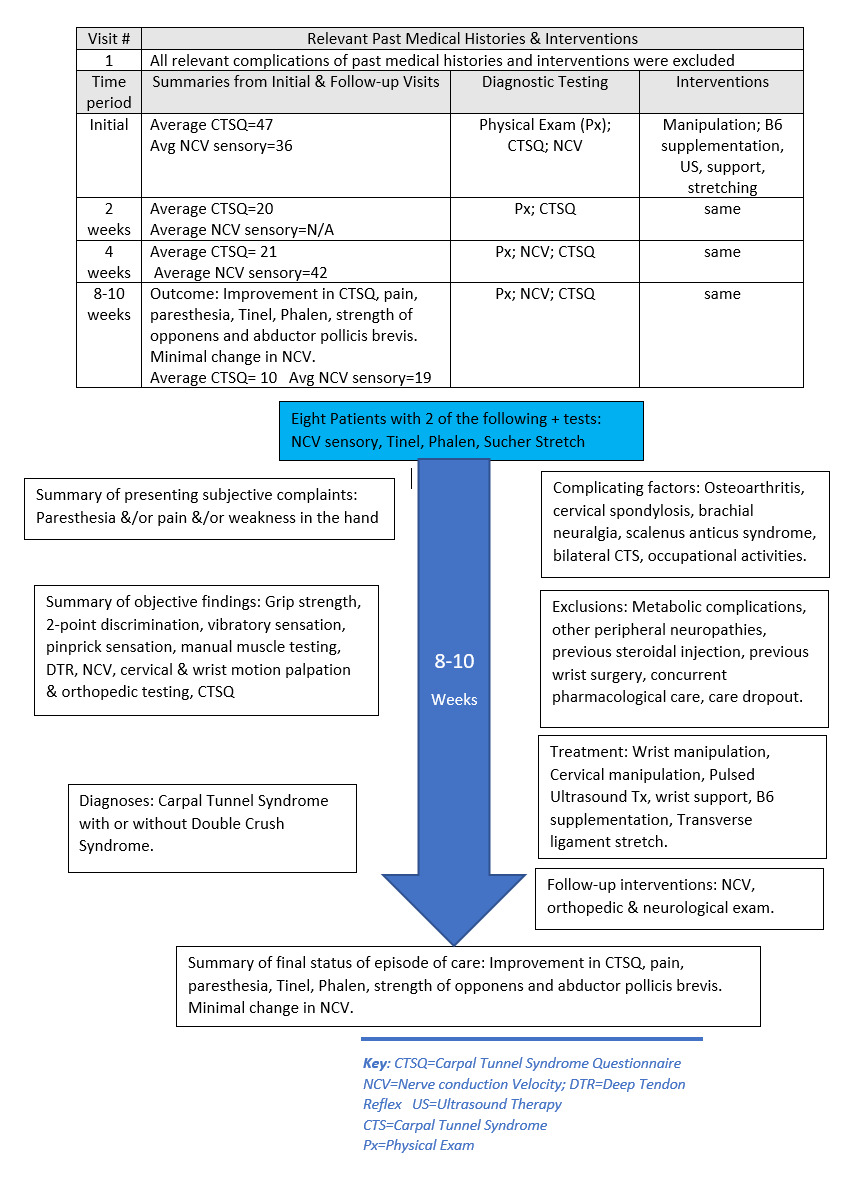
Patient Information: Nineteen patients diagnosed with carpal tunnel syndrome were prospectively assessed in a private chiropractic clinic. Recruitment was a passive process in which there was no solicitation. Patients all had complaints of numbness, tingling and/or pain in the thenar area, thumb and first 2 digits of the hand. Conditions were from variable causes and all were chronic. Data was collected as part of the usual diagnostic workup and follow up. After exclusion and inclusion criteria were applied, 8 patients were included and 13 involved carpal tunnels were included, due to bilateral involvement in five patients. Demographics included 1 male, 7 females and ages from 36 to 78. Occupations included retired secretary, machinist/manufacture laborer, nurse, maintenance worker, home health aide and other noncontributory jobs. (Figure 1)
Patients were re-examined every 2-4 weeks for up to a 9-week period. Initial examinations included motor/sensory assessment and motion/static palpation of the wrist and spine. Motor strength targeted the abductor pollicis brevis and the opponens muscles. Dynamometer grip testing was performed (Baseline hydraulic analogue hand dynamometer) with 3 trials being conducted on each side (arm by the patient’s side, elbow at 90°, wrist at ~15° radial deviation). Sensory evaluation was performed by means of 2 point discrimination testing (1.5cm distance between the 2 sharp points),10 vibratory sensation, (128Hz tuning fork) and sensation to pinprick (Whartenburg pinwheel). All deep tendon reflexes of the upper and lower extremities were evaluated for any proximal loss of nerve function. Full cervical spine examination was performed including all ranges of motion, with standard cervical orthopedic tests to assess cervical joint integrity, radiculitis or brachial neuralgia. Patients who met the criteria underwent NCV motor & sensory studies (Oxford Instruments Teca/Synergy, model #03c015C/Oxfordshire, UK).
Objective outcome measures included Phalen’s maneuver, Tinel’s sign, Sucher’s test (opponens stretch) tests, assessment of grip strength, and manual muscle testing of the abductor pollicis brevis (APB) and the opponens muscles. Subjective outcome measures consisted of the Carpal Tunnel Functional Outcome Score Questionnaire (CTSQ)11,20 Numerical Ratings of pain21,22 and paresthesia. Those that had initial pain rated as 0 were noted to be in uninvolved sides or had insufficient primary criteria findings and were excluded in the study.
Clinical Findings: Diagnostic criteria for carpal tunnel syndrome was derived from the literature23 and clinical experience. Primary criteria required 2 of the following 4 criteria:
-
Positive Nerve Conduction Velocity (NCV) Sensory Study
-
Positive Tinel
-
Positive Phalen
-
Positive Sucher Stretch24,25
Eight patients met the minimal diagnostic criteria of carpal tunnel syndrome. Seventy five percent of the patients had a positive Phalen. All patients had a positive Tinel on at least 1 side. All patients had positive NCV sensory findings at the carpal tunnel on at least 1 wrist. Seven of 13 wrists (54%) examined also had loss of motor function as demonstrated by NCV. Forty percent of the wrists tested had loss of strength in either the APB or opponens pollicis via manual muscle testing. Two-point discrimination, vibratory sensation and grip strength were inconsistently reported. Grip strength demonstrated a weakness in 50% of patients with a loss ranging from 0 to 62%. The initial presentation severity of the condition, as measured by CTSQ, ranged from of 120 to 34 prior to therapeutic intervention. (Table 1)
Therapeutic Intervention: Wrist manipulation was performed using an instrument-assisted manipulation of the lunate bone in the anterior to posterior direction using an ActivatorIITM device, with concurrent performance of the “Opponens Roll” maneuver for “myofascial release” of the transverse carpal ligament (as described by Sucher).25,26 Distraction therapy to cervical spine was utilized in initial stages of care when there was moderate degree of disc degeneration. Manual Diversified high-velocity low-amplitude cervical manipulation was used in all patients either initially or within 2 weeks of care. This was most commonly performed at C5-6-7 levels in the direction of restrictions as determined by motion palpation. Pulsed ultrasound (Richmar, analogue) was applied for 4 minutes to the anterior aspect of the carpal tunnel and the transverse carpal ligament attachments at 1 W/cm2 and 100pps. Patients involved with this project were provided with an M-braceTM (M Brace Radi-ul Carpression Angle™-WristPainCom, Inc*)* and instructed to wear it daily, during daytime activities. The M-BraceTM is intended to approximate the distal radius and ulnar, and subsequently the scaphoid and hamate, by means of sustained medial to lateral and lateral to medial pressure to decrease the tension in the transverse carpal ligament and increase the cross-sectional area of the carpal tunnel.27 Vitamin B6 supplementation was recommended at 50 mg 3x/day for 2 weeks then 50mg once a day thereafter, to reduce the symptoms of neuritis. In office manipulative and ultrasound treatment was thrice weekly (3x/week) for 6-12 treatments.
Outcomes: The results in this study showed a positive improvement in all CTSQ scores with the conservative multimodal care and the combined use of cervical and wrist manipulation. Improvements ranged from a high of 120 (mean=52) upon initial presentation to a low of 7 at end of treatment (mean=14.5, @10wks). Average improvement= 72.5%. (Figure 2)
Wrist pain was not present in 5 out of the 13 cases. One patient rated initial wrist pain as high as 9.5/10 (mean=6). Final pain scores ranged from 0 to 3 (mean=0.4). Paresthesia’s were uniformly present at the initiation of care and were rated as high as 10/10 (mean=7) and as low as 4/10 (mean=2.25). The presence of paresthesia decreased an average of (56%). (Table 2)
Average gain in grip strength was 7.3%. Patients presenting with paresthesia consistently reported involvement of the 2nd and 3rd digits and frequently reported involvement of 1-4th digits with fewer presenting with paresthesia’s in the 5th digit. Each patient had a variable degree of initial pain, but all showed consistent diminishment in intensity. Tinel’s was a more sensitive examination measure than Phalen test as it correlated with CTSQ and was more sensitive to Patient Oriented Evidence that Matters (POEM). Tinel sign revealed that there was a good response to care in 80% of the patients over 10 weeks. Phalen’s demonstrated a good response to care in 44% of the patients over 10 weeks. When motor deficiencies were found in the abductor pollicis brevis &/or opponens pollicis there was a unanimous post-treatment improved strength. Positive examination markers and functional outcome measures did not correlate with change in the neurodiagnostic tests. (Figure 3)
This patient population had a low incidence of uncomplicated single crush CTS. Complicating factors found in this case series that would have contributed to a double crush syndrome, or distal nerve sensitization, included cervical spondylosis, degenerative joint disease, brachial neuralgia, scalenus anticus syndrome, bilateral carpal tunnel, and ongoing work-related ergonomic aggravation. Cervical degenerative joint disease was the most common complicating factor (5 patient files), with 1 case of osteoarthritis in the hand. Fifty percent (50%) of the patients included in the study had bilateral positive findings. When this was present, each hand was treated separately for data accumulation.
DISCUSSION
This case series from a private office population of CTS patients is clearly a small sample of the overall CTS population under care in the United States. Response to care is observed via many outcome measures. This report used symptoms, objective exam findings, neurodiagnostic testing and the Carpal Tunnel Syndrome Questionnaire (CTSQ) for diagnosis and outcome measure.
The symptomatic and physical exam changes were responsive to the patient outcome but did not correlate with NCV changes in this study. This was similar to previous studies done by Lazaro.28 Although NCV is appropriate for diagnosis, it is not as sensitive for an outcome measure. The CTSQ was sensitive to the patient-oriented evidence that matter (POEM) in this case series. It was responsive to measuring the outcomes and indicated a positive response to the multimodal treatment, including the concurrent treatment of both cervical and wrist manipulation.
The high frequency of bilateral presentation in this study may be attributed to a high prevalence of central neurological phenomenon involved in carpal tunnel syndrome. Central neurological pathologies or physiological inhibition may cause the bilateral distribution. This would predispose the patient to distal Wallerian degeneration, which can affect the patient bilaterally or unilaterally. One patient in this group had neurological compromise in 3 areas along the neurological pathway. The distal neurological effect of these multiple lesions has been demonstrated to be cumulative by radiological, clinical and electro-neurological exam. It has been observed that the presence of a more proximal compressive or physiological lesion would render the more distal nerve vulnerable to compression by disturbances in axon flow.30 This would diminish the usual distal treatment outcomes.29–31
Outcome measures: Both the literature and clinical practice reveals delineation of the diagnosis and outcomes of CTS has been based on many different criteria. The gold standard for diagnosis has commonly been nerve conduction velocity motor and sensory studies. Initial diagnosis has been shown to correlate nerve testing with the self-reported measures for CTS.32 Numerous published studies have utilized Phalen’s and Tinel’s for initial diagnosis. Many studies used subjective functional outcome measures to assess the changes in the patients’ activities of daily living. Patient progress has been monitored by a variety of different outcome measures. Davis utilized the Short Form-36 and a 5-item hand-finger functioning subscale developed by the investigators (Hand Scale).32,33 This was found to have a moderate correlation with grip and pinch strength and weak correlation to the Semmes-Weinstein monofilament or sensory nerve conduction.11 Garfinkle used grip strength and pain reduction. Muller et al included sleep improvement, along with the other common measures.34 Psychological wellbeing, patient satisfaction, and work status have also been utilized. Yeoman published the Carpal Tunnel Syndrome Questionnaire (developed by Levine) to assess pain, numbness, weakness and tingling along with a functional status scale.11,35 This is reportedly more accurate than the SF36. Subjective evaluations, functional self-administered questionnaires and self –administered hand diagrams have been of significant value in establishing the diagnosis of carpal tunnel syndrome4,8,36 and have been used to assess progress. This study chose to utilize the patient’s symptoms, physical examination findings and neurodiagnostic testing as reliable criteria for diagnosis, based on the literature and clinical experience. The NCV lacked sufficient sensitivity to be used as an outcome measure or prognosticator of response to care. This concurred with the findings of Lazaro7,28 This study therefore utilized the CTSQ, along with symptoms and physical exam findings to assess outcomes.
Treatments Used: Since this study was conducted in a private office setting, multimodal therapies were commonly applied. This study observed the positive outcomes of these multimodal conservative therapies (manipulative therapy, ultrasound therapy, nutritional therapy, distraction therapy) with an emphasis on concurrent spinal and wrist manipulation. Although a conclusion could not be drawn as to the specific treatment efficacy, the functional improvement, symptomatic improvement, and improved physical exam findings were achieved with the conservative multimodal therapeutic applications. This suggests the need for further research to delineate the efficacy of the specific therapies.
Limitations: Multiple levels of neurological compromise either anatomically or physiologically, complicate the conditions described and subsequently the efficacy of the treatment to the related pathology. Multiple types of care are common in clinical practice but prevent the drawing of a definitive conclusion regarding any single specific treatment. Due to the small number of cases presented, the clinician should be careful about extrapolation to other patients.
CONCLUSION
This study was a prospective case series of patients with carpal tunnel syndrome. Conservative multimodal treatment was applied to all the patients and the outcomes were observed. The outcome measures in this study showed a high incidence in improvement of CTS by means of multimodal conservative care, including concurrent manipulative therapy of both the cervical spine and wrist. A high concordance rate of cervical complications of carpal tunnel syndrome is observed in the patients involved with this study. Clinicians are advised to investigate proximal nerve root anatomical and/or physiological lesions that might cause Wallerian degeneration and predispose the patient to CTS. This may provide more consistent outcomes from conservative care and decrease the need of surgical intervention. Further clinical research is needed. The Carpal Tunnel Functional outcome is proposed as a measuring tool that concurs with Patient-Oriented Evidence that Matters (POEMs) to evaluate the outcome of conservative therapies for CTS for future studies.
Ethics Approval & Patient Consent to Participate
Authorization for research uses and disclosures of health information was obtained by each potential patient participant. Internal Review Board approval is not applicable, as study was performed in private practice.
Consent for Publication
Informed written consent was received for publication of the manuscript and figures [the information in the figures/manuscript]: Written informed consent was obtained from the patient/participant for publication of their individual details and accompanying images in this manuscript. The consent form is held by the authors/by the authors’ in the patients’ clinical notes and is available for review by the Editor-in-Chief.
Conflict of Interest
The authors declare that they have no competing interests
The author has not at any time received any payment from a third party for any aspect of the submitted work (including manuscript preparation and has no competing interests to divulge.
Funding
This project was self-funded by Multimed Center, Inc. & David N. Taylor, DC, DABCN, FICCN. There has been no payment or services from a third party (government, commercial, private foundation, etc.) for any aspect of the submitted work (including but not limited to grants, data monitoring board, study design, manuscript preparation, statistical analysis,
Author’s Contributions
David N. Taylor, DC (DT) conceived of the study and participated in its design and coordination and drafted the manuscript, participated in the design of the study, performed the statistical analysis and revised the manuscript. DT read and approved the final manuscript. DT contributed the following:
Project concept development & design, supervision, organization & implementation, writing of manuscript, data collection/processing, data analysis, interpretation, literature search, critical review.
Availability of data and material
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Trial registration
University Hospital Medical Information Network # UMIN0 00036619;April 28,2019


_indicates_a_paradoxical_.png)

_indicates_a_paradoxical_.png)