INTRODUCTION
Parkinson’s Disease (PD) “is a progressive movement disorder characterized by bradykinesia, resting tremor, muscular rigidity, and the loss of postural reflexes”.1 Symptomatically, PD patients often experience the following: pill-rolling tremors, bradykinesia, limb rigidity and dyskinesia, as well as problems with both gait and balance. In 2015, the CDC reported that PD is the 14th leading cause of death for Americans as well as the second most common neurodegenerative disease.2 Currently, there is no standard of treatment for PD. Treatments vary based on the individual symptomatology of each patient; however, the majority of treatments involve the use of dopamine promoters, most commonly levodopa.
Complementary therapy is sometimes used by patients in addition to their medication or current therapies. Spinal manipulation, used by various professions, has been used as an ancillary treatment for patients with PD. While the exact mechanism of action of SM is unknown, there are a wide range of theories. These include changes to both the autonomic and sympathetic nervous systems, as well the potential influence on the hypothalamic-pituitary-adrenal (HPA) axis.3,4 Most of the evidence reported by practitioners using SM on PD patients are case reports, which helps to emphasize the need for the performance of higher-level research.
Regarding the initial assessment and diagnosis of PD is difficulty associated with early detection. The majority of PD diagnoses are made after 60% of the dopamine neurons have been destroyed, allowing the manifestation of physical symptomatology.2 When PD is diagnosed, the disease is tracked with different scales, including the Unified Parkinson Disease Rating Scale (UPDRS). This scale is considered the “gold standard” of PD measurement.2 Other commonly used scales are the UPDRS, Hoehn and Yahr Staging, and the Schwab and England rating of Activities of Daily Living.2,5 Patient subjective reports are also frequently used by clinicians, but make assessment difficult due to the lack of standardization.
METHODS
A systemic search strategy was developed to identify literature related to spinal manipulation and its effects on PD symptoms. We searched the following databases up to August 2018: Academic Search Premier, CINAHL Complete, MEDLINE Complete, Primary Search, Alt HealthWatch, Information Science and Technology Abstracts, EBSCOhost, PubMed, and Index to Chiropractic Literature. We used manipulation OR chiropractic OR spinal manipulation OR manipulative medicine AND Parkinson’s OR Parkinson OR Parkinson’s Disease OR Parkinson Disease for the search terms for all the databases.
We reviewed the abstracts from all search results for relevant clinical studies on the use of spinal manipulation for the treatment of PD symptoms. The following criteria had to be met for us to include the article:
-
Subjects had to be human
-
Treatment was required to include spinal manipulation
-
The study had to have undergone peer review
-
Any studies that did not meet this criterion were excluded from being included
Main Outcome Measures
All studies had to use a form of spinal manipulation as part of the trial. While UPDRS is often considered the gold standard of measurement, there is still debate on if this is the best method of tracking the progression of PD.6 Patient subjective report is often considered crucial to early detection and tracking the progression of the disease due to subjective reports being an early indicator of PD developing in early stages.7
RESULTS
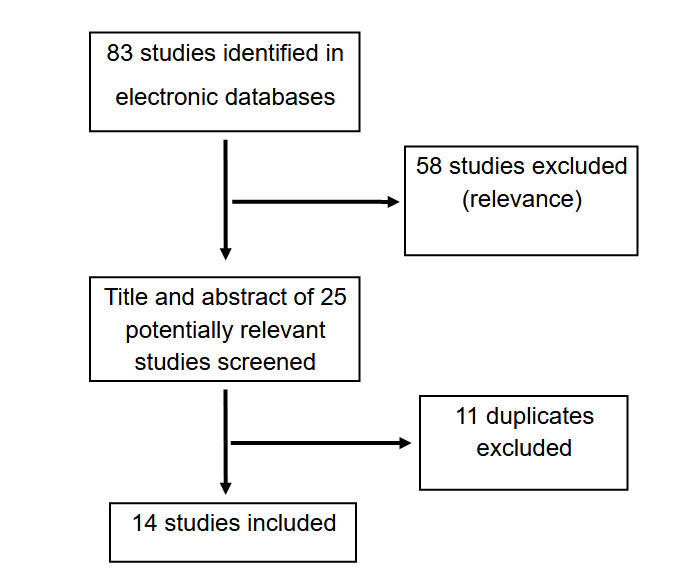
Fourteen articles were found to be either clinically relevant and/or met the criteria (Figure 1).
Figure 1.PRISMA flow chart.
A search in CINAHL, Academic Search Premier, Alt HealthWatch, MEDLINE Complete, and Primary Search using the terms Chiropractic and Parkinson’s Disease yielded only 4 results that met the criteria.1–3 When we expanded to Spinal Manipulation, there were only 2 results that were duplicates of the other search. Changing Spinal Manipulation to Manipulative Medicine yielded 7 results, with two results meeting criteria.2,3 A search in Index to Chiropractic literature with Parkinson’s gave 39 total articles, with 13 relevant and meeting the criteria; out of the 13, 4 were duplicates of the earlier searches.4–12 PubMed search of Chiropractic and Parkinson’s gave only 7 results, with only 2 relevant results, which were both duplicates of earlier searches. Changing Chiropractic to Spinal Manipulation gave only 6 results, with 1 relevant article that had been found earlier. (Table 1 provides information on each paper).
Table 1.Evidence table of information.
| Study ID |
Intervention |
Outcome Measurement Utilized |
Results |
| Bello 2011 |
1. NUCCA chiropractic technique |
Patient subjective report |
Patient reported that her fatigue, depression, and resting tremor in left hand had gone away. She also reported that her coping skills had returned, all tightness in her muscles had ceased, and she had regained use of her left arm and leg. Patient still had rigidity in her third left toe on occasion.8 |
| Bova 2013 |
1. Blue lensed glasses
2. Vibration therapy
3. Mirror imaging
4. Cross-crawl exercises
5. Chiropractic manipulation |
Parkinson’s Disease Questionnaire |
PDQ was 15 at time of intake and 9 at the end of 2 months of treatment. Patient had improvement in his writing ability, improved posture, reduction of a subconscious leftward lean, reduction in anterior flexion by 10 degrees, and patient began walking without assistance from his walker.6 |
| Bredin 2015 |
1. Diversified chiropractic technique |
Patient subjective report |
Patient reported an improvement in balance and that his symptoms only began improving once he began chiropractic care. Patient continued to take Disipal medication during treatment.9 |
| Chung 2011 |
1. NUCCA chiropractic technique |
Patient subjective report |
Subjective report of improvement in 60% weakness, 50% in tremors, and 0% in rigidity after one month of treatment. After three months, there was improvement in 50% weakness, 60% tremors, and 30% in rigidity. Six months of treatment resulted in 70% improvement in mobility and a decrease in the number of falls the patient had been experiencing.10 |
| DiFrancisco-Donoghue 2016 |
1. Osteopathic manipulative medicine |
1. Movement Disorder Society-Unified Parkinson’s Disease Rating Scale (MDS-UPDRS)
2. Sensory Organization Test (SOT)
3. Mini-Balance Evaluation System Test |
Study began with 11 subjects but only 9 completed the study. Patients were split into two groups with 6 receiving OMM for the first 6 weeks then counseling for the next 6 weeks. The other 5 received counseling first then OMM. SOT had no statistical significance but there was an increase in the overall composite score. The Mini-BEST had no apparent trend in changes for pre to post intervention of either of the groups, but there was improvement. The MDS-UPDRS showed more improvement in the pre to post OMM than from the control. The treatment effect was statistically significant in the group receiving control for the first 6 weeks then OMM for the following 6 weeks.11 |
| Elster 2004 |
1. Upper cervical chiropractic technique |
Patient subjective report |
Study composed of 37 patients, with 7 patients not included who discontinued the study. Out of the 37, 34 reported improvement: 16 were substantial, 8 were moderate, and 11 were minor. Three cases showed no change. Treatment ranged for 1 to five years with no symptom progressions reported in any of the 37 patients.12 |
| Elster 2000 |
1. Upper cervical chiropractic technique |
UPDRS |
Patient reported a return of his balance and being able to ride his bike once again. UPDRS was taken originally with a rating of 32/74 as an on/off stage of when his medication was working and was not working respectively. Week 4 scores were 20/56 and the final score taken at 12 weeks was 13/47. There was a 43% overall improvement between the beginning and final UPDRS scores.13 |
| Friedman 2017 |
1. Upper cervical chiropractic technique |
Patient subjective report |
Patient originally complained of right-sided tremors, memory loss, balance issues, constant leg pain, occasional poor circulation, decreased muscular strength, and the need for a walker. After initial adjustment, patient no longer needed a walker for assistance and his tremors were decreased. Patient was seen for 6 months and reported his symptoms appeared to be regressing and decreasing; he mentioned that he was now taking half of the Levodopa he was originally taking.14 |
| Landry 2012 |
1. Upper cervical chiropractic technique |
1. SF-36
2. PDQ-39 |
PDQ-39 had a decrease in score (a sign of a better quality of life) in mobility, emotional well-being, stigma, cognitive impairment, and bodily discomfort. There was an increase in score for activities of daily living. There was no change in social support or communication scores which were both 0% pre and post.
SF-39 had an increase in score (a higher percentage shows a better quality of life) for physical component summary, mental component summary, bodily pain, physical functioning, and mental health. The score for general health remained unchanged.15 |
| Malachowski 2011 |
1. Upper cervical chiropractic technique |
Neurological exam |
Patient received a neurological evaluation on intake then was re-evaluated at 12 weeks. He showed a decrease in positive neurological tests of the following: CN VII, dysmetria, and Rhomberg. Dysmetria was originally positive bilaterally, but post-test was positive on the left and negative on the right. Patient also reported being able to rise from a sitting to standing position more easily and being able to hold his head up to look at people while ambulating.16 |
| Malachowski 2014 |
1. Upper cervical chiropractic technique |
UPDRS |
Three patients were involved in the study. Patient one had an intake UPDRS score of 25 and received care for three months with a UPDRS score of 15 taken at month 2. Patient two had an intake score of 27 and received care for 6 months with an updated score of 15 at month 5. Patient three had an intake score of 39, receiving care for 3 years and an updated score of 16 at 36 months.17 |
| Norton 2013 |
1. Activator Method
2. Postural exercises |
Objective range of motion measurements |
Patient had symptoms that included resting tremors in her hands, fatigue, lack of motion in the cervical and lumbar spine with associated neck pain and stiffness and lower back pain. Patient was adjusted eleven times over the course of sixty-day treatment plan; at the end of the care plan, patient reported an improvement in motor abilities and a decrease in the frequency of tremors. The decrease in tremors occurred prior to the beginning of prescription medication, meaning the reduction in symptoms could have occurred because of the medication.18 |
| Shapiro 2012 |
1. Chiropractic Biophysics technique |
Patient subjective report and objective findings |
Patient’s range of motion was taken during the assessment yielding the following findings:
ROM:
Cervical- Flexion 40o, Extension 25 o , RLF Flexion 10 o, LLF 5o, R/L Rotation 65 o.
Lumbar- ranges of motion were the following: Flex 65 o, Ext 15 o, RLF 10 o, LLF 10 o, R/L Rot 10 o.
MMT:
2/5 muscle weakness:
- neck extensors
- right and left l cervical lateral flexors
- trunk flexors/trunk extensors
DTRs:
All reported as either absent (0) or somewhat diminished (1+).
Positive orthopedic tests:
- Cervical compression
- Shoulder compression
- Jackson’s compression
- Max cervical compression
- Minor’s sign
- Patrick’s
- Milgram’s
- Ely’s
- Yoman’s.
Patient received 3 visits a week for 12 weeks before tests were reperformed.
Post treatment findings:
ROM:
Cervical- Flexion 40o, Extension 34 o , RLF Flexion 25 o, LLF 25o, R/L Rotation 70o.
Lumbar- ranges of motion were the following: Flex 70o, Ext 10o, RLF 20 o, LLF 20 o, R/L Rot 15 o.
MMT:
5/5 muscles:
- neck extensors and flexors
- left lateral cervical flexors
- trunk flexors
4/5: muscles:
- R lateral neck flexors
- Trunk extensors
DTRs:
All reported as normal (2+)
Positive orthopedic tests:
- R. max cervical compression
- R SLR
- Patrick’s
- Yeoman’s
Patient also reported the following improvements: neck pain 30%, double vision 50%, lack of energy 40%, unexplained weight loss 20%, right hand weakness 40%, bilateral knee pain 50%, low back pain 50%, left hip pain 90%, bilateral calf cramping 80%, bladder leakage 50%, erectile dysfunction 30%.19 |
| Wells 1999 |
1. Osteopathic manipulative medicine |
Gait analysis |
Twenty total patients participated with ten as a sham group and ten as a treatment group. There was also eight people as a control group in the study. All patients were required to undergo a 10-hour washout of their medication. Gait analysis was taken of stride length, cadence, shoulder velocity, arm movement velocity, wrist movement velocity, and lower limb velocity of hip, knee, and ankle. Analysis was taken prior and immediately after the adjustment or sham adjustment. The Parkinson’s patients showed significant increases in gait parameters related to stride and velocity for the upper and lower limbs compared with their pretreatment values. Cadence increases slightly but not significantly. The normal and sham-treated patients had now significant changes compared to their pretreatment values.20 |
DISCUSSION
We would like to note that there are several weaknesses in this review. These include the variability that occurs within the disease progression, the diagnoses being made at different times throughout the progression, the amount of time on pharmacological intervention, the presence of other therapies not accounted for, and the focus on purely subjective patient reports, to name a few. Within the subject improvements reported by patients, we cannot infer how long the improvements will last or whether or not these improvements would halt further deterioration. Additionally, the presence of only 1 study using a sham adjustment and the large number of case reports, while previously discussed, must be mentioned again as a significant weakness for this study. These limitations will be discussed in future publications on the topic of PD and alternative treatments.
We are unable to say there is a statistical significance in the use of spinal manipulation for the treatment of Parkinson’s symptoms; however, there appears to be clinical significance.11 While statistical significance is historically considered more important, clinical significance yielded from case reports is important because it helps create a hypothesis for future studies.17 The studies that were found and met the criteria for inclusion noted improvement in patient symptoms. This clinical significance is clearly important to the patient. Another plus to consider is that spinal manipulation is also considered safe, with little risk to the patient.11
CONCLUSION
With an growing and aging population in the United States, there is an increase in the prevalence of Parkinson’s Disease. According to 1 study, we can predict between 700,000 to 770,000 cases of PD, depending on a decrease or increase in smoking prevalence.16 With a significant outlook in the increase of cases, it is important that research be performed now to prepare for the current outlook. Further research needs to be performed in the use of spinal manipulation for PD symptoms. Until higher quality, long-term studies are able to be performed, it can not be concluded that spinal manipulation is an effective treatment for Parkison’s Disease and/or its symptomatology.
Acknowledgements
We would like to express our gratitude to Edward Murphy for his assistance in obtaining the full-text articles used in writing this review.
Funding sources and potential conflicts of interest
No funding sources or conflicts of interest were reported for this study.