INTRODUCTION
Neck pain is common and has a considerable impact on individuals and their families, communities, health-care systems, and businesses.1–4 At least 33% and as high as 65% of people have suffered and recovered from an episode of neck pain within the last year.1 Neck pain can be a disabling condition and, in most cases, is marked by periods of remission and exacerbation running an episodic course over one’s lifetime.1,2 Women are more likely than men to develop neck pain and are more likely to suffer from persistent neck problems.1–4 Of all 291 conditions studied in the World Health Organization (WHO) Global Burden of Disease 2010 (GBD) study, neck pain ranked 4th in terms of disability and contributes to an economic burden of billions of dollars in costs associated with treatment and lost work time.5 The estimated cost of neck pain in The Netherlands alone in 1996 was $686 million USD.6
Anxiety defined by the American Psychological Association as an emotion characterized by feelings of tension, worried thoughts and physical changes like increased blood pressure is the most common of psychiatric diagnoses.7 The prevalence of anxiety disorders (ADs) is difficult to pinpoint given frequent changes in diagnostic criteria but studies suggest that ADs afflict 15.7 million people in the US each year and 30 million people at some point in their lives, which impose high individual and social burden, tend to be chronic and can be as disabling as somatic disorders.8 The first GBD studies suggest that mental disorders, as a group, are the most costly diseases worldwide and subsequent studies suggest that the GBD underestimated the costs of anxiety and stress disorders though ranking them as the 6th leading cause of disability.9,10 As far back as 1990, the annual cost of ADs was estimated at $42.3 billion.11 Generalized anxiety disorder (GAD) patients are high users of primary care resources, effect women more frequently than men and are more prevalent in mid-life (females over age 35).12
Anxiety and depression are prevalent in chronic neck pain patients and studies suggest that pain is associated with the recurrence of depressive and anxiety disorders.13,14 As with neck pain and ADs, there exists a higher prevalence of chronic pain conditions among women.15 The total economic burden of chronic pain was estimated at $560-$635 billion – greater than the cost of heart disease, diabetes or cancer.16
Benefits of chiropractic management for chronic spinal musculoskeletal complaints have been well documented.17–19 To date, there is limited evidence to support the chiropractic management of anxiety and/or depressive disorders. However, patients suffering from these disorders may seek complementary and alternative therapies.20 The focus of this report is to present evidence of the reduction of perceived anxiety, a decrease in salivary cortisol (a biological marker for stress) and an improvement of musculoskeletal symptoms in a patient undergoing chiropractic management.
CASE REPORT
History
A 40 year-old female had a 2-week history of chronic, recurring neck pain and headache that was exacerbated by an increase of desk and computer work. She reported constant pain described as tension throughout the upper back and neck. Her pain waxed and waned in severity and worsened when sitting at a desk and driving. It improved with movement. Her headaches were daily and worsened as the day progressed while sitting at a computer. She indicated that her headaches were mostly in the suboccipital region and occasionally in the bilateral temporal regions. Her symptoms further interfered with gaining a restful sleep. She rated both her neck and headache pain as a 7/10 on a Visual Analogue Scale.
She also completed the Neck Pain Disability Index (NDI), where she scored 30/50 or 60%. Studies have shown the NDI to have a high degree of reliability and internal consistency appearing to be sensitive to the levels of severity of complaint and to changes in severity in the course of treatment.21
She also reported a history of anxiety, which seemed to worsen with increasing severity of her musculoskeletal complaints. She had not been evaluated elsewhere for anxiety. She rated her anxiety as a 7/10 on the Visual Analogue Scale for Anxiety (VAS-A). She also completed the PHQ-4, an ultra-brief screening scale for anxiety and depression. Increasing PHQ-4 scores were strongly associated with functional impairment, disability days, and healthcare use and demonstrates that anxiety has a substantial impact on functional status independent of depression.22 Her self-reported scores revealed a 5 out of 6 for anxiety and 1 out of 6 for depression. Her score in the depression category suggested a negative result; however, her score in the anxiety domain was greater than 3 suggesting a positive result for that domain and was further evaluated by GAD-7, as recommended. She scored a 15 on GAD-7, a valid assessment for Generalized Anxiety Disorder,23–26 indicating severe anxiety. Scores of 5, 10, and 15 are taken as cut-off points for mild, moderate and severe anxiety.
Examination
Chiropractic examination was performed using a battery of commonly used tests.27 Postural examination revealed a high left shoulder and anterior head carriage. Cervical spine range of motion (CROM) was assessed usign a single bubble inclinometer.28 Cervical flexion was 50⁰ and resulted in “tension,” left lateral flexion was 45⁰ and resulted in neck pain on the left, right lateral flexion was 35⁰ and resulted in left-sided neck pain, left rotation equaled 60⁰ and right rotation was measured to be 70⁰. Static palpation revealed hypertonicity of the upper trapezius, levator scapulae, sternocleidomastoid, pectoralis minor and suboccipital musculature bilaterally with trigger points noted primarily in the left upper trapezius, left levator scapula and suboccipital regions consistent with Upper Crossed Syndrome.29 Motion palpation revealed reduced and painful joint end-feel at C1-2, C5-6, T3-7. Examination also revealed cervical syndrome (fast) indicating C1 subluxation. Cranial nerves were assessed and reported as normal. Deep tendon reflexes of the upper extremities were graded +2 bilaterally. The Cervical Distraction test reduced local neck pain and cervical compression tests were negative. Radiographic examination of the cervical and thoracic spine revealed loss of the cervical lordosis, mild degenerative changes at C5-6 and a mild dextroscoliosis of the thoracic spine.
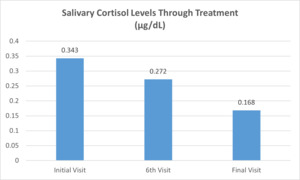
Finally, the patient agreed to providing a saliva sample to establish a baseline salivary cortisol level as a measure of stress. Analysis using enzyme-linked immunoassay (ELISA) revealed an average cortisol concentration of 0.343 μg/dL.
Intervention and Outcomes
Chiropractic care was provided for 12 visits over a 6-week period. She received specific chiropractic adjustments using Diversified Technique (contact-specific, high-velocity, low-amplitude) to correct identified vertebral subluxations on each visit. In addition to chiropractic adjustments, she was treated with Instrument-Assisted Soft-Tissue Mobilization (IASTM) utilizing the RockBlades® Mowhawk IASTM system and emollient by RockTape® (2001 TW Alexander Drive, Durham, NC 27709) at her upper trapezius, levator scapulae, sternocleidomastoid, pectoralis minor and suboccipital musculature to address hypertonicity, trigger points and associated myofascial pain.30,31 A home-exercise program was provided to address apparent Upper Crossed Syndrome.29,32
She reported steady improvement on the Visual Analogue Scale throughout the course of treatment. Re-evaluation occurred on the 6th visit after 2 weeks of care. Improvements in neck pain and headache were recorded on the NDI. She scored 14/50 (28%) indicating substantial improvement from initial assessment (a change of 5 points, or 10%, is considered significant). She reported slight, infrequent headaches during this visit. Initially, she noted moderate, frequent headaches. Anxiety was re-assessed with the PHQ-4 instrument. She scored 3/6 for anxiety, so GAD-7 was repeated, on which she scored a 9. Improved from the initial visit, this score indicated mild to moderate anxiety. Another saliva sample was collected at this time and upon analysis showed decreased salivary cortisol levels (0.272 μg/dL) compared to the initial, baseline sample.
Postural examination on the 6th visit revealed persistence of her high left shoulder and anterior head carriage. Global CROM was improved and less painful. There was continued hypertonicity of the involved muscles; however, no trigger points were present. Motion palpation restrctions existed at C1-2, T3-5. These findings represent a reduction in indicators for vertebral subluxation since the initial visit.
Re-examination again took place on the final visit (visit 12). She once again self-assessed using the NDI, PHQ-4 and GAD-7 questionnaires. Her score on the NDI was 3/50 or 6%, indicating significant improvement since beginning treatment. She reported a resolution of headache. She no longer had difficulty sleeping and had greater tolerance for and ability to perform her ADLs. PHQ-4 assessment resulted in a score of 2 out of 6 and though this represented a negative result for anxiety, GAD-7 was repeated, on which she scored a 4 – a negative result for generalized anxiety disorder. For a summary of the patient’s scores on these self-assessment tools on the initial, 6th and 12th visits (Figure 1). A final saliva sample was collected from the patient at this time and showed a reduction of salivary cortisol levels (0.168 μg/dL) compared to both the initial sample and the sample collected on the 6th visit (Figure 2).
Postural examination revealed at this time a slightly high left shoulder but no significant anterior head carriage. CROM was normal and did not elicit pain. Mild hypertonicity in the upper trapezius and levator scapulae muscles was noted on static palpation. Motion palpation revealed some restriction at C1-2 and T3-4. Chiropractic examination was negative for cervical syndrome. These findings represent a further decrease in the indicators for vertebral subluxation.
DISCUSSION
This report outlines the reduction of anxiety symptoms along with decreased salivary cortisol levels in a 40-year-old female patient receiving chiropractic adjustments for the reduction of vertebral subluxation. Additionally, she reported improvement in her chronic neck pain and a resolution of headache. This case suggests a correlation between perceived anxiety levels and salivary cortisol concentration.
Saliva samples were obtained to measure cortisol levels as an additional assessment for stress. Stress triggers the hypothalamus-pituitary-adrenal axis to release cortisol.33–35 Cortisol production has a circadian rhythm and the typical diurnal variation of cortisol secretion has been well established.33,34,36,37 Table 1 shows normal a.m. and p.m. salivary cortisol ranges in females of the patient’s age.38 This diurnal variation was taken into account as each sample was collected at the same hour of day (early afternoon); furthermore, cortisol levels have been shown to rise independent of circadian rhythm in response to stress.34,39 Cortisol can be obtained from blood or saliva. Salivary cortisol has been widely used as a measure of exposure to stress.33 Studies consistently report high correlations between salivary and serum cortisol levels.33,40–42 One study suggests that salivary cortisol determined by enzyme-linked immunoassay (ELISA) is preferable to serum total cortisol.43 This allows for the less invasive, more economical collection of saliva, which the patient can self-collect. Samples in this study were collected using passive drool techniques, which researchers consider to be the “gold standard”,44 and SalivaBio’s Passive Drool Collection Aids. Samples were then analyzed using Salimetrics® Cortisol Enzyme Immunoassay Kit specifically designed and validated for the quantitative measurement of salivary cortisol.
Studies on the effect of chiropractic manipulation on salivary cortisol levels are limited; however, a study by Whelan et al45 at New York Chiropractic College found that chiropractic manipulative therapy (CMT) did not significantly change basal salivary cortisol levels. One limitation of that study is that its subjects were asymptomatic adult male chiropractic students. A prospective case series by Tuchin et al46 investigating the effect of spinal manipulation on cortisol levels on 9 subjects over 6 weeks revealed a statistically significant reduction of cortisol over the course of the study but showed no apparent alteration in cortisol levels pre and post spinal manipulation and so considered the evidence to be inconclusive. A randomized clinical trial to determine the immediate effect of low back manipulation on cortisol levels in adult males with mechanical low back pain concluded that a neuroendocrine effect can be elicited by spinal manipulation.47
Patients suffering from anxiety and depressive disorders commonly receive psychotherapy and pharmaceuticals for anxiety and depressive disorders.17,48 Side-effects of anti-depressants and benzodiazepines, most commonly prescribed for anxiety and depressive disorders, are well-documented. These adverse effects can decrease compliance and delay recovery.49 Side effects can be mild and self-limiting or as serious as increasing the risk of suicide.49 Adverse effects of anti-depressants are usually underreported in clinical trials and large scale naturalistic studies are restricted to 6 months of use.50
Though there is limited evidence to support the chiropractic management of anxiety, there are studies outlining the use of chiropractic care for anxiety and stress disorders. Russell et al described improvement on PHQ-4 and Health Wellness and Quality of Life questionnaires after treating a patient with a 3-month history of anxiety and panic attacks for chronic low back and neck discomfort.17 Roth et al reported significant decreases in both GAD-7 and PHQ-9 scores across treatment in 5 of 6 patients who also reported decreases in muscle tension and pain and increases in mental clarity and physical energy.51 A 19-year-old female diagnosed with GAD reported a 50% reduction in anxiety after the first adjustment.52 Additional case studies have described improved quality of life and reduction or resolution of anxiety and/or depression.53–55
While patients are more likely to seek out chiropractic care for pain than anxiety disorders, as was the case here, evidence shows a strong correlation between the 2.13–16 In reporting the results of a survey on the use of complementary and alternative therapies, Kessler et al found over 50% of respondents with anxiety attacks and/or severe depression reported using complementary and alternative therapies to treat those conditions over the prior 12 months, though only about 20% visited a complementary or alternative therapist.20 This paper also reported that the use of complementary and alternative therapies for the treatment of anxiety and depression is considerably higher than that reported for any other physical condition with exception of back and neck pain (in which chiropractic is common) and further predicts that the use of such therapies is likely to increase.20 This suggests that patients are seeking alternatives to standard approaches for the management of mental health. Chiropractors must be mindful of the prevalence of anxiety disorders in their chronic pain patients.
Assessment and correction of the vertebral subluxation is a central theme in clinical chiropractic practice. Chiropractic patients report healthcare benefits beyond a period of therapeutic care and their presenting complaints.56 This case report documents the improvement of both anxiety and musculoskeletal symptoms in a patient receiving CMT for the correction of vertebral subluxation.
Limitations
Though the patient in this case reported a history of anxiety and self-assessment tools suggested this to be true, she was never formally diagnosed with generalized anxiety disorder by a mental health provider.
As with the collection of any biological sample, there is the possibility of contamination, bacterial growth, etc. that may compromise assay performance.
Limitations of this study include those inherent to a single case report. Results contained herein cannot be generalized. Higher-level studies such as randomized clinical trials should be conducted to explore the effectiveness of chiropractic manipulation on both musculoskeletal and non-musculoskeletal conditions.
CONCLUSION
Chiropractic management of chronic, recurring neck pain and headache in a 40-year-old female with anxiety was associated with improvement in both musculoskeletal and anxiety symptoms resulting in improved physical function. There appeared to be a correlation between the her perceived anxiety and salivary cortisol levels. This provides an argument for the use of chiropractic management of patients with generalized anxiety disorders and chronic pain. Given the prevalence of both anxiety and chronic pain, the frequency at which they co-occur and the significant individual, social and economic burden that is associated with these conditions along with the demand for complementary and alternative approaches that seemingly exists, there is a need for further research into the role chiropractic may play in mental health.
ACKNOWLEDGEMENTS
I thank the Department of Biology at Frostburg State University for the use of their laboratories, where the saliva samples in this case were analyzed.