INTRODUCTION
Excessive thoracic hypokyphosis, also known as ‘straight back syndrome’ (SBS)1,2 was first documented in 1960 by Rawlings and is defined as the congenital loss of normal physiologic thoracic kyphosis, particularly the mid to upper portion. Problematically, this deformity biomechanically decreases the distance between the spine and the sternum and may compress internal structures, including the heart and lungs.1,2
Common symptoms associated with SBS includes back pain and exertional dyspnea; as well, it may mimic congenital heart disease as it often presents with either a mechanical heart murmur or a false heart enlargement.2 A false enlarged cardiac sign, also known as ‘pancake cardiac silhouette sign’ on a chest x-ray, simulates cardiomegaly.3 Although diagnostic features of a systolic murmur are often present in SBS patients, these symptoms are considered benign.4 Regarding systolic murmur, however, Spapen et al. notes that this is associated with mitral valve prolapse, a condition linked with significant morbidity and mortality, and that this may be underestimated in SBS patients.5 The incidence of SBS is unknown,6 and the definitive diagnosis for SBS is made from the lateral thoracic x-ray6,7 or CT scanning.8,9
Although severe SBS, including lordotic thoracic spinal deformity, necessitates spinal surgery,10–12 less pronounced deformity may be amenable to non-surgical spinal rehabilitation. Only 3 case reports have documented successful non-surgical improvement in increasing the thoracic kyphosis in patients with SBS.13–15 Brooks reported a 16° improvement in thoracic kyphosis in a patient with kyphoscoliosis (not exclusively SBS) over a 4-year time span.13 Treatment varied over the time period and consisted of deep tissue massage, outpatient psychological therapy, daily exercises focusing on mobilization of the chest wall and spinal manipulation. Mitchel et al. reported a 10° increase in thoracic kyphosis in a 33-year-old over 16-weeks.14 There was resolution of both back pains and exertional dyspnea and a greater than 2 liter increase in lung capacity, which was maintained at a 7-month follow-up. Betz et al. reported a 14° increase in thoracic kyphosis in an 18-year-old over 12-weeks.15 There was relief of exertional dyspnea and back pain that was maintained at a 2.75-year follow-up. Importantly, there was also an increase in the antero-posterior thoracic diameter as well as the ratio of the antero-posterior to transthoracic diameters, two anatomical measurements critical to the wellbeing of SBS patients.
In the current report we discuss improvement in thoracic kyphosis and reduction of associated forward head posture in a patient suffering from back pain-related to SBS who was treated with CBP technique.
CASE REPORT
An 18-year-old male sought care for low back pain (LBP) he had had for 2 months. He strained his back while lifting weights while squatting. He also noted cramping in lhis eft calf and right quadriceps muscle and tended to toe walk. He also had exercise or allergy-induced asthma.
He stood with visible head flexion and a high left shoulder. Spinal range of motion (ROM) assessment was unrestricted in the low back, though elicited pain in all directions and was restricted in left lateral bending in his cervical spine. Deep tendon reflexes were normal except the right patellar reflex was a 1+. Dermatome and myotome testing were unremarkable.
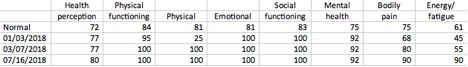
He rated his middle back pain a 3-5/10 and the lower back a 2-5/10 on a Visual Analogue Scale (VAS).The patient scored 10% on the Oswestry low back pain disability index (ODI),16 and scored low on the role-physical, bodily pain and energy/fatigue subscales on the Short-Form 36 question quality of life health questionnaire (SF36) (Table 1).17
A full-spine radiographic assessment was completed with the patient in the neutral standing position with the feet hip-width apart (Figures 1, 2). All images were digitized using the PostureRay software analysis system (PostureCo, Inc., Trinity, FL, USA). This system incorporates the Harrison posterior tangent (HPT) method (lines placed on the back of the vertebral bodies) to measure the sagittal plain spinal contours both intersegmentally (Relative Rotation Angle: RRA) and regionally (Absolute Rotation Angle: ARA).18–21 This method has a standard error of measurement of about 2° and is reliable and repeatable, as is standing posture.22
The patient was diagnosed with thoracic hypokyphosis SBS, having an ARA measurement from T1-T12 of 19.5° [vs. 43.7° normal23] (Figure 1). The patient also had cervical hypolordosis [C2-C7 ARA = -20.3° vs. -31-42° normal24,25] (Figure 2), reduced Atlas plane line [-17.6° vs. 24-29° normal24,26], and lumbar spine hypolordosis [L1-L5 ARA = -31.9° vs. -40° normal27], and an increased sacral base angle [45° vs. 40° normal27].
The patient was treated 3 times per week for 8 weeks with Chiropractic BioPhysics® (CBP®) technique. CBP is a whole-spine and posture correcting method using mirror image® exercises, spinal adjustments, and spinal traction.28,29 The primary treatment goal for this patient was to increase the thoracic spinal curve.
The patient performed 3 in-office exercises. The first exercise (Figure 3) consisted of placing a Prolordotic neck exerciser band (Circular Traction Inc., Huntington Beach, CA, USA) around the base of the neck and to elongate the strap by extending the arms forward, then to round the shoulders and flex the thorax before extending the head – this order prevented the patient from extending the upper thoracic spine. Each repetition was held for 5 seconds. The second exercise (Figure 4) consisted of placing a 10-pound thoracic-flex traction body weight (Circular Traction Inc., Huntington Beach, CA, USA) around the base of the neck and then to alloy it pull the upper back downward. A strap was placed at the thoracolumbar junction to stabilize the lower spine and to focus the majority of the bending in the upper thoracic spine. This position was held for 2 minutes. The third exercise (Figure 5) involved crossing the arms and grabbing the shoulders to pull the upper back downward. When the patient felt his thoracolumbar junction start to move, he was instructed to hold for 5 seconds and then repeat. A block was placed behind the pelvis to stabilize the movement and prevent postural shifting. This is a dynamic exercise that encourages both movement and isometric strength. All exercises took 8 minutes to complete and were performed on a PowerPlate® 3D vibration platform (Performance Health Systems, Inc., Northbrook, IL, USA) to increase the intensityof the exercises.30
The patient also received prone spinal manipulative therapy (SMT) as well as instrument-assisted paraspinal muscle stimulation with a bolster positioned under the chest to induce forward rounding of the thoracic spine. Spinal traction was performed in the prone position on a recumbent Universal Traction System® (UTS® Las Vegas, NV, USA) pulling up at T7 while strapping the lower and upper thorax down (Figure 6). Traction duration was increased each session until the duration of 20 minutes was achieved and maintained thereafter.
The patient was prescribed a home rehabilitation routine to compliment the in-office treatment. The Prolordotic-assisted exercises as previously described; laying supine over a cervical Denneroll traction block to be placed in the mid neck for a duration of 15-20 minutes daily; laying prone over an Erikson prone traction wedge similar to the traction set-up as described above for a duration of 15-20 minutes was to be done at home daily. Cryotherapy was to be used after the home routine if necessary. The patient consented to the publication of treatment results including any and all x-rays and pictures.
Results
An assessment was performed on March 7, 2018, after 24 in-office treatments over a 9-week period. The patient reported the LBP to be 100% improved, the asthma symptoms to be 90% improved, the muscle cramping to be 90% improved, and the toe walking tendency to be 70% improved. The patient scored a 2% on the ODI, had substantial improvements in three SF36 health indices, and now rated both the mid and LBP to be a 1/10 on average, and a 2/10 at worst. Physical assessment revealed all ROM tests were pain-free and within normal limits and all other tests were unremarkable.
Radiographic assessment revealed a clinically significant increase in the thoracic kyphosis of 15° (T1-T12 ARA: 34.6° vs. 19.5°), an increase in cervical lordosis (C2-C7 ARA: -28.2° vs. -20.3°), an increase in APL (-25.9° vs. -17.6°) and a decrease in sacral base angle towards normal (41.6° vs. 45°).
A follow-up assessment was performed 7.5 months after starting treatment and 4.25 months since ending intensive corrective care. The patient had received only 4 subsequent ‘stabilization’ treatments, approximately once per month. All subjective improvements were maintained. He rated the mid and LBP to be 0/10 ‘on average’ and 0/10 ‘at worst’ and scored a 2% on the ODI. The SF36 scores were also maintained with a greater improvement in the energy/fatigue health scale. Radiography revealed that the correction to the thoracic spine (T1-T12 ARA: 36.5°) was maintained as was the cervical lordosis (C2-C7 ARA: -27.6°) (Figures 1, 2).
DISCUSSION
This case demonstrates non-surgical improvement in thoracic kyphosis of 15° occurring after 24 in-office treatments as well as a home program over a 9-week time period. The improvements were verified to be stable at a 4-month follow-up. The improvements in posture correlated to improvements in pain, walking ability, muscle cramping, and exertional dyspnea originally reported as an exercise-induced asthma.
Although SBS is officially diagnosed on x-ray or CT scan, no official angle defines its presence. We recommend radiographic measurement is a critical assessment criterion to not only help in diagnosis but also to monitor for improvement after treatment. We used the HPT method as it is more accurate than a 4-line Cobb, and it also measures the spinal curve along its curve being consistent with an engineering analysis vs. the Cobb method that measures a cross-section to the spinal curve and which can be affected by a deviation in vertebral body shape.18,31 As assessed using the PostureRay analysis system, an average normal thoracic contoured line gets added to the patient’s image, aiding in a quick and accurate diagnosis.
There are different grades of SBS that may necessitate different treatment approaches. The surgical correction of severe SBS, when the thoracic spine is lordotic is described in the literature.10–12 Surgery is only recommended for SBS patients who have cardiopulmonary symptoms with severe structural thoracic lordosis of greater than 25-30°.11 As this case and others suggest, for mild cases of SBS (hypokyphosis), non-surgical intensive rehabilitation programs incorporating thoracic hyper-flexion protocols may prove to be the most effective approach to restore/improve normal physiologic kyphosis and simultaneously relieve related back pains and exertional dyspnea typically experienced by these patients.14,15
This case featured a 15° improvement in kyphosis in 9-weeks. The Mitchel case14 showed a 10° improvement in 16-weeks and the Betz case15 showed a 14° improvement in 12-weeks. Together, these three CBP cases show a 10-15° improvement in thoracic kyphosis over a 9-16 week duration which may be very clinically important. In the reduction of thoracic hyperkyphosis (THK), for example, several recent CBP case reports and 2 series show changes of 9-23° over durations of 9 weeks to 13 months32–37; the 2 case series showed an average improvement in THK of 11° over 9-10 weeks.32,33 Other non-surgical rehabilitation methods used to reduce THK do not typically use x-ray, but the 2 studies that did perform pre-post x-ray trials each showed only a 3° reduction over 6 months38 and 2 years.39
CBP methods may prove its effectiveness for SBS and other structural spine deformities as it incorporates patient-specific mirror image traction methods. We believe that sustained spinal traction in the reverse of a patient’s spinal deformity may be the ideal approach to reduce the deformity as this targets the viscoelastic properties of the intervertebral discs and ligamentous tissues.39,40 Spinal traction causes ligamentous tissues to biomechanically creep (deform over time) that causes plastic deformation (structure permanently deforming/lengthening)40,41; this likely contributes to the radiographically demonstrable spinal structural improvements as seen in the CBP treatment of THK,32–37 SBS,14,15 cervical hypolordosis,42–44 and lumbar hypolordosis.45–47 Although CBP methods involve exercises and spine and postural adjusting procedures, as demonstrated in several randomized trials, the traction is key to structural spine changes and successful long-term patient outcomes.42–47
The definitive diagnosis for SBS is obtained via radiographic imaging.6–9 While the utility of x-ray is well known in daily practice so too is the presumed risks from the radiation exposures. As recently discussed by many,48–54 concerns of future cancer risks from diagnostic x-rays or CT scans are based on a flawed linear model assumption. The linear no-threshold (LNT) model has been used by all major radiation safety committees for decades but now is undergoing scrutiny. Multiple articles by Calabrese have systematically documented that the 1956 recommendation of the US National Academy of Sciences Biological Effects of Atomic Radiation I Genetics Panel changed from a threshold model to a linear dose-response model for estimating risk assessment, was an ideologically motivated decision based on deliberate falsification and fabrication of the research record.55,56 There is no evidence that exists showing dangers to humans exposed to radiation levels lower than 100mGy; because x-rays are much less than this (1-3mGy),53,54 there should be no concerns about radiation exposures to patients receiving spinal x-rays for their back pains.48–54
Limitations to this case includes that it is only a single case. One may argue whether this case demonstrated a sufficiently straightened thoracic spine to be officially diagnosed as SBS. We argue that a thoracic curve having greater than 50% reduction in its normal physiologic alignment is pathological; whether termed SBS or hypokyphosis is essentially a semantics issue. Although there was a 4-month follow-up, a longer follow-up would prove better information as to the stability of spinal correction attained. We recommend more research into non-surgical methods to increase the thoracic spinal curve in SBS patients, although the rarity of the condition presents an obvious challenge for this endeavor.
CONCLUSION
This case demonstrates the improvement in both SBS and cervical hypolordosis corresponding to improvements in back pain and classic exertional dyspnea commonly associated with this disorder. The large structural improvement in thoracic curve is likely due to the unique and multimodal mirror image thoracic hyper-flexion traction and exercises used in the CBP treatment approach.

_image_showing_thoracic_hypolordosis.jpg)
_image_showing_forward_head_translatio.jpg)
.jpg)
.jpg)
.jpg)

_image_showing_thoracic_hypolordosis.jpg)
_image_showing_forward_head_translatio.jpg)
.jpg)
.jpg)
.jpg)
