INTRODUCTION
Trigeminal neuralgia (TN or tic douloureux) is described as recurrent attacks of lancinating facial pain along the dermatomal distribution of the trigeminal nerve.1 It is usually unilateral in presentation and is triggered by innocuous sensory stimuli.2 TN is rare and estimated to affect about 4-13 per 100,000 persons.1
Typical treatment options for TN include medications, surgery, and complementary approaches.1 First-line treatment approaches typically include anti-epileptic and tricyclic antidepressant medications.1 Carbamazepine is the drug of choice although other anti-epileptics including oxcarbazepine, baclofen, lamotrigine, phenytoin, and topiramate are also commonly prescribed.3 Multidrug treatment regimens are useful in selected patients.2 Surgical management of TN patients are reserved for those with severe, non-remitting symptoms, for those who have experienced failed pharmaceutical treatment with at least 3 medications, and/or for those who suffer from intolerable pharmaceutical side-effects.1
The surgical treatment of choice for treating TN is microvascular decompression (MVD).2,3 Other neurosurgical options include gamma knife radiosurgery, percutaneous balloon compression, glycerol rhizotomy, and radiofrequency thermocoagulation procedures.3 In some cases, partial sensory root sectioning may be indicated.3 Emerging techniques include deep brain and motor cortex neuro-modulatory stimulation as options to those patients who cannot use pharmacologic or surgical methods.1
Many mechanisms of pathogenesis may be involved in producing TN symptoms, such as pathologies at the trigeminal nerve root (compression or traction), dysfunction of the brain stem and basal ganglion or cortical pain modulatory mechanisms.3 Neurovascular compromise (NVC) is the prevailing theory of TN pathogenesis.1–3
Alf Breig pioneered the biomechanics of the central nervous system.4–6 He showed, using cadaveric specimens, that flexion of the cervical spine unfolded the cord and could traction the brainstem to the level below the tentorium and that cervical extension relaxes the cord tension, also relaxing the tension in the lower brain structures. In patients with TN, Breig noted that most could elicit facial pain on head flexion and stated “there are other, hitherto overlooked, mechanisms for the precipitation of trigeminal neuralgia, amongst them the elongation the spinal canal and stretching of the pons-cord tract accompanying flexion of the cervical spine or the whole column.”5
Breig was a neurosurgeon and recommended cervicolordodesis (CLD) to place the cervical spine in an extended position to relax the spinal cord and related neural tissues in the treatment of various neurological disorders including TN. Strong evidence suggests that extension traction methods as developed by Chiropractic Biophysics® (CBP®) technique methods may restore the lordotic cervical alignment in craniocervical patients presenting with cervical hypolordosis/kyphosis,7–15 and it also aids in improving neurological symptoms.8,10,13
This report describes the successful outcome of a patient suffering from TN who was treated by the correction of craniocervical posture by CBP technique methods. What is particularly interesting about this case is that after initial improvement in both craniocervical posture and TN symptoms, further treatment led to worsening of posture and reaggravation of TN symptoms, which was then followed again by an improvement in posture and the reduction of TN symptoms.
CASE REPORT
A 64-year old male developed TN following a dental procedure. Prior to seeking chiropractic care, he had received 2 nerve blocks that had provided temporary relief; when the pain returned, he underwent 2 stereotactic radiosurgeries. The first round of a highly concentrated dose of radiation to the right side of his head near the temporal area relieved his symptoms by about 75% for approximately 4 months. The second stereotactic radiosurgery failed. He was prescribed Neurontin but later switched to Tegretol™ (Carbamazepine), and was currently taking a dose of 800mg daily.
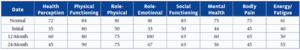
He reported his facial pain level to be a 7/10 on a numerical rating scale (NRS: 0=no pain; 10=worst pain ever). He scored a 16% on the neck disability index (NDI).16 The patient also scored lower than normal on all 8 indices of the short form-36 (SF-36) Health-Related Quality of Life Questionnaire (Table 1).17 All cervical ranges of motion were within normal limits; however, there was muscular rigidity upon palpation bilaterally along the cervical spine. All orthopedic tests were unremarkable, and facial sensation was also normal. He was active playing in the senior games, softball, and bowling leagues. He had constant “lightning-bolt” pain on the right side of his face and the stated that his medication only took the edge off.
Posture assessment (Figure 1) revealed a forward head posture, left head tilt, left head translation, right thoracic translation, and a right axial rotation of the pelvis.
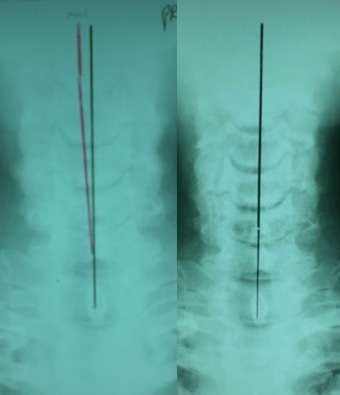
A full-spine radiographic assessment (Figures 2 and 3) was taken and analyzed using the Harrison posterior tangent method18,19 for the sagittal images and the modified Risser-Ferguson method19 for the coronal images. These methods are reliable and repeatable, as is posture.18–20 The images revealed a complete lack of cervical lordosis (absolute rotation angle from C2-C7=-1°; normal =34-42,21–23 forward head posture (FHP=35mm vs. <15mm normal22), and an atlas plane line (APL) of 10° (vs. 24-29 normal21,22) (Figure 3). The patient had well-demarcated osteoarthritic bone spurs from C4-C7 (Figure 3). On the posterior-anterior cervical radiograph, the patient had a left head translation of 7mm (vs. 0mm normal) (Figure 2).
Treatment Protocol
The patient started care with the goal of improving the craniocervical biomechanical postural parameters in order to provide pain relief from the TN. CBP technique is an evidence-based spine and posture correcting method that features mirror image® exercises, spinal adjustments, and traction methods.24–26 Much supporting evidence exists substantiating CBP methods as being effective for increasing the cervical lordosis7–15 and other craniocervical parameters.7–15,27 Typical CBP treatment regimens include sessions 3 times per week for 36 total sessions between assessments.25,26 This is the regimen that this patient received throughout care.
The patient received involved care (3 times per week) for approximately 1 year, and then was treated on a maintenance schedule (2 times per month) for another year. A timeline of events is reported in Table 2. The initial 4 treatments were aimed at loosening the cervical spine and to provide pain relief and involved spinal manipulative therapy (SMT) as well as cryotherapy. On the fifth treatment, structural ‘corrective care’ was initiated and included Chiropractic BioPhysics (CBP®) mirror image exercises, traction, and spinal adjustments. The patient performed right-sided head translation exercises and traction (www.berrytranslations.com, NY) (Figure 4), and received ‘instrument adjustments’ (Impac Inc., Salem, OR) (a handheld percussion instrument is held to the cervical paraspinal tissues and provides stimulation while the patient actively translates the head to the opposite position), as well as full-spine SMT.
The next 3-month block of care (3 treatments/week) was directed at correcting the sagittal posture of the head and neck and traction was changed to a static type ‘extension-compression 2-way’ (Figure 5). The patient also performed head retraction exercises (Figure 5). Upon re-assessment at the 6-month mark, the patient was transitioned to a more dynamic neck extension traction, ‘seated dynamic extension-compression 2-way’ traction which was thought to be more aggressive to continue the correction (Figure 5). After reassessment at 9-months, however, the patient had an unexpected regression of symptoms and craniocervical posture (Figure 3). Therefore, he was put back on to the original static neck extension traction (extension-compression 2-way), where after another 3-months (12-months total), the patient again experienced a significant relief of symptoms and thereafter, was put on ‘maintenance care.’ A 1-year follow-up assessment (two years total treatments) was also performed and is reported on. The patient gave verbal and written consent to the publication of these results.
Results
After the initial 3-months (Figure 2), his left head translation was completely re-aligned to midline. His pain levels remained a 7/10 and still complained of right-sided facial pains. After another 3-months of sagittal cervical static extension-compression 2-way traction (Figure 5), his pain intensity dropped to 2.5/10, and he also reduced his Tegretol use to 100mg/day (vs. 800mg/day initially). His FHP reduced (24mm vs. 33mm), lordosis increased (-17° vs. -1°), and APL increased (-20° vs. -10°).
Following another 3-months of a more dynamic type of cervical extension 2-way traction (Figure 5), he regressed, having a resurgence of pain levels (4/10) corresponding with worsening postural radiographic parameters (FHP increased to 33mm; ARA increased to -10°; APL reduced to -17°). He also increased his medication to 400mg/day. He was encouraged by his family to quit treatment, but he chose to continue as long as he could re-commence the former static extension-compression 2-way traction that had achieved the initial symptom relief.
He was put back on the initial static extension-compression 2-way traction that had resulted in the initial symptomatic relief. After 3 further months of treatment (12-months overall), he again improved having an NRS of 2/10, reducing FHP to 26mm, increasing ARA to -14°, and increasing APL to 14°. He was for the first time able to stop taking Tegretol, and also reported no facial ‘shock-like, lightning-bolt’ pains. He also improved on 7/8 SF-36 QOL indices (Table 1). This finalized 1 year of ‘corrective care,’ where, moving forward, he continued on a maintenance care plan (1-2 treatments per month).
A 1-year follow-up assessment (2 years since initial presentation) demonstrated he had maintained wellness, having an NRS of 2/10 and a further slight improvement of lateral craniocervical radiographic parameters (21mm FHP, -18° ARA, -22° APL). He had improved on half of the SF-36 QOL indices, though showed lower scores for half the indices, including pain possibly due to a recent onset of acute low-back pain due to cutting wood and playing softball. Regarding his former complaint of TN, he said he felt ‘the best ever’ and chose to discontinue further care.
DISCUSSION
This paper discusses improvement in trigeminal neuralgia symptoms in an older male after improving cervical spine posture in the sagittal and coronal planes. Interestingly, unforeseen regression of the patient’s sagittal cervical posture coincided with the re-emergence of neurological symptoms; these symptoms again diminished using a re-correction of the alignment accomplished by reperforming the originally successful cervical extension traction methods.
As mentioned, Breig4–6 illustrated in several books definitive causes of neurological impingements based on spinal positions, including cervical flexion as eliciting symptoms in patients with trigeminal neuralgia.5 This is because any flexion of the spine lengthens the spinal canal and leads to an unfolding the cord and nerve roots.4,5 Once a spinal position surpasses some threshold, normal physiological cord unfolding changes to abnormal pathological cord tension. This is where a patient’s poor (forward flexed) posture may lead to neurologic symptoms.
Since the correction of craniocervical posture may lead to improvements in neurological pathologies,8,10,13 it is logical that the correction of posture in patients with TN may also result in simultaneous relief of symptoms due to the reduction in pathologic tension in the pons-cord tract that may be tensioning the trigeminal nerve. The fact that our patient experienced initial relief with improved posture, then regression of relief with worsening posture, and then again, relief from TN pains coinciding directly with the re-improvement in posture confirms in this patient, that the cause was related to the spinal subluxation (forward head position and hypolordosis).
Why did the patient have a regression of posture during treatment? He was transitioned at the 6-month mark to a dynamic 2-way extension compression traction, as this type of traction is known to be more aggressive due to it being ‘dynamic,’ i.e. using gravity. For unforeseen reasons, he did not respond well to this altered type of traction; the reasons are still unknown, though it may be due to the amount of degenerative changes in the cervical spine, which presents a challenge to a practitioner attempting to re-align it, although it can be done.28
Further confirmation for the craniocervical posture induced TN theory for the current case is supported by the fact that former treatments received by the patient either failed or only provided short-term relief, and these included 2 nerve blocks, 2 stereotactic radiosurgeries and the use of the anti-epileptic pharmaceutical, Tegretol™, which the patient had been reliant on, consuming 800mg per day.
One can question the whether the treatment duration and number of treatments given to this patient were necessary, and/or ethical given recommendations to limit treatment number to 6-12 treatments and to provide care based on pain management only.29–31 As highlighted recently,32,33 there are evidence-based approaches to spine and posture correction that center on the reestablishment of spinopelvic parameters to achieve superior patient outcomes, beyond simple pain-based, spinal manipulation. CBP methods has a significant amount of research supporting its use in this context for patient care.7,34,35 Due to the presentation of challenging clinical presentations, frequent treatments over long durations may be necessary to achieve the best patient outcomes25,26 and has been presented in several recent published cases.36–39
The limitations to this case are that it is a single case report. Although there is a 1-year follow-up, the patient was receiving maintenance treatments (2x/month). The regression and reemergent symptomatology with the worsening of posture during the course of treatment, followed by the mirrored relief of symptoms by the continued correction in posture shows a unique trend of the TN symptoms correlating with the craniocervical posture. These findings also agree with Breig and point to the possible pathogenesis of TN by subluxated craniocervical posture. This also implicates the treatment approach for those suffering from TN by the correction of posture; this may be 1 cause of TN. Future research should examine this plausible mechanism in the pathogenesis of TN.
CONCLUSION
This case is interesting in that the correction, worsening, and re-correction of posture was directly related to the painful symptoms of trigeminal neuralgia. Subluxation of the craniocervical posture may be a plausible cause in some cases of this disorder. Radiographic assessment is necessary to quantify postural deformity in this disorder.
Conflict of Interest
RHB manufactures and sells ‘Berry translation’ traction tables as used in this case; PAO is a paid consultant to CBP NonProfit, Inc.; DEH teaches chiropractic rehabilitation methods and sells products to physicians for patient care as used in case.




_and_traction_(right)_in_the_coronal_plane._this_w.jpg)





_and_traction_(right)_in_the_coronal_plane._this_w.jpg)
