INTRODUCTION
Human spinal posture is fundamental to normal function as a bipedal being.1,2 Recent research found that altered spine alignment/postural subluxation, referred to as adult spinal deformity (ASD) is a global epidemic with serious and deleterious consequences for patient health-related quality of life (HRQOL).3 In fact, Pellise and the European Spine Study Group determined that HRQOL was worse for patients suffering from ASD, including having an anterior sagittal balance of greater than 50mm, than from the chronic health conditions of self-reported arthritis, congestive heart failure, diabetes, and chronic lung disease.3
Anterior sagittal balance by anterior thoracic posture causes great increases in physiologic disc loading and corresponding increases in extensor muscle loads required to maintain upright static equilibrium. Extensor muscle loads have been shown to increase almost 5 times normal and to correspond to a marked increase in compressive and shear intervertebral disc loads in the thoracolumbar spine.4 As stated by Harrison et al. “This posture is common in lumbar spine disorders and could contribute to lumbar disc pathology, progression of L5-S1 spondylolisthesis deformities, and poor outcomes after lumbar spine surgery.”4 Thus, successful methods to reduce anterior thoracic posture would benefit those suffering from this subluxation deformity.
This report discusses the reduction of severe forward sagittal balance in a geriatric woman with chronic low back pain (LBP) and sciatica using the non-surgical rehabilitation methods of Chiropractic BioPhysics® (CBP®) technique.
CASE REPORT
An 87-year-old female had a primary complaint of chronic low back pain (LBP) and sciatica. She was 172cm in height and weighed 58.5kg. She had had LBP and disability for the last 30 years. She noted a family history of osteoarthritis and osteoporosis. She had few injuries other than some minor falls. She reported she was always afraid of chiropractors and had never seen one for treatment. The only treatments she had received in the past included periodical massage therapy. Previously, the patient was prescribed FosamaxTM but was concerned about the pharmaceutical side effects and chose not take it. Other than her back pain, she had no other co-morbidities.
Physical Assessment
All lumbar range of motion (ROM) movements were restricted and painful. Straight leg raise was positive, as was the Valsalva maneuver for pain. The intensity of her LBP was rated as a 7/10 on a numeric pain rating scale (NPRS: 0=no pain; 10=worst pain ever), and her sciatica was rated an 8/10. The sciatic pains were bilateral and were more prominent down the left leg. HRQOL was measured using the SF-365 and revealed lower than normal scores for pain6; the component summary scores for physical and mental categories were 83 and 84, respectively.
Radiographic Assessment
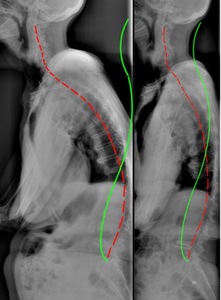
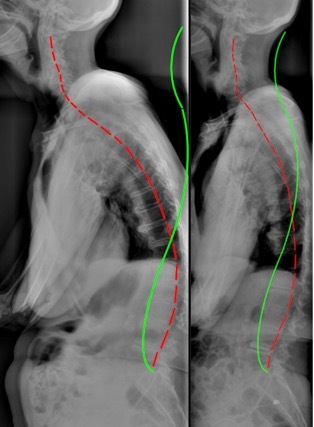
Radiographic examination was performed (Figure 1) and spinal alignment was measured by digitizing the images in the PostureRay software system (PostureCo. Inc., Trinity, FL, USA). This system used the Harrison posterior tangent method to measure regional and intersegmental vertebral angles and distances.7–10
The patient had extreme anterior sagittal balance, 175.2mm, as measured from the horizontal displacement from C1-S1, or 145.1mm, as measured from T1-S1. The lumbar lordosis L1-L5 measured +13.2° (vs. -40° normal11,12), the thoracic kyphosis T1-T12 measured 37.9° (vs. 44° normal13), and the cervical lordosis C2-C7 measured -28.4° (vs. normal -29-42°14–16). The forward head translation as measured as the horizontal distance from the posterior-superior C2 vertebral body corner to the vertical line drawn from the posterior-inferior C7 vertebral body corner measured 31.4mm (normal <15mm14,15).
Treatment
She was treated using CBP technique17–20 methods with the goal of improving the structural alignment of the spine and posture; specifically, to reduce the excessive anterior sagittal balance subluxation. CBP technique incorporates mirror image® (MI®) exercises, spinal adjustments and traction methods, as described elsewhere.17–20 These structural methods have been shown to offer superior long-term patient outcomes versus traditional or conventional physiotherapeutic interventions that do not achieve structural correction to the spine.21,22
She was treated for 24 sessions at a frequency of 3 times a week for 8 weeks before re-examination. Each treatment consisted of muscular stimulation with the patient laying prone with the headpiece of the treating table elevated, forcing the patient into a MI or extended position. Both the Arthrostim (Impac Inc., Salem, OR) and Impulse (Neuromechanical Innovations Inc., Chandler, AZ, USA) handheld adjusting instruments were used to stimulate the paraspinal muscles of the back. This is thought to act as mechanical massage and to also cause neuromuscular relaxation of the spine stabilizing muscles.23
She performed MI traction (Figure 2) in Target Force traction (Saugus, MA, USA). Laying supine, a padded strap was placed at the level of the thoraco-lumbar junction (TL: T12-L1), where it was connected to a spreader bar connected to a winch. An approximate vertical orientation of the pulling strap was set by tilting the frame over the flat bench. She would lay relaxed allowing us to tighten the pull on the TL area to a tension considered by her to be ‘comfortably tolerable.’ The traction was performed up to 18 minutes per session. Initially she began with a flat bench, but progressed to laying on a 6-inch, thick block placed under the thorax with her head supported but in an extended (posteriorly translated) position.
She also performed MI exercises (Figure 3). She stood with her back toward the wall with a block located at the thoraco-lumbar junction. Simultaneously, her pelvis and head were retracted backwards toward the wall. This position is held for a few seconds for each repetition. She worked up to 50 repetitions per visit. This exercise was also prescribed for homecare as was general stretching of the lower extremities.
Outcome
Upon reassessment she reported her sciatica to be alleviated on the right side and 90% resolved on the left side. Lumbar ROM improved and was now pain free. The SLR and Valsalva tests were also now pain free. On average, her sciatica was reported as 0/10 and the LBP as 2/10. The pain score on the SF36 improved to 57.5 (vs. 45), and both component summary scores improved for the physical (85 vs. 83) and mental (100 vs. 84) categories. She enjoyed the treatment protocol and was motivated by feeling relief right from the beginning of treatment.
Radiographic assessment revealed significant reduction in anterior sagittal balance (Fig. 1). The C1-S1 sagittal balance reduced to 66.5mm (vs. 175.2mm) and the T1-S1 sagittal balance reduced to 47.5mm (vs. 145.1mm). The lumbar lordosis improved to be slightly lordotic (-1.6° vs. +13.2°), the thoracic kyphosis increased towards normal (40.6° vs. 37.9°), and the cervical lordosis increased to within normal limits (37.3° vs. 28.4°). Anterior head translation reduced to 15.5mm (vs. 31.4mm).
DISCUSSION
This case shows the reduction of anterior sagittal balance and improvement of overall posture by non-surgical CBP technique rehabilitation methods in an elderly woman with significant spine deformity and 30 years of self-reported disability.
Significant ASD often requires surgical intervention.24 Although surgical reduction of sagittal plane deformity is predictably accomplished,25,26 there is a high risk of major complications, hospital readmissions, and unplanned reoperations.26,27 Thus, a non-surgical means to reduce such deformities is urgently needed. Although the evidence for CBP methods is now substantial,21,22,28–45 there is little support showing the reduction of severe spinal deformities such as seen here.
Although our patient was 87 years old, a dramatic improvement of the spine was accomplished in a short duration. This suggests that the elderly may not be as fragile as one may presume, and as long as the patient does not have outright osteoporosis, aggressive non-surgical spinal traction methods can be employed safely. Other than the main LBP complaint, our patient had no other comorbidities and probably represented an ideal senior patient for these procedures as she also described no major discomfort from the treatments.
Despite CBP spinal rehabilitative protocols taking longer than other methods to treat spinal deformity (i.e. surgery), it is safe and more cost-effective than spine surgery. Costs associated with spine surgery average about 120, 000 USD.6 Alternatively, costs associated with non-surgical CBP spine rehabilitation may accrue up to $3000-$5000 dollars; however, this is still less than 5% the cost of spine surgery.46
Although there is an increasing evidence base for CBP methods for improving spine alignment, particularly for increasing cervical and lumbar lordosis,21,22 trials have been limited to treatment durations of 10-12 weeks and to 30-36 treatment sessions. As described by Oakley et al.18 and demonstrated in successful spine deformity cases requiring extended treatment programs,47,48 to facilitate ideal spine alignment improvements (i.e. return the spine to an ideal/normal alignment), it may take several ‘blocks’ of corrective care programs which may span several months or more in severe cases. Thus, CBP methods is proving to be both an evidence-based and cost-effective treatment approach for patients with ASD.
The limitations to this case was that it is only 1 patient and cannot be generalized. Further, no long-term follow-up is reported. Due to the dramatic reduction of the gross spinal deformity, further research is recommended to ascertain the efficacy of these methods to treat patients with severe spinal deformity.
CONCLUSION
This case suggests that gross spinal deformities can be reduced by non-surgical methods, and that the improvement in gross deformity correlates with the reduction in chronic symptom burden. Although there is a substantial evidence base for the use of Chiropractic BioPhysics methods, research is needed for its use on patients having severe spinal deformities.
Conflict of interest
JWH and DEH teach chiropractic rehabilitation methods as used in this manuscript; PAO is paid consultant for CBP NonProfit, Inc.; DEH sells products for patient care as used in this manuscript.