INTRODUCTION
Lower extremity injuries are common in all sports, resulting in injury rates ranging from 60-100%.1,2 The ever-growing participation in sports-specific youth and adolescent training has contributed to the increase in youth and adolescent musculoskeletal injury rate, including muscular strains.2–4 Within the many events of track and field, muscular strains of the thigh are common due to the explosive nature, high rate of use, and rapid deceleration that occurs.1–3 The rectus femoris is the most commonly strained quadriceps muscle. This injury can result in extensive physical rehabilitation and treatment before an athlete may return to sport, especially sprint events.1–4 Sprinting requires a violent contraction of the rectus femoris to flex the hip into the triple flexion position, which provides a challenge to treatment and rehabilitation when injured.
The treatment of musculoskeletal conditions warrants an ever-growing desire for the best available conservative management options. Previous research indicated that isometric/eccentric strength training, various forms of manual therapy, and functional movement training may help manage rectus femoris strains.5–7 Collegiate track athletes with a quadriceps strain are typically restricted from activity for <7 days (83.8%).1,2 With acute strains, rest and limitation of physical activity is important; however, an active rehabilitation plan and treatment protocol to reduce inflammation is vital to maintain muscular strength at pre-injury levels. This case report discusses the use of multimodal chiropractic management for a grade 2 rectus femoris strain that resulted in increased sprint speed and overall performance of a high-school female track athlete within 14 days post-treatment.
CASE REPORT
An 18-year-old female track athlete sought care for a left quadriceps strain. The strain occurred 2 days prior to her visit. The injury occurred while practicing the 100m sprint. She was doing a light jog and then while transitioning into a sprint and pushing off with her left foot she heard a “pop” and felt an immediate sharp pain in her left quadriceps, mid-muscle region along its lateral aspect. Following the initial pain, she had difficulty walking. That evening she saw a physical therapist, who applied Rock Tape™ and told her to rest. When she saw us, her pain was an 8/10 at its worst and a 0/10 at best on the Numeric Pain Rating Scale. She indicated the pain was better than the date of injury. She had no pain at rest and aggravating factors included using the stairs and walking. She had not participated in any athletic events since the injury.
Initial examination revealed an alert, pleasant and athletic female. She had a slight limp, keeping weight off of her left lower extremity (LE). Deep tendon reflexes (DTR) were 2+ and symmetrical for the Patellar and Achilles reflex. Left hip flexion strength was 3/5 and left quadriceps strength was 3+/5. All other LE muscle strength testing was 5/5 and symmetrical. There were palpable muscle spasms that also evoked pain in her left vastus lateralis and rectus femoris, mid-muscle belly region. Functionally, she was unable to perform a body weight squat or lunge due to pain.
She was diagnosed with a Grade II quadriceps strain. Her initial treatment first consisted of instrument-assisted soft-tissue mobilization (IASTM) while she was lying in the supine position for 3 minutes over the entire distribution of the left quadriceps group as well as the distal psoas tendon. Manual muscle release of the vastus lateralis and rectus femoris was then performed. The doctor placed his contact hand just distal to the active trigger points with the quadricep group in the shortened position and then passively lengthened the quadriceps group. Following that, therapeutic exercises consisted of seated left knee extensions using a red Theraband™ (3 sets 10 reps), isometric quadriceps contractions at 1 second holds (3 sets 10 reps), standing hip flexion using a red Theraband™ (3 sets 10 reps) followed by standing hip flexion isometric holds with a red Theraband™ holding for 30 seconds (3x). This was then given as a home exercise program (HEP) to be done 3x/day. Lastly, Rock Tape™ was placed over the length of the quadriceps muscle. She was told not to participate in any athletic activities, nor run or jog, until her next appointment.
She returned the following day. Subjectively, she reported feeling better. She now had no pain while walking and noticed tension with max hip flexion, along with 6/10 pain. With resisted knee extension, the pain was 0/10. She then told us that she had subsectional races in 7 days and was hoping to compete in the 100m, 200m, and 400m dashes. She felt it likely she would make it to the state competition. Following subsectionals, she would have another week to recover.
At this second visit she had 4+/5 strength for left knee (quadriceps) extension. There were still painful and palpable trigger points in the vastus lateralis and rectus femoris. Myofascial restrictions were also noted through the quadriceps group while using IASTM. When performing a 6" step down and a 1-legged squat on the left leg, we noticed that she had medial translation of her left knee, indicating left gluteal weakness. Treatment at this visit consisted of interferential stimulation current over the left quadriceps group while she performed 6" step downs (2 sets of 10 reps) on each leg followed by single-leg squats into a chair (3 sets of 10 reps) performed bilaterally. IASTM was then done for 3 minutes over the entire distribution of the left quadriceps group as well as the distal psoas tendon while she lay supine. Again, manual muscle release of the vastus lateralis and rectus femoris was performed, over the time the patient engaged in active knee flexion while the doctor held the contact locations. Rock Tape™ was applied over the length of the quadriceps muscle. She was again told not to participate in any athletic activities, nor run or jog, until her next appointment. 6" step downs (3 sets of 10 reps) and 1-legged squats into a chair (3 sets of 10 reps) was added to her HEP.
The patient returned the next day for treatment. Subjective complaints only included soreness to touch. At the very worst, her pain had only reached 3/10 while at best it was 0/10. She indicated that her quadriceps felt fatigued and “over-worked.” She had been faithful with her HEP.
Her quadriceps strength was a 5/5 and hip flexion was also 5-/5. There was still pain and trigger points noted on palpation, along with myofascial restrictions through the quadriceps. Treatment now consisted of interferential stimulation current over her left quadriceps group while performing 6" step downs (2 sets of 10 reps) on each leg followed by 1-legged squats into a chair (3 sets of 10 reps) performed bilaterally. IASTM treatment shifted away from passive treatment to a more dynamic intervention. IASTM was performed over the quadriceps group while she performed 10 reps of body weight squats, butt kicks, high knee marching steps, lunges, and 1-legged squats into a chair. Following this, 2 more sets were repeated without IASTM treatment. Rock Tape™ was applied over the length of the quadriceps muscle. The HEP remained the same; however the patient was given a blue Theraband™ to increase resistance. She was told she could return to athletic participation. The first day of participation should include 25% of her max intensity Should she not suffer any setback, she could move to 50% the following day, and 75% the next day. If she did have a set-back, she was to remain at 25% max intensity until her next follow-up appointment in 3 days.
Three days later, she returned for care. She noted her quadriceps was feeling “pretty good, a little bit sore.” Her exercise progressions increased 25% each day without set-back. Two days prior, she did a 400m run at 50% max intensity and noted soreness the first 50m but then felt fine. The previous day she ran 2 100m sprints at 75% max intensity with the pain getting up to a 3/10 at worst. She had no pain while walking or using stairs. She noticed minimal pain when trying to lunge.
Her quadriceps strength was 5/5 on the left while hip flexion was 5-/5. Pain and trigger points were found inthe rectus femoris and vastus lateralis; however, this was improved from the last visit. Myofascial restrictions were felt through her left quadriceps while performing IASTM. Treatment included interferential stimulation current to the left quadriceps group during 6" step downs (2 sets of 10 reps) on each leg followed by single-leg squats into a chair (3 sets of 10 reps) performed bilaterally. Next, compression floss was wrapped around her left thigh at 50% stretch. She then performed 3 sets of 10 reps of body-weight squats with green Theraband™ around her knees, buttock kicks, high-knee marching steps, 10 lunges bilaterally, and single-leg squats bilaterally. Her HEP program remained the same; however, she began to include compression floss wrapped around her left thigh at 50% stretch. Athletic restrictions included 90% max intensity the next 2 days of practice. She was told to follow-up in 2 days with the follow-up day being treatment only and absolutely no physical activity. She was told to use that day as a day of rest, as the following day was subsectionals. Rock Tape™ was applied over the length of her quadriceps muscle.
In 2 days, returned to the office. She performed her track and field activities at 90% max intensity and was seeking treatment on her rest day. She only noted soreness upon stretch in her left quadriceps. Muscle strength remained 5/5. There was still pain and trigger points in her rectus femoris and vastus lateralis; however, this had improved. Myofascial restrictions were felt through her left quadriceps while using IASTM. Treatment included passive IASTM to the quadriceps muscle group with her laying supine. Dry needling with electric stimulation was also provided for 20 minutes in the left quadriceps muscle. Rock Tape™ was applied over the length of the quadriceps muscle and she was told to participate fully in tomorrow’s meet event. Instructions for the meet included performing her HEP at 1 set of 10 reps with the compression floss 30 min prior to each event. Following the meet, she was told to rest for a day and then ramp back up on a 25% max intensity interval level each day following. She scheduled a follow up for 1 week later.
At that next visit, she let us know she took 1st place in all of her events: 100m, 200m, and 400m sprint with personal records in the 100m and 200m. She noticed minimal pain the day of those races, 1/10 at worst while competing, with some residual soreness for 2 days after the event. After the soreness went away, she had no pain and indicated her pain was absent at this treatment. She was reporting for treatment on a rest day with her meet the following day. Examination revealed muscle strength remaining at 5/5. There was minimal pain and tenderness on palpation of the quadriceps group and minimal trigger points. Because this a rest day, treatment applied was passive and included IASTM to the quadriceps muscle group with her laying supine. Dry needling with electric stimulation was also provided for 20 minutes in the left quadriceps muscle. Rock Tape™ was applied over the length of the quadriceps muscle and she was told to participate fully in tomorrow’s event.
Following sectionals, she again had a week to prepare for state competition. She was released to an as-needed basis and told to seek treatment only if she felt she needed another treatment or if she had a set-back. She was to continue using her compression floss daily with her HEP. Instructions for her section meet included performing her HEP at 1 set 10 reps with the compression floss 30 min prior to each event.
She did not return for care after her section meet as she indicated she was pain free. She also informed us that she set new records at the section meet in all 3 of her events. One week after completing her section finals, she participated in the state competition. She placed in all 3 events and again set personal records in the 100m and 400m sprint.
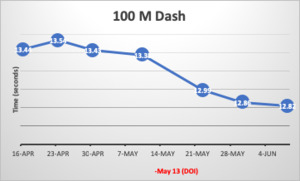
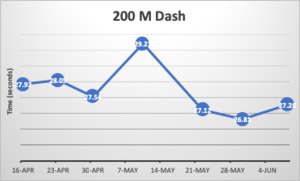
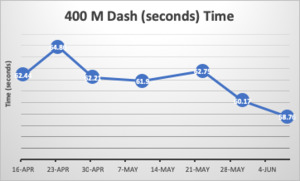
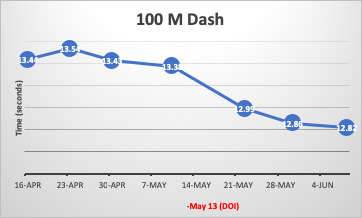
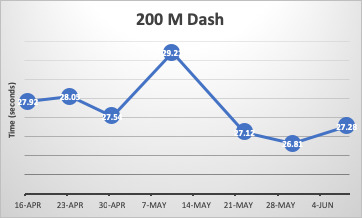
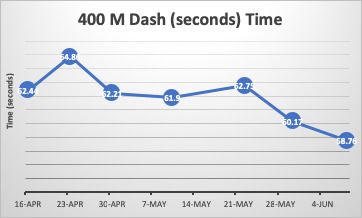
The figures below display her time (in seconds) for her events. The vertical red line is the day of injury. She had 6 treatments from May 15-29. Her last treatment was the day before her sectional meet and following her section meet she had no further care through her state competition, as she felt that she had not only returned to her normal but improved from her baseline scores. Her times clearly improved following multimodal chiropractic intervention, even post-injury.
DISCUSSION
For track and field athletes, especially sprinters, musculotendinous strains may hinder future performance and limit participation in practice and events. Female athletes, compared to men, have a greater risk of suffering a quadriceps strain and recurrence of injury in all sex-comparable sports.1–4,8 In addition, quadriceps strains in track and field athletes average a participation-restriction time of <7 days, with return to activity continuing to be limited.1,9 Our report demonstrates the use of multimodal chiropractic care, including active and passive-based interventions, during a return to participation in a female, high-school track athlete.
Per the Italian Society of Muscles, Ligaments and Tendons, clinical indication for a diagnosis of a muscular strain emphasizes the importance of an in-depth history and clinical examination.10 The following criteria for musculotendinous strain that were met, as per patient history and exam, were sharp pain evoked by a specific movement, well localized pain, easily appreciable upon palpation, and preceded by a snap sensation. No diagnostic imaging was used as we did not believe it was clinically necessary nor would have changed our treatment methods.
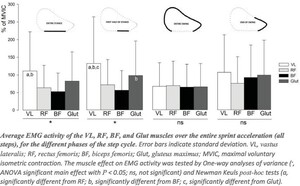
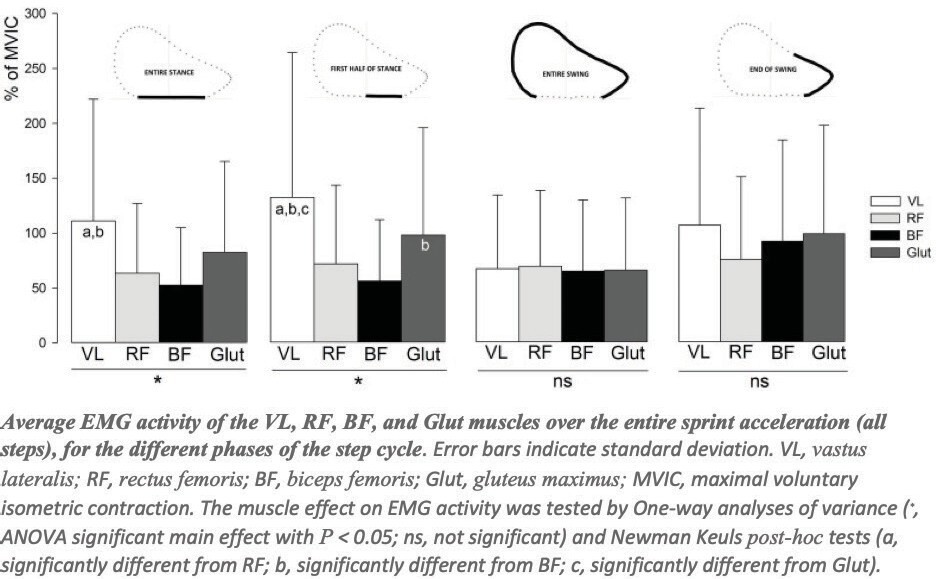
Due to the prevalence of recurring injury in women who suffer a muscular strain, our active treatment was aimed at increasing muscular strength of the quadriceps to help reduce the risk of reinjury while increasing performance.11–13 A functional movement examination including a 2-legged squat, single-leg squat, and 6-inch step down indicated slight left gluteal weakness compared to the right. During the 6-inch step down and 1-legged squat on the left leg, knee valgus collapse was more pronounced. As evident in Figure 4, created by Morin, Gimenez, Edouard et al, EMG activity of the gluteal muscles is greatest during the end of the swing phase, with the rectus femoris EMG activity also highest during the end of the swing phase.13 The quadriceps are also the greatest contributors to the support phase and when braking. As mentioned earlier, most quadriceps strains are sustained during rapid eccentric contraction; therefore, a decrease in quadriceps strength and an increase in tendon stiffness may result in excessive eccentric tension through the elongated rectus femoris. Inability to properly distribute forces, muscular activity, and rapid, excessive forces in an elongated state may provide insight why addressing muscular strength of our patient’s left quadriceps and gluteal muscles was important for optimal recovery and increased performance post-injury. Research on sprint performance provides evidence a hip flexor strengthening program can help with increasing hip flexor strength and improving sprint performance.12
Most of the treatment included manual therapy and instrument-assisted soft tissue mobilization (IASTM). Manual therapy and IASTM are common treatments for musculoskeletal conditions and have been widely studied, although research is conflicting. The purpose of using IASTM here was to attempt to desensitize injured tissue, mitigate pain, increase range of motion, and promote healing of the strained musculature. (15-18) As stated earlier, there are contradictory results regarding the use of IASTM to promote increase in range of motion and decrease pain; however, some studies have shown that IASTM can produce acute increases in range of motion.14,15 Although acute, the potential for an increase range of motion is beneficial to help the patient perform the recommended rehabilitative exercises efficiently and through a greater range of motion during the treatments. In this case, performing IASTM to help increase hip flexion and extension was crucial to ensure pre-injury range of motion was returned. The IASTM protocol used incorporated IASTM with active movement of the hip through flexion and extension while explaining the proposed mechanisms of the treatment. The explanation provided to the patient was that IASTM has been studied to improve tissue extensibility, activate mechanoreceptors within the area stimulating a neurophysiological effect, decrease patient apprehension, and decrease inflammation. (15-18) Finally, recent work provides evidence for the use of IASTM to enhance lower extremity muscular strength in individuals with lower extremity musculoskeletal injuries. (19) This may provide insight as to the increased performance of the patient post- injury, however, the research is conflicting as another study found IASTM to the lower extremity in non-injured subjects did not produce a change in muscular strength or power output. (20)
In addition to the active rehabilitation and manual therapy, psychosocial factors of the athlete should be considered. As she progressed with care, it was crucial to address her concerns about whether she would be able to compete in her upcoming events. We discussed that the importance of adherence to her rehabilitation program would provide a greater chance at her having positive outcomes with care, as athlete adherence to rehabilitation programs has been shown to demonstrate better outcomes. (21,22) Her internal goal of competing and external motivation from family and supporting members to participate in her final high-school track events may have also played a crucial role in her care. Goal setting and social support following injury has been shown to improve outcomes of rehabilitation programs. (22) Furthermore, progression using graded exposure to return to sport was provided to introduce load and assess psychological readiness to compete. Graded exposure and psychological readiness to compete are important for athletes as it allows the clinician and athlete to assess where the athlete stands regarding confidence to fully participate, confidence in the injured body part, and overall confidence of the athlete. (23)
Following care, she set personal bests in the 100M, 200M and 400M sprints 7 and 14 days after initial injury. Finally, she did not suffer a re-injury or aggravation of previous strain while competing in 3 different competitions spread throughout 2 months post-injury.
Limitations
One limitation of this study is its single-subject design. It represents anecdotal evidence that may lack important comparative analysis and statistical evaluation. Considering the amount of time lost on quadriceps strains annually by athletes, more research and clinical education is needed regarding proper treatment and evidence-based therapeutic regimens of these treatable injuries. Furthermore, further literature should also focus on prevention.
CONCLUSION
This case discusses multimodal chiropractic intervention of a grade 2 quadriceps strain involving a female high- school athlete. The treatment provided allowed her to not only adequately recover from the injury but also set personal records in her 3 events following care. It illustrates not only the importance of treating the specific injury, but also treating global mechanic dysfunction.