Introduction
Sport-related concussions (SRC) are a significant health concern currently at the forefront of public health awareness1 Over the past 10-15 years, increasing numbers of youth and adolescents have visited emergency departments or their primary-care provider with concussion-like symptoms.2 Most patients experience an improvement in symptoms regardless of seeking treatment; however, a medical assessment, specific rehabilitation plan and a guided process towards recovery is preferred.3 The majority of pediatric concussion patients will return to sport and school activities within 1-4 weeks.3 Those who sustain head trauma and do not have timely access to proper medical care are at small risk of sustaining another concussion or more severe forms of traumatic brain injury (TBI) or other neurological conditions that may be unrecognized.4 They are also at risk for premature return to sport and/or school, prolonging recovery.
Although most pediatric concussions can be managed by their primary-care provider, some patients have persistent symptoms requiring referral to specialists in concussion management.5 Unfortunately, timely access to specialized healthcare is not always readily available, especially for those living in rural or remote communities with significant geographic, socio-economic or cultural barriers to these services.6–8
Despite a variety of educational attempts delivered worldwide concerning concussion recognition and management, SRCs are often unrecognized. Educating athletes, parents, coaches, trainers and other sport-related personnel regarding appropriate screening and management of concussion is essential to idenitifying unrecognized concussions.9 Concussion education programs help improve concussion detection and adherence to management strategies; however, these educational efforts must be regularly reinforced.9 There is no uniform educational program to disseminate information to student athletes about concussion.10
Managing athletes with head injuries requires specific clinical decision making, adherence to already established protocols, and the knowledge and ability to make referrals for an integrated care approach.11 In an ideal setting, all sustained SRC’s would result in immediate removal from play followed by an additional sideline assessment when the concussion injury is witnessed. Immediate continued play after a sustained SRC can worsen symptoms.12 However, this may not always the case, as in the cases we describe here.
This paper describes a case of a 10-year-old girl with a sport-related concussion who was diagnosed and clinically managed by chiropractors. Her case involved a situation where she was playing basketball and unknowingly sustained a concussion, which was then misdiagnosed until she saw a chiropractor days after the concussion. This paper discusses the examination, diagnosis and appropriate management of concussion as per current guidelines.
CASE REPORT
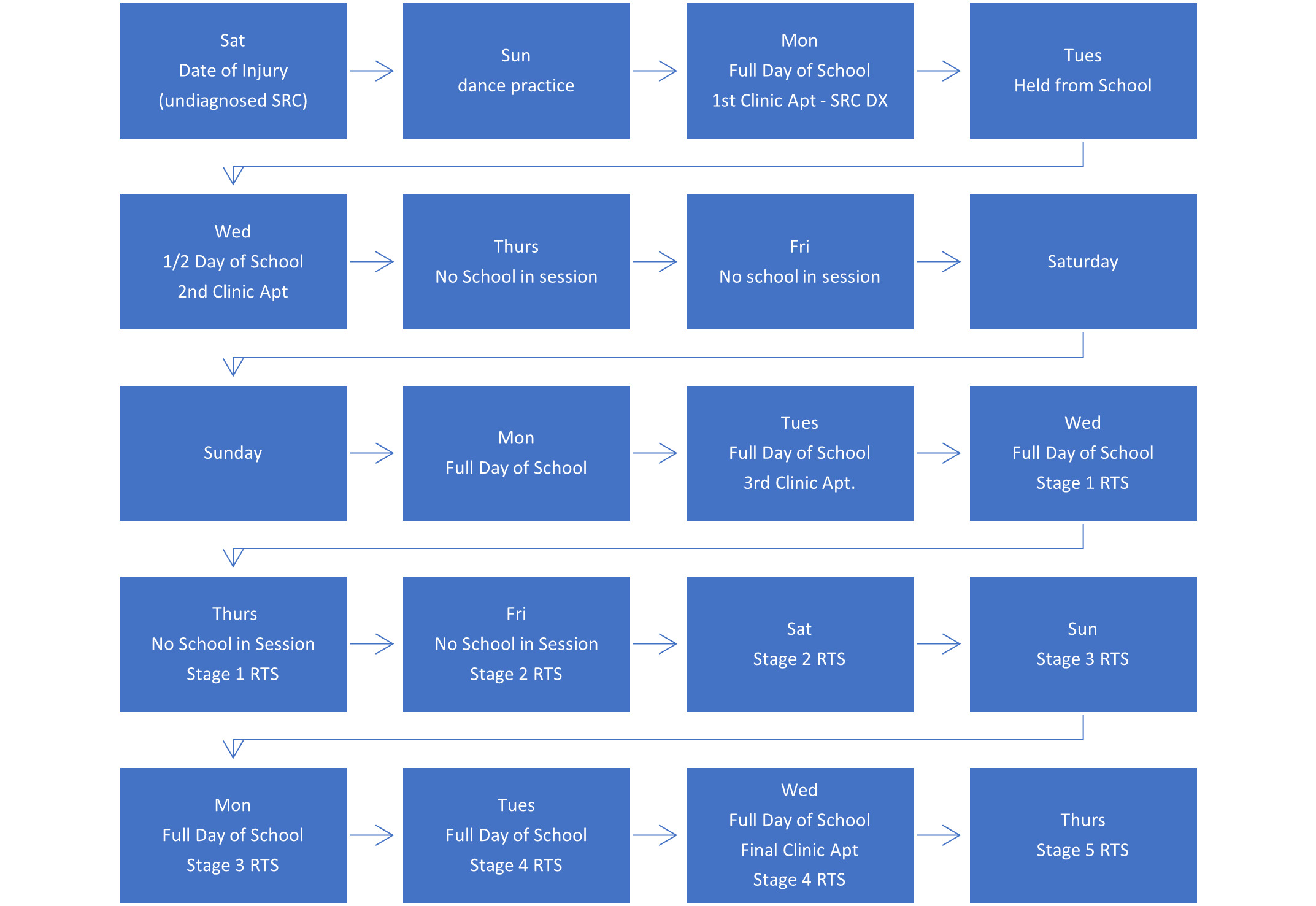
A 10-year-old basketball player sustained an acute SRC during her second basketball game of the day. During the game, she collided with another player and fell backwards, hitting her head on the floor. This injury was not seen by the coach, her parents or any other authority, and she continued to play. The following day, she practiced her dance routine after school, then proceeded to attend school the next day. She visited a chiropractic clinic 2 days later, complaining of neck pain, headache, mid-back pain, and low back pain, clearly and understandably unaware that she may have sustained a concussion.
She had not experienced loss of consciousness (LOC) or amnesia. She did report dizziness and visual disturbances that she described looking like “static on a television.” These symptoms lasted for a short time after the fall, quickly resolved, and she continued play. After the game ended, she noticed neck pain, suboccipital headache, mid-back pain and low back pain. Her neck pain and headache were both rated a 10/10 on the Numerical Rating Scale (NRS). She had no radiculitis into her upper extremities. The day after her head injury injury, while practicing her dance routine, she experienced 5 minutes of dizziness and visual disturbances. While attending school, she had a general lack of focus and felt as though she was unable to complete math equations that she would have otherwise been able to complete. She also experienced some generalized dizziness and reported a return of the visual disturbances while engaging in those math problems. Her mid-back and low back pain, felt achy and she rated each to be a 4/10 on the NRS. There was no lower extremity radiculitis or alterations in bladder or bowel function.
The Child SCAT 5 was performed. Her initial symptom score was 46/63. Immediate memory was a 13/15, concentration was 3/6, 7 errors were recorded during the balance exam, and 4/5 for the delayed recall. Romberg’s test was negative with eyes open and closed; however, during the 20-second eyes closed single-leg stance she had 5 errors, with 2 errors during the 20-second eyes closed tandem stance. Finger-to-nose test was performed inadequately and accommodation revealed involuntary right lateral deviation during convergence of her right eye. Cardinal fields of gaze produced asymmetrical and jerky pursuit eye movements. Light reflex test was normal when the light was shined in the left eye, but created discomfort and delayed pupil constriction in the left eye after shining the light into the right eye. Neurologically, she had 4/5 strength for C5 on the right with normal deep tendon reflexes at all levels. Cervical active range of motion revealed limited flexion, extension, bilateral lateral flexion and rotation; all movements reproduced her neck pain. Foraminal compression and shoulder depression tests reproduced her localized neck pain but did not cause any upper extremity radiculitis. Tenderness to palpation and hypertonicity were present, bilaterally, within the cervical paraspinal muscles, as well as in many other neck muscles, and at the vertebral levels associated with the cervicothoracic junction, mid-thoracic region and lower back.
We informed the child and her mother that she had sustained a concussion. Concussion education was provided and the return-to-sport and return-to-school process was implemented. Due to the severity of symptoms, her care included a course of chiropractic multimodal intervention.
Initial treatment consisted of cervical spinal manipulation, myofascial release, and instrument-assisted soft-tissue mobilization. Her initial home exercise program (HEP) included working on single leg stance with her eyes closed and going for a few 15-minute walks. We advised her and her mom to limit her screen time to a total of 45 minutes per day and to watch in 15-minute increments. She stayed home from school the following day and was told to return for only half days for the following 2 days. She was restricted from all sporting activities and physical education class until she could start Stage 1 of the return-to sport guidelines as outlined in the Consensus Statement on Concussion in Sport.13
Two days following her initial examination, we did a follow-up exam. She stated her neck pain was worse than when she initially came into the office, rating her pain a 10/10 on the NRS. On the morning of this appointment, she felt a sharp pain within her right inner ear along with continued tinnitus in the same ear. Fifteen minutes before the appointment she experienced dizziness along with peripheral visual disturbances after pushing a shopping cart around a grocery store. She also participated in her school’s talent show the day before this visit and sang 2 songs. After singing the second song she had a headache and noticed difficulty concentrating during her math class the next day. By the time of this visit, her low back pain had resolved; however, her mid-back pain remained. We manipulated her cervicothoracic junction and mid-thoracic spine. Myofascial release and instrument-assisted soft-tissue mobilization were both used in the same regions. The exercises added during this visit included Figure 8 walks, visual acuity every hour, eye infinity every hour, and single leg stance eyes open and closed. She was cleared to go back to school when it reopened 5 days later.
Her third visit was 6 days later. She now had less neck and mid-back pain. She played tag at recess the day of her visit and did not experience any dizziness or have any headaches. However, she was still having trouble at school completing math problems. Treatment included spinal manipulation and manual therapy where indicated. Exercises added to the HEP included eyes-closed single-leg balance on a TherabandTM balance pad for 20 seconds 3 times, an exercise circuit consisting of 10 lunges each leg, 10 squats, and 10 modified push-ups 3 times, and a Vestibular Ocular Reflex (VOR) exercise. She was told to progress through the stages herself and given the dates in which to follow, but that she had to go 24 hours symptom free at each stage.
Her fourth visit was 8 days later, where she reported mild neck pain without experiencing any dizziness or headache. The Child SCAT 5 symptom score continued to decrease, to 3/63 with continued improvement overall. The IMPACT test was administered and revealed insignificant findings. She had full active pain-free cervical ROM. Spinal manipulation and manual therapy were performed. She was advised to progress to Stage 4 that night at practice, and if she was symptom free, she could progress to Stage 5, which gave her full clearance to play in her basketball game the next night. Figure 1 provides the full time-line for this case.
Discussion
Concussions are 1 of the many types of injuries that may be seen in a chiropractic office. It is important chiropractors take the time to learn more about concussion and its management. New information regarding management occurs daily.
This repoprt demonstrates several key issues: the importance of concussion recognition, the importance of a proper management plan and, finally, that chiropractic manipulative therapy may be beneficial in the recovery process. A proper management plan will differ based on the patient’s presenting symptoms and age, as there is no gold standard for a specific time frame for full resolution of symptoms.13 Here, we initially withheld the child from school and sport, and gave her limitations that included decreased screen-time. She was told to begin working on her balance and to go on 15-minute walks, but to stop if she began to experience any of symptoms. Every appointment following the initial visit consisted of evaluating what her symptoms were and how she was responding to the prescribed exercises. From there, the progression of exercises and back-to-school and sport limitations could be made.
Concussion recognition is the first and most important step in the management of an SRC. For a healthcare provider, the first suspicion that a player has sustained an SRC is when the patient reports a blow to the head or neck during play. In our case, nobody saw the incident happen. Therefore, the recognition was left to our patient. Of course, at 10-years-old, she was not educated on the importance of linking the symptoms she was experiencing to falling and hitting her head on the gym floor. An unrecognized concussion is serious because it leads to the possibility of second impact syndrome. Although this is rare, this occurs when a player sustains a second concussion before the original concussion has resolved.14 Recurrent concussions typically add to the time it takes for symptoms to resolve and even increase the likelihood of loss of consciousness during the second SRC.15 Additionally, pediatric patients are at higher risk for SRC’s because of their developing neurological, vascular, and musculoskeletal systems.15 This is why it is essential to recognize and evaluate a concussion immediately following the injury, especially in pediatric patients. Another part of recognizing a concussion is identifying the signs and symptoms of a current concussion. Common symptoms of SRC’s in youth athletes are headache, dizziness, concentration difficulties and confusion, with high rates of accommodative, convergence and saccadic dysfunction.16 Our pediatric patient experienced most of these; however, she came to our office 2 days following the concussion, so management was quick and successful.
Once an SRC has been diagnosed, follow the most recent management protocols to provide a safe and quick recovery for the patient. Ideally, an initial evaluation would be performed on the sideline immediately after the concussion occurred. If there is a lack of available healthcare, an initial evaluation should take place in-office as soon as possible. The initial assessment for a pediatric patient should include a complete and thorough history prior to conducting the Child SCAT-5 and physical examination. The physical exam should include a head and neck exam and neurological, ocular, and balance tests. Typically, further diagnostic imaging is not required for the diagnosis of an SRC unless there is a suspected fracture or intracranial hemorrhage.16
Once an SRC has been diagnosed, the back-to-school and back-to-sport protocols can be put into place. Recommendations are to suggest 24-48 hours of rest with restrictions of activities of daily living that provike symptoms.15 Light aerobic exercise that does not aggravate symptoms after the 24-48-hour rest period may help in quicker progression of the patient.15 A gradual return-to-school should include limiting daily activities at home that are symptom provoking and slowly building up the time allowed to do these activities.15 As symptoms are being tracked, the patient can progress to doing school activities at home, half days at school, and then finally back to full days with certain restrictions as needed. As the progress through return-to-school is being monitored, the patient should have a progression of ongoing rehabilitation exercises helping to improve the patient’s aerobic capacity that stays below symptom threshold, as well as balance and cognitive exercises as deemed fit.15 On top of rehabilitation, the athlete’s return-to-sport protocol should also be taking place and should include a progression that includes rest, light aerobic exercise, sport-specific exercise, non-contact training drills, full contact practice, then finally return to play. There should be at least 24-48 hours of staying sub-symptom threshold before the patient can move onto the next stage to avoid any regression during management.15
Until the emergence of recent literature, the primary treatment following SRC’s included education, physical and cognitive rest, neurocognitive rehabilitation, and in some cases antidepressants. However, those forms of treatment had shown little effectiveness for Post-Concussion Syndrome.17 More recent studies have started looking at multimodal treatment options including but not limited to cervical manipulation for spinal dysfunction, vestibular rehabilitation, visual training, cardiovascular exercise, and more. Post-concussion symptoms may be associated with cervical spine and/or vestibular dysfunction.18,19
CONCLUSION
This is a single case report, and cannot be generalized; however, this also reports diagnostic considerations that can. To further gauge the effectiveness of care, further studies need to be completed. Most athletes with SRC will recover within 21-28 days, with the greatest recovery in the first 2 weeks. Neurocognitive impairment tends to linger across various domains up to 28 days following SRC.20 This case is no exception to that, which may suggest that the athlete did not benefit from chiropractic compared to natural progression of SRC. More research is required to determine the overall effectiveness of chiropractic intervention related to SRC.