INTRODUCTION
Beyond the average mortality rate of 0.012%,1 an estimated 10-30% of individuals who contract coronavirus disease (COVID-19) experience mild to severe protracted or new symptoms that persist for greater than four weeks after the initial infection.2 This post-viral phenomenon has been referred to by several names; one common designation is long-COVID. While symptoms of long-COVID vary by individual, common symptoms include fatigue, cognitive impairment, muscle or joint pain, and breathing difficulties.2–5
The array of symptoms and presentations in long-COVID make the search for an effective therapeutic intervention a challenge. Symptom-targeted therapies such as personalized rehabilitation programs and pharmacotherapy have met with some success, off-label pharmaceutical use to attenuate symptoms in long-COVID sufferers has been recommended (with caution) by several reviews and organizational guidelines.6–10 For example, anti-inflammatory agents like non-steroidal anti-inflammatory drugs (NSAIDS) and corticosteroids have been suggested for inflammatory related symptoms.6,8–13 Off-label use of a medication should only be prescribed after the medical doctor discusses risks and side effects with the patient.14 To date, no specific pharmaceutical has been approved for the treatment of long-COVID.
While therapeutic interventions for long-COVID continue to evolve, research on possible treatments may ultimately be advanced by focusing on the mechanisms of action related to its development. Proposed mechanisms include the presence of viral remnants (viral reservoir) within the body, autoimmune responses, and dysautonomia, among others.2 Dysautonomia in particular can be easily assessed in a clinical environment, as it does not require advanced staining technology, blood work, or expensive post capture analysis.15–18 While the use of surrogates of physiologic function can be challenging, dysautonomia can be measured using a 3-lead electrocardiogram (ECG) to evaluate heart rate variability (HRV).18 HRV, a measure of the variation between interbeat intervals of the heart, is a low-cost assessment tool that could be used to expand the clinical study of long-COVID beyond conventional clinical and medical research.15–21 This is crucial when patients are seeking alternative approaches to improve their health, and yet to date there has been limited research undertaken in Europe and North America to evaluate different complementary and integrative medicine approaches to the pandemic.22–25
According to a 2012 national survey, roughly 33% of Americans used healthcare approaches beyond conventional medicine approaches.26,27 Understanding the role of complementary and integrative medicine (CIM) in overall health and as an intervention for both COVID-19 disease and long-COVID could be of importance to global public health initiatives.22–24 CIM represents a broad spectrum of healthcare modalities and practitioners.27–29 This cohort of practitioners may be able to help with current pandemic research by providing (1) an expanded perspective of a patient base that may or may not present to conventional medical offices, (2) a potential therapeutic course of care, and (3) greater understanding of the mechanisms of action associated with long-COVID.
To meet the above objectives, it is important to first establish a methodology that can be integrated into CIM practices. The present study was conducted using the manual therapy intervention of chiropractic care. While not conclusive, manual therapy has been shown to induce changes in blood pressure, HRV, heart rate, and neuroimmune chemical concentrations.30–38 Chiropractic care in the United States is used by roughly 8.4% of the population, and 53% of those patients seek manual therapy interventions like chiropractic care to improve their overall well-being.27,29,39 However, the challenge of integrating clinical research into the practice setting is frequently a limiting factor to increased CIM research production. The purpose of the present study was to prototype a long-COVID study within a practice-based setting, testing procedural steps, outcome measures, and patient response to care.
METHODS
Overview of Study Design
This study was a single-group exploratory study conducted to prototype study procedures, outcome measures, and patient response to 8 to 12 weeks of chiropractic care. The study was integrated into a busy chiropractic clinic. A study support team within the clinic was established and included 3 chiropractors practicing the Axial Stability Method (ASM) chiropractic technique, administrative support staff for scheduling and phone screening, and a study coordinator who also assisted in data collection. The study was approved by the Life University Institutional Review Board, and each study participant was advised of their rights as a participant and signed an informed consent document prior to study participation.
Study Population
Participants between the ages of 25 to 65 were recruited through healthcare referrals, social media, and emails to existing patients of the participating chiropractor. The initial aim was to recruit 20 individuals for the study. Participants could be included in the study if they tested positive for COVID-19 viral infection or presented with SARS-CoV-2 antibodies greater than 90 days prior to qualifying for the study. In addition, participants had to have presented with at least two long-COVID symptoms (Table 1), which could not be explained by an alternative diagnosis.
Participants were excluded from participation in the study if they were participating in any other COVID-19 related clinical trial or taking medications specifically prescribed to counter the effects of the COVID-19 virus. The exclusion did not include over-the-counter or prescribed medication to counter specific COVID-19 symptoms such as cough, body aches, or sleep disturbances. Since the individuals were receiving chiropractic care, participants were also excluded if they had any contraindications to chiropractic care, such as surgery or a fracture to the skull or spine within the past 6 months. Additional exclusionary criteria were:
-
Pregnancy: currently or planning to become pregnant during study timeline
-
Legal: pending health-related legal litigation
-
Health practices: history of cigarette, e-cigarette, or vape use within the past 5 years or more than 3 alcoholic beverages per day
-
Non-COVID related chronic disease process: history of malignant cancer not in remission for the past 5 years (excluding squamous or basal cell carcinoma) or present multi-system disease (e.g. Paget’s or Lyme disease)
-
Mental health: evidence or medical history of clinically significant, uncontrolled psychiatric diseases (e.g. schizophrenia or schizoaffective disorder)
Study Protocol
On-site clinicians, support team, and investigators worked in collaboration with university investigators to develop a study protocol that could reasonably be integrated into the existing chiropractic practice setting. Initial eligibility was determined through phone screening; secondary screening was determined by review of pre-exam paperwork, health history, and physical exam. Per normal and customary care, if a participant presented with pain during the physical exam, they were asked to complete the Oswestry Disability Index40 for low back pain, Headache Disability Index,41 or the Neck Disability Index42 based on location of pain. Immediately following the physical exam, those participants meeting final eligibility requirements received their initial baseline assessments. The ASM model of chiropractic care incorporates 3 distinct phases of care, so follow-up assessments were conducted at completion of each phase of care. This resulted in four assessment time points. Each assessment time point consisted of the following participant self-reports and assessments, with the exception of 1 fatigue survey that was administered weekly.
Participant self-reports: Long-COVID is a complex condition with a heterogenous mix of symptoms.2–5 Self-reported surveys were implemented to capture response to care across the spectrum of symptoms.
-
Functional Assessment of Chronic Illness Therapy–Fatigue Scale (FACIT-Fatigue)43,44: The FACIT-Fatigue (PROMIS Item Bank v1.0-Fatigue-Short Form 13a) is a 13-item measure that assesses self-reported fatigue and its impact upon daily activities and function (facit.org). This 5-point Likert-type scale–ranging from “0” (not at all) to “5” (very much)–was administered to participants weekly, and as long as assessment occurred on the same day of the week, participants had the choice of taking the survey through email, text, or in-person.
-
Multidimensional Fatigue Symptom Inventory- Short Form (MFSI-SF)45: The MFSI-SF–consisting of 5 subscales (vigor, general, physical, emotional, and mental–was administered at baseline and each follow up assessment time point. The MFSI-SF consists of 30 items assessing the feeling of fatigue over the past 7 days and includes). Participants rate each item on a scale of “0” (not at all) to “4” (extremely).
-
Study-specific COVID-19 disease and long-COVID surveys: To gain a better understanding of the participants’ overall symptom experience with COVID-19 disease and long-COVID, 2 study-specific symptom surveys were created. One survey asked about the participants’ remembered experience during active COVID-19 disease. A second survey asked about participants’ present long-COVID symptoms using a 7-day recall (Table 2). For both surveys the participants were asked to report on the presence, number of days, number of hours per day, and intensity of each symptom. Participants were asked to rate their symptom intensity from “0” (no symptom) to “10” (worst intensity). The survey evolved from multiple sources, including Centers for Disease Control and Prevention Human Resources and reports such as the COVID-19 “long hauler” symptoms survey report.3,46,47
-
RAND 36-Item Health Survey (SF-36): Patients with long-COVID often experience diminished self-reported quality of life (QoL.25,48 To assess changes in QoL, participants were asked to complete the SF-36 (version 1.0) at each assessment time point. The SF-36, a validated short-form survey developed from the Medical Outcomes Survey, assesses 8 distinct health concepts: physical functioning, bodily pain, role limitations due to physical health problems, role limitations due to personal or emotional problems, emotional well-being, social functioning, energy/fatigue, and general health perceptions.49–52
-
Post-Study Survey: Finally, since this study was designed to prototype study methodology, participants received an anonymous post-study survey. The survey asked several questions about their experience in the study, including questions regarding the process, staff, and referral.
CareTaker Medical physiologic recordings: Using the CareTaker Medical system (CareTaker Medical NA, Charlottesville, Virginia), participants were setup with a wrist monitor, finger-based blood pressure cuff, Vivalink chest ECG sensor (Vivalink, Campbell, California), and pulse oximeter. (Figure 1) Devices were connected via Bluetooth to a Samsung Galaxy Tab A8 (Samsung Electronics, Suwon-si, South Korea) running the CareTaker Medical Software versions 1.6 to 2.0.35 (CareTaker Medical NA, Charlottesville, Virginia). The sampling rate was 128 Hertz.
Recordings were performed for 7 minutes in the supine position, with the individual instructed to breathe normally. At each assessment time point, recordings were conducted before and after the chiropractic care intervention. Approximately 3 minutes of rest time was provided prior to the post-chiropractic assessment to simulate the additional time required for ECG setup and equipment preparation. Participants were asked to keep exercise, sleep, medication, and caffeine consumption consistent at each assessment time point.
Spirometry: Spirometry was performed utilizing a handheld spirometer and LabQuest Viewer software (Vernier, Beaverton, OR). Participants were instructed to wear a nose clip or hold their nose shut with their fingers, sit up straight, and place their mouth on the mouthpiece of the spirometer. Then, they were asked to breathe in and out normally once, take a deep and forceful breath in, and then forcefully and fully exhale as quickly as possible. This was repeated three times for each assessment session.
Balance: The Fukuda stepping test is considered an indicator of dynamic balance.53–56 Participants stood in the middle of a room with their eyes closed and arms outstretched in front of them and were asked to march in place for 50 steps. If fatigued, they were allowed to stop. To ensure the safety of the participant, an investigator monitored them while they were marching.
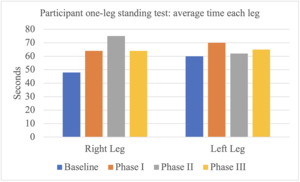
The 1-leg standing test for assessment of postural and balance control has been shown to be sensitive to clinical change.57,58 At each assessment time-point the participants were asked to stand self-supported with eyes open, palms resting on their hips, and one leg raised off the floor. They were allowed to self-select the starting leg, then repeat the test with the other leg. For safety, an investigator stood next to the participants to monitor and assist if they became unstable. The test and recording were stopped when the participant placed the non-supported leg on the floor for stabilization or when two minutes had elapsed on the timer.
Chiropractic care: Chiropractic care was provided using the Axial Stability Method (ASM) chiropractic care protocol, with 1 or 2 visits scheduled each week for up to 12 weeks.59 Axial Stability Method (ASM) is a precise, gentle, low-force chiropractic technique practiced since the 1970s. The technique, originally a spin-off of Sacro-Occipital Technique (SOT), the work of Dr. Major B. DeJarnette,59 has since evolved into a comprehensive stand-alone technique. The ASM technique focuses care on regions of the body exhibiting instability–especially the pelvic structural system–and includes three standard phases of care for the neuromusculoskeletal system:
-
Phase 1. Stabilizing the Triad of Equilibrium: stabilization of the occiput and first cervical vertebra (O/C1) using an ActivatorTM instrument (Activator Methods International, Ltd., Phoenix, Arizona) to adjust the segments after stimulation of the visual and vestibular systems;
-
Phase 2. Sacro-iliac (SI) Structural Foundation: stabilization of the SI joints using SOT wedges;
-
Phase 3. Muscle Balancing: whole body ActivatorTM instrument adjusting of the muscles of counternutation and nutation in supine, then sitting, then standing positions.
Based on the lead clinician’s experience with long-COVID sufferers, Phase 1 of care also included an acupressure protocol and Viscero-Somatic Reflex Patterns (VSRP) protocol, theorized to rebalance the autonomic nervous system.60,61 Drawing upon reflex points often employed by early osteopathic physicians and traditional Chinese medicine practitioners, the ASM acupressure and VSRP protocols use a series of muscle tests with the participant in the supine position; correction involves the use of an Activator instrument excursion to the spine and/or therapeutic pressure applied to specific areas of the body.60,62
Data Processing
Since this study was a single-group prototype development study with a small sample size, no statistical analyses were performed. Data were represented as averages and/or individual participant reports.
Survey instruments: For the FACIT-Fatigue, the T-scores were calculated using the Health Measures Scoring Service (healthmeasures.net) with calibration set at default PROMIS Wave 1. The MFSI-SF processing consisted of questions representing each of the 5 subscales that were individually summed to produce the subscale value, and the total score was calculated by summing scores for all subscales except vigor, which was subtracted.63,64 Similar to the MFSI-SF, the SF-36 instrument included questions that related to specific domains of health, and scoring of each health domain was performed using the recommended scoring rules for the RAND 36-item health survey, version 1.0 at https://www.rand.org/health-care/surveys_tools/mos/36-item-short-form/scoring.html. No processing was required for the study-specific long-COVID surveys and post-study survey.
CareTaker Medical physiologic recordings: Participant systolic, diastolic, and heart rate samples were averaged for each recording session. Raw ECG data were processed offline using Mindware Technology’s HRV Analysis 3.2.11 software (Mindware Technologies, Westerville, Ohio). Mindware’s automatic beat detection was complemented by visual ECG inspection to identify R-peaks and R-to-R interval irregularities (e.g. noise, outliers). Interval irregularities were corrected by averaging preceding and subsequent R-peaks. The interbeat interval (IBI) file was downloaded from Mindware as a Microsoft 365 Excel file Version 2205 Build 16.0.15225.20028 (Microsoft, Redmond, Washington) to allow for uploading into Kubios Premium 3.4.3 (Kubios Oy, Kuopio, Finland) for calculation of the root mean square of successive differences (RMSSD) between normal heartbeats.
The IBIs were also uploaded from Excel into the Physiological Time-Series Entropy Calculator (www.EntropyCalc.com) for the calculation of distribution entropy: embedding dimension 3, stretching factor 1, and bins 100. Distribution entropy is a non-linear method of evaluating HRV; meaning, the complexity of a living system leads to non-linearity and unpredictability within a time series.17,65,66 While there are several forms of entropy, distribution entropy has shown good reliability in shorter time recordings of less than 15 minutes, overcoming several of the limitations of other Kolmogorav entropy-based measures.65
Spirometry: There were inherent flaws with the data collection, including inconsistent effort on trials and the oversight of ensuring valid results during the collection process; therefore, no spirometry data was processed for this study.
Balance: For the Fukuda Stepping Test, the participants’ location at completion of their 50 steps were marked, and the displacement (distance traveled) and angle of rotation from their starting point were measured. Figure 2 illustrates a sample movement path (line C) and the angular displacement. The angle reported was the absolute value of angle AC so not the actual angle needed for analysis. Since the data was recorded as if on a clock, a conversion was done to get the actual angle the feet were facing from the orginal direction. The angle reported was based on degrees from the start. For example, 11:00 and 1:00 are both two half hour increments from the 12:00 time and were recorded as 30 degrees for both. This methodology was an approximation of the clock-face equivalent. No processing was required for the 1-leg standing test. Only the length of time on 1 foot or the maximum value of 2 minutes were recorded.
RESULTS
Study Recruitment and Population
Recruitment was initiated in March of 2021 through an initial email to the patient population of the chiropractic care study site (1,929 recipients), posting of the flyer on the study site website, and healthcare referrals. A follow-up email to study site patients was sent in May 2021, and beginning June 15, 2021, Facebook ads were funded and initiated.
Recruitment was slow. Between March of 2021 and August of 2021, 30 individuals indicated interest in the study through phone or email. Table 3 provides a breakdown of the study recruitment numbers. In July, a question was added to the phone survey that asked how the participants found out about the study. Most individuals who completed the phone survey and were asked the question (n = 12) reported that they found the study through Facebook ads (n = 8), with 4 participants reporting that they found out about the study through a friend or on a Facebook support group. Since the procedures in this study were being prototyped, the investigators decided to suspend recruitment in August of 2021, and the data from the 7 participants were analyzed.
Demographics for each participant are provided in Table 4. The average age of the participants was 46, and 5 of the 7 participants were female. Only one participant was admitted to the hospital with COVID-19 disease (5 days). All participants presenting with pain reported that their pain was either mostly or completely resolved by the end of care.
Clinic Integration of Study Protocols
Integrating the study protocol within a busy clinical practice presented several obstacles that had to be overcome. Scheduling was one of the primary challenges. The initial study protocol indicated that participants would receive care 2 to 3 times per week for up to 9 weeks. Due to life events and scheduling challenges, actual participant care and completion time was 1 to 2 times per week for up to 12 weeks. Complicating the scheduling process, measures such as HRV ideally needed to be conducted within a similar time frame for each assessment. To overcome this challenge, set days and times of the week were allocated to study-specific participant care and assessment, and set responsibilities were assigned to specific clinic staff. The clinician provided the initial intake review and exam, chiropractic care, and the post-exam. Study assessments were conducted by a clinic administrator trained to perform each assessment. Participant scheduling and any administrative follow-up were conducted by the clinic front-desk staff. Initially, participant phone screening was conducted by the collaborating research institution investigators; however, this added an additional communication layer between the participant and the clinic, so an amendment was approved by the Institutional Review Board transferring initial phone survey review to clinic front desk staff.
To aid in overall scheduling, the baseline assessment time point was considered in relation to how this date would impact scheduling throughout the study timeline. A discussion regarding the importance of scheduling and follow-through was conducted with each participant at the onset of the study. This discussion served as a secondary review of the Informed Consent procedures, seemed to assist with participant follow-through, and allowed those with more time constraints to withdraw early in the study process. Additional considerations included fundraising to offset clinician lost revenue, time allocated to analyzing and preparing data for evaluation by other investigators or a statistician, translating standard clinic reports to a de-identified form for sharing with collaborators, and time needed for study-related questions and technical support challenges.
Participant Self-Reports
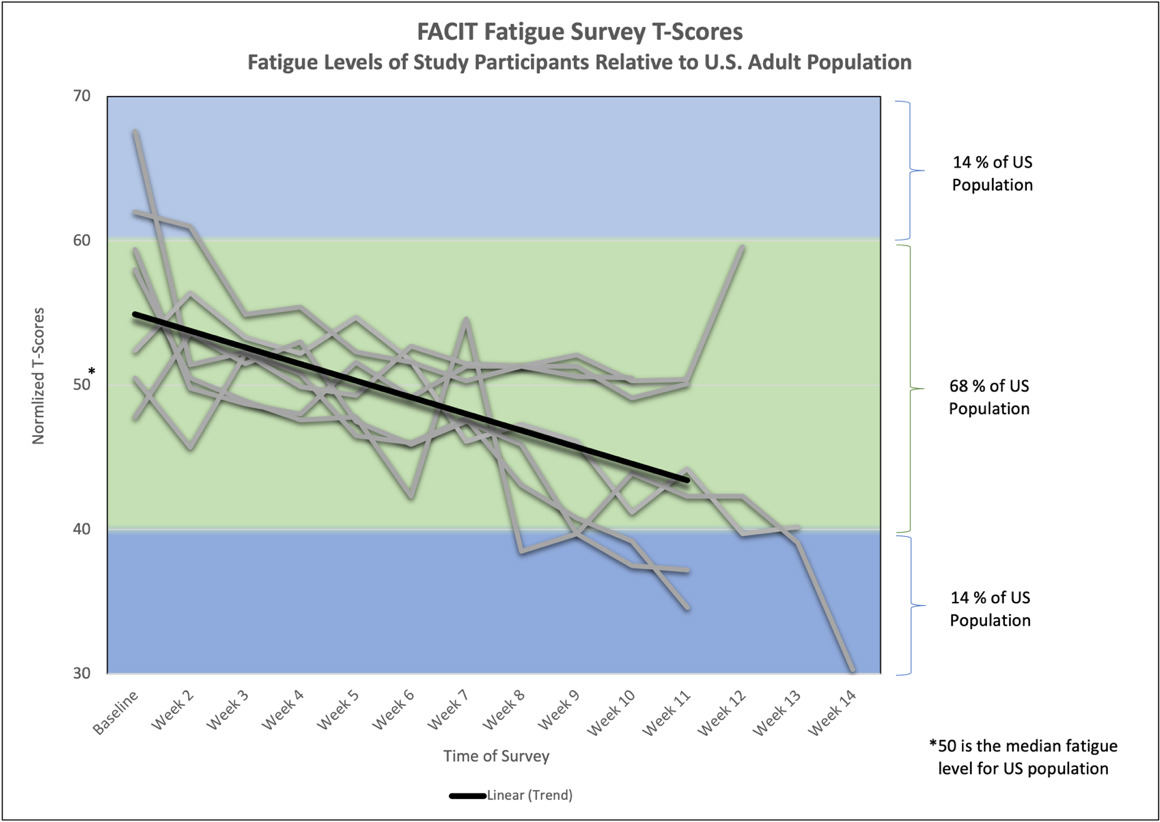
Functional Assessment of Chronic Illness Therapy–Fatigue Scale (FACIT-Fatigue Survey): Overall, participants reported improvement or complete resolution of self-reported symptoms. For the FACIT-Fatigue survey, scores were normalized to the United States (US) population, where 50 is the median fatigue level. Figure 3 shows 2 standard deviations on either side of the US normal fatigue level. At the beginning of the study the average FACIT-Fatigue T-score was at the 76th percentile level; meaning, the participants were on average more fatigued than 76% of the US population. By the end of the study participants on average were scoring in the 25th percentile; meaning, only 25% of the US population was less fatigued than the study participants.
The FACIT-Fatigue Figure 4 shows participants’ downward trends in T-Scores as well as the overall downward trendline. Participants started out at an average baseline score of 56.8, and after at least 15 ASM chiropractic sessions, participants reported an average score of 43.2.
Multidimensional Fatigue Symptom Inventory–Short Form (MFSI-SF): The secondary measure of fatigue, the MFSI-SF, demonstrated a similar trend in fatigue improvement as demonstrated in Figure 5. Overall, participants improved from baseline, with participant 114 as the only exception. She had been experiencing long-COVID symptoms since March of 2020 and adapted her daily routine to allow rest periods for the fatigue. At the end of the study, the participant reported that she was largely back to her pre-COVID routine, and did not require as much of an altered schedule to abate the fatigue. Her ability to balance her available energy is reflected as relatively low fatigue at baseline and at post on the MFSI-SF. Interestingly, her FACIT-Fatigue T-Scores improved from 52 to 40.
The FACIT-Fatigue survey was shorter and allowed for weekly tracking of the participants’ responses over the course of care, with the focus of the survey being fatigue and its impact upon daily activities and function. In contrast, the MFSI-SF was a 30-item survey that delineated health domains contributing to the fatigue. Table 5 and Figure 5 reflects the individual participant scores within the different contributing domains of the MFSI-SF.
Study-specific COVID-19 disease and long-COVID surveys: Study-specific assessments of the participants’ symptoms during active COVID-19 disease are represented in the Figure 6 heatmap. Figure 7 represents the progression in long-COVID symptom intensity for each participant at baseline and at conclusion of the study. The heatmaps’ individual squares represent the numerical severity for a symptom reported by a specific participant. Yellow hues indicate a more intense symptom experience, while darker green hues indicate less intense symptom experiences. The long-COVID symptoms of ear pain, sudden loss of body weight, and rash/spots on toes/feet are not shown on the heatmaps, as no participant listed these symptoms for the baseline or final symptom survey.
Figures 6 and 7 show that participants experienced several intense COVID-19 disease symptoms during their active COVID-19 disease and baseline long-COVID condition. Some of these symptoms had passed by the start of the long-COVID study, but many of the participants continued to experience some of the same symptoms as well as new ones in varying degrees of intensity during the study period. The final symptom assessment at the end of the study demonstrates improvement in nearly all participants across the spectrum of symptoms. Of note, Participant 115 had a cold on his last assessment day; this was represented as an increased number of symptoms on the final assessment survey, specifically respiratory based symptoms.
RAND 36-Item Health Survey (SF-36): Use of the SF-36 provided an opportunity to assess self-reported quality of life. Figure 8 shows the average SF-36 scores for each SF-36 domain. In each of the domains, scores increased–suggesting improvement–over the course of care.
Study-specific anonymous post-survey: As a prototype study, the opinions of study participants will help to inform future iterations of the research. Overwhelmingly, participants either agreed or strongly agreed that the study organization, processes, length, staff, knowledge, and overall experience was appropriate.
CareTaker Medical physiologic recordings
Average blood pressure (BP) and heart rate (HR) were recorded before and after a single session of chiropractic care at each of the assessment time points. Table 6 provides the individual participant CareTaker Medical physiologic responses. Heart rate generally dropped after a single chiropractic care session, though heart rate tended to increase in most participants over the course of the study.
For BP 3 of the participants had a baseline pre-chiropractic care systolic BP of less than 110 mmHg; for each of these participants, their systolic BP readings increased after the initial chiropractic care session. Over the course of care, only 1 of the 3 participants with initial systolic BP less than 110 mmHg maintained the increase in their systolic BP. The other 4 participants had a baseline pre-chiropractic care BP of greater than 130 mmHg. Three of the 4 participants experienced a drop in BP immediately after their first baseline, chiropractic care session, and the drop in BP was sustained over the course of care.
Five of the 7 participants showed an increase in RMSSD from baseline pre-chiropractic to baseline post chiropractic care. This result was mirrored in the Phase II pre- to post-chiropractic care results, in which 6 participants showed increased RMSSD and 1 participant showed no change in RMSSD. Pre-chiropractic care baseline to Phase III results showed a decrease in RMSSD for all participants; exempting participant 114, who showed an increase. For Distribution entropy (entropy), 4 of the 7 entropy scores for baseline pre- to post-chiropractic care increased, and Phase II pre- to post-chiropractic care entropy scores increased for all participants. Interestingly, Phase III pre- to post-chiropractic care showed 6 of the 7 participant entropy scores as decreased or unchanged. For the pre-chiropractic baseline to Phase III results, participants with a baseline entropy score equal to or less than 0.60 increased in entropy; participants with an entropy score greater than 0.60 demonstrated more variability in response.
Balance
Fukuda stepping test: From baseline assessment to Phase III assessment, 6 of the 7 participants decreased in distance traveled, and one participant’s score remained the same. The average distance traveled decreased during the Phase II and Phase III assessments; this result may be due to the over 100 cm travel distance recorded for three of the participants during the baseline or Phase I assessment sessions. (Figure 9) For absolute angle, no clear patterns were observed among the different assessment time points for the individual responses, and high absolute angle of rotation from start scores were also noted for a few participants in different assessment periods, influencing the average absolute angle value. (Figure 10)
One-leg standing test: For the 1-leg standing test, 4 of the 7 participants showed an increase in the length of time they could stand on their right leg from baseline to Phase III assessment time point, and one participant remained at the cap of 120 seconds. For the left leg, only 2 participants showed an increased time, and 2 participants remained at the cap of 120 seconds. Based on the average scores of the participants, the results demonstrate an initial increase between baseline and Phase I for both legs. For the right leg, an additional increase in sustained one-legged stance time is observed between Phase I and II. This increase is not observed in the left leg. With the small sample size, this may have been influenced by Participant 119’s drop in time from 120 seconds to only 29 seconds in Phase II. Averages for both the left and right leg decrease from the peak time at Phase III. (Figure 11)
DISCUSSION
Long-COVID is a complex condition that may not include a singular etiology2,15,18; this complicates the development of therapeutic interventions and research. While challenging, the 10-30% of individuals who experience protracted symptoms need a solution.2 Although traditional medicine and academic research serve as anchors in a metaphorical relay race to find reliable care methodologies, the baton can be shared with complementary and integrative medicine (CIM) providers, such as chiropractors. The present study was designed to prototype long-COVID study procedural steps, assessment methodologies, and participant response to care in a busy chiropractic practice.
One key aspect in the success of any research study is the recruitment of participants. Although several methods of recruitment were employed for this study, Facebook advertisements (ads) were the most successful method. Facebook ads were launched June 15, 2021 and were responsible for 4 of the 7 participants enrolled in the study. A study by Ellington et al reviewed the use of social media recruitment methods in the fields of nutrition, physical activity, and obesity, and although considerably cheaper per participant–$11.90 for social media vs. $214 for traditional methods–the rate of conversion from ad interaction to study enrollment was only 21.2%.67 The present study had a conversion rate of 57.1%. While this study only utilized Facebook ads, other social media advertising venues such as Instagram, Twitter, or Google may provide additional options for future research studies.67,68 The key for the present study was finding a way to connect specifically with long-COVID sufferers, and Facebook ads were the most successful method employed.
Once participants were recruited into the study, implementation of the study protocol and participant response to care could be evaluated. Based on feedback from the clinical team, scheduling and staffing were 2 key challenges to overcome. Due to external life factors and schedule coordination, patient care times extended beyond the initial estimate of 9 weeks to 12 weeks. This was complicated by the need to be mindful of circadian rhythms, which influence outcome measures such as Heart Rate Variability (HRV).69 The present prototype study suggests that it is feasible to implement a clinical study in a busy chiropractic clinic; however, study-specific task assignments for staff and clinicians, blocked time for participant care, and extended care plans are recommended for study success. Additional considerations include fundraising, data preparation time, study-related technical support challenges, and discussions with participants to ensure compliance.
Since follow-up assessments were distributed over 12 weeks of care, conversations with participants to remind them of assessment compliance requirements were crucial. For example, in addition to maintaining a similar assessment time window for HRV measurement, participants were asked to maintain consistent exercise, sleep, medication, and caffeine consumption for each assessment time point.70 Pre-appointment phone calls helped prevent rescheduling due to lack of participant compliance. Once participants were in the clinic, most surveys and assessments were tolerated and successfully performed by the participants, exempting spirometry. Whether technician, equipment, or participant-related, the effect of complications in spirometry acquisition were poor data quality and inconsistent effort within the trials. Challenges related to spirometry performance were not unique to this trial.71 An editorial in the Primary Care Respiratory Journal highlighted the difficulties of incorporating spirometry in a primary care setting.71 In addition to advocating the development of advanced training programs for the administration and review of spirometry results, the article suggests referrals to local respiratory centers and visiting spirometry teams as possible solutions.71 Since the ability to walk without becoming breathless is a concern for long-COVID suffers, a proposed solution to the challenges of spirometry is the 6-minute walk test.2–5 The 6-minute walk test (6MWT) is a simple test of patient functional status that does not require exercise equipment or advanced training.72 In long-COVID sufferers, the 6MWT test has been used to show changes over time, and 6MWT performance has been associated with patient dyspnea and hypoxia levels.73,74
Respiratory symptoms, such as shortness of breath (dyspnea), chest tightness, or difficulty breathing, were reported by 6 of the 7 participants, and nearly all symptoms improved or completely resolved by the end of the study period. Two participants (115 and 119) contracted a non-COVID virus at the end of care and presented with very slight respiratory symptoms at the final assessment. In addition to the changes in respiratory symptoms, participants reported improvement or complete resolution of self-reported symptoms across the spectrum of long-COVID symptoms. SF-36 results were similar to MFSI-SF domain results, with both assessments reflecting pronounced improvement, especially following the initial phase of care. Fatigue, one of the main long-COVID complaints,2,3 improved for all participants. The FACIT-Fatigue T-scores showed that participants transitioned from being in the 76th percentile to the 25th percentile on average; meaning, the participants changed from being on average more fatigued than 76% of the population to being more fatigued than only 25% of the US population.
Having the FACIT-fatigue assessed weekly and the MFSI assessed at the follow-up time points provided greater insight into each participant’s symptoms. Each participant presents with their own unique set of life circumstances, so the self-reports and the small size of the present study allowed the authors to understand the potential context behind some of the participant results. The ability to connect changes in respiratory symptoms to onset of a non-COVID virus, personal adaptations to fatigue, return to work, or increased levels of stress due to the loss of a job helped with interpreting prototype results, allowing for adaptations in study design for future research. Two participants–119 and 114–showed a slight increase or no change in 1 of the 2 fatigue surveys. Participant 119 was one participant who contracted a viral infection at the end of the study. Participant 114 had been experiencing long-COVID symptoms for over a year and was therefore accomplished at adapting her routine to account for her long-COVID fatigue. At the end of the study, Participant 114 was able to accomplish more in her daily life. Even so, her reported fatigue was unchanged on the MFSI-SF, although, her score did improve on the FACIT-Fatigue.
In addition to patient-reported outcomes, this study incorporated physiology and balance. The results of these objective assessments were mixed. For heart rate (HR), heart rate variability (HRV), and blood pressure (BP), the results reflect the chiropractic literature, in which some studies demonstrate an increase in the values immediately post-care and over time, while other studies show no change or a decrease in the values immediately post-care and over time.30–32,37,75–83 Examining the results of the present study for trends, a baseline, pre-chiropractic care systolic BP less than 110 mmHg was observed in 3 individuals; for each of these participants systolic recordings increased after the initial chiropractic care session. The other 4 participants had a baseline pre-chiropractic care BP of greater than 130 mmHg. Three of the 4 participants with a systolic BP of greater than 130 mmHg experienced a drop in BP immediately after their first chiropractic care session. These results were similar to the results of a pre-, immediate, and post-chiropractic care study by Torns.76 The Torns study demonstrated a significant increase in systolic BP for hypotensive participants and a significant decrease in systolic BP in normotensive, prehypertensive, and hypertensive participants. Although only 4 of the 7 participants in the present study maintained their directional systolic BP changes over the course of care (1 of the 3 participants with an initial systolic BP less than 110 mmHg maintained the increase, while 3 of the 4 with an initial systolic BP of greater than 130 maintained the decrease) the unique baseline-related responses suggests that a systolic BP phenotype should be considered in future study development and analysis.
The HRV results, which were incorporated to provide a window into the autonomic function of the participants exhibited some similarities to the BP results. Most participants exhibited an increase in RMSSD from baseline to immediate post-chiropractic care for baseline and Phase II care; however, the overall response for participants was a decline in RMSSD from baseline to Phase III care. For distribution entropy, which represents the degree of complexity within a non-linear system, the pre-chiropractic baseline to Phase III results showed a trend associated with baseline presentation. Participants with a baseline entropy score equal to or less than 0.60 increased in entropy; participants with an entropy score greater than 0.60 demonstrated more variability in their responses. The variation in responses to care reflecting the existing chiropractic literature–and the response to care trends associated with baseline scores for both BP and HRV–provide some preliminary indication that assessment of physiologic function could provide value in future iterations of chiropractic clinical research on long-COVID.30–32,37,75–83
As a protocol development study, there were several limitations. Given the small sample size, inference related to phenotypes and care response was limited. All but one of the participants also reported pain-based symptoms that resolved or nearly resolved over the course of care. The COVID-19 pandemic has been associated with new onset of chronic pain conditions and increases in existing chronic pain levels.84 According to a review by Shanthanna et al, sympathetic overactivity, dysregulation of neural activity, and inflammatory immune mediators may be potential mechanisms associated with changes in chronic pain responses.84 While the exact mechanisms associated with observed chiropractic-related improvement of pain are not known, chiropractic is a non-drug therapy recommended for the resolution of pain, especially musculoskeletal pain.81 The mechanisms proposed by Shanthanna et al. related to long-COVID chronic pain are similar to those suggested by other researchers as mechanisms for long-COVID symptoms in general, namely autonomic dysregulation and inflammation.2,84,85
An additional limitation was the lack of validated self-reports related to the participants’ mental health and stress. Using the self-report specifically designed for the present study, participants reported improvements in anxiety, depression, concentration, and mental focus. To address complaints of anxiety and depression, future studies should include validated participant self-reports such as the Depression Anxiety Stress Scales (DASS).86 Depression, anxiety, and post-traumatic stress disorder (PTSD) may present as either effects or risk factors associated with long-COVID.87 To assess cognitive function, the addition of open-access cognitive tests such as those developed as part of the NIH Toolbox could be integrated into the study protocol (https://www.healthmeasures.net/). These assessments have been used in past long-COVID research studies, with results indicating poorer performance in cognitive domains such as working memory and attention.88 Finally, physiologic assessment measures such as heart rate variability can be influenced by an individual’s level of stress.70 Several of the participants in this study experienced varying degrees of stress during the 12 weeks of care. The small sample size did allow the clinicians an opportunity to gain greater insight into their associated mental or physical stressors; however, the addition of self-reported stress measures might provide additional context to the results.
CONCLUSION
The purpose of the present study was to prototype a long-COVID research protocol within a practice-based setting, testing procedural steps, outcome measures, and patient response to care. The results of the study suggest that similar research would be feasible; however, investigators need to account for challenges in recruitment, staffing, and scheduling. Participant self-reports and basic physiologic measures of cardiovascular function and balance were successfully implemented. Participants reported improvement and often resolution of long-COVID symptoms and pain, and physiologic marker responses to care were consistent with previous chiropractic research. The study design and small sample size limit response to care generalizability, and the authors recommend findings be confirmed with properly powered clinical trial design.
ACKNOWLEDGEMENTS
We would like to acknowledge the considerable generosity of our donors. Direct support for the present study was provided through generous philanthropic leadership by the Gray Family, with additional support from Jay Grossman. Early support for the development of an Axial Stability Method Chiropractic research program within Lydian Chiropractic clinic was provided by the Zebrin Foundation.
The authors would also like to acknowledge the assistance with study scheduling by Noha Azzi Ranson and data preparation provided by Austin Garlinghouse which were beneficial to the study implementation and manuscript preparation, respectively.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.

_and_the_angular_displacement_measured_for_the_fukuda_stepp.jpeg)









_and_the_angular_displacement_measured_for_the_fukuda_stepp.jpeg)